Abstract
Purpose
To determine the correlations of intraocular pressure (IOP) with risk factors in rhegmatogenous retinal detachment (RRD) patients.
Methods
A total of 113 eyes in 113 consecutive patients with RRD were enrolled in this study. IOP was measured using applanation tonometry at the initial visit. Based on the difference in IOP between the affected and unaffected eyes, the subjects were divided into two groups: group 1 (IOP difference ≤ 2 mmHg) and group 2 (IOP difference > 2 mmHg). Correlations between the IOP and RRD morphology, visual acuity (VA), best-corrected VA (BCVA), retinal break size and location, range of retinal detachment, macular involvement, and proliferative vitreoretinopathy were analyzed.
Results
The IOP at the initial visit was 12.88 ± 3.2 mmHg in the affected eyes and 14.27 ± 2.5 mmHg in the unaffected eyes. The IOP difference between the affected and unaffected eyes was −1.40 ± 2.82 mmHg. The BCVA and range of retinal detachment showed statistically significant differences between groups 1 and 2.
Figures and Tables
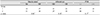
 | Figure 1Detachment chart. Outer circle represents ora serrata and inner circle represents equator of the globe. Each 12 perpendicular black line indicates 30 degrees. Using the blue lines which indicates 45 degrees, we describe the extent of detachment in 8 regions (superior, superotemporal, temporal, inferotemporal, inferior, inferonasal, nasal, superonasal). |
 | Figure 2Distribution of the largest retinal tear position. Group 1, the total of 52 eyes were involved. Group 2, the total of 61 eyes were involved. The difference of distribution between the two groups was not statistically significant (p = 0.626, chi square test). |
Table 1
Baseline demographics and clinical characteristics of the study subjects

Values are presented as mean ± standard deviation unless otherwise indicated.
LogMAR = the logarithm of the minimal angle resolution; VA = visual acuity; BCVA = best corrected visual acuity; IOP = intraocular pressure; DD = disc diameter.
*Student t-test; †chi-square test; ‡significant difference between groups.
References
1. Mitry D, Charteris DG, Yorston D, et al. The epidemiology and socioeconomic associations of retinal detachment in scotland: a two-year prospective population-based study. Invest Ophthalmol Vis Sci. 2010; 51:4963–4968.

2. Algvere PV, Jahnberg P, Textorius O. The Swedish retinal detachment register. I. A database for epidemiological and clinical studies. Graefes Arch Clin Exp Ophthalmol. 1999; 237:137–144.
3. Beijing Rhegmatogenous Retinal Detachment Study Group. Incidence and epidemiological characteristics of rhegmatogenous retinal detachment in Beijing, China. Ophthalmology. 2003; 110:2413–2417.
4. Sasaki K, Ideta H, Yonemoto J, et al. Epidemiologic characteristics of rhegmatogenous retinal detachment in Kumamoto, Japan. Graefes Arch Clin Exp Ophthalmol. 1995; 233:772–776.
5. Dobbie JG. A study of the intraocular fluid dynamics in retinal detachment. Arch Ophthalmol. 1963; 69:159–164.

6. Solberg T, Ytrehus T, Ringvold A. Hypotony and retinal detachment. Acta Ophthalmol (Copenh). 1986; 64:26–32.

8. Netland PA, Mukai S, Covington HI. Elevated intraocular pressure secondary to rhegmatogenous retinal detachment. Surv Ophthalmol. 1994; 39:234–240.

9. Burton TC, Arafat NI, Phelps CD. Intraocular pressure in retinal detachment. Int Ophthalmol. 1979; 1:147–152.

10. Regan CDJ, Rousseau AP. The intraocular dynamics of eyes with retinal detachment. Am J Ophthalmol. 1966; 61:696–702.

11. Leydhecker W, Akiyama K, Neumann HG. Intraocular pressure in normal human eyes. Klin Monbl Augenheilkd Augenarztl Fortbild. 1958; 133:662–670.
12. Kim CS, Seong GJ, Lee NH, Song KC. Prevalence of primary open-angle glaucoma in central South Korea the namil study. Ophthalmology. 2011; 118:1024–1030.
13. Davanger M. The difference in ocular pressure in the two eyes of the same person: in individuals with healty eyes and in patients with glaucoma simplex. Acta Ophthalmol (Copenh). 1965; 43:299–313.
14. Huerkamp B, Behme H. Intraocular tension, especially glaucoma in retinal detachment with tear in the ora retinae. Albrecht Von Graefes Arch Ophthalmol. 1955; 156:433–442.
15. Syed Z, Stewart MW. Age-dependent vitreous separation from the macula in a clinic population. Clin Ophthalmol. 2016; 10:1237–1243.

16. Wickham L, Bunce C, Wong D, Charteris DG. Retinal detachment repair by vitrectomy: simplified formulae to estimate the risk of failure. Br J Ophthalmol. 2011; 95:1239–1244.

17. Pastor JC, Rojas J, Pastor-Idoate S, et al. Proliferative vitreoretinopathy: a new concept of disease pathogenesis and practical consequences. Prog Retin Eye Res. 2016; 51:125–155.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download