Abstract
Purpose
We explored the utility of ultra-wide fundus photography (UFP) to evaluate patients with blunt ocular trauma who visited our emergency room.
Methods
We retrospectively reviewed the records of 162 patients with blunt ocular trauma who visited the emergency room between June 2015 and December 2016. The patients were divided into two groups: those who underwent UFP and those who did not. We reviewed all medical records and took photographs to illustrate trauma-related retinal problems, and compared the two groups.
Results
Ninety-two eyes underwent UFP and 70 eyes did not. In the latter group, commotio retinae was detected in 17 eyes (24%), Berlin's edema in seven (10%), and retinal hemorrhage in three (4%). In the former group, commotio retinae was detected in 45 eyes (49%), Berlin's edema in 10 (11%), and retinal hemorrhage in 10 (11%). Retinal breaks were evident in only two eyes (2%). The frequency of commotio retinae significantly differed between the two groups.
Figures and Tables
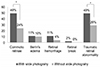 | Figure 1Retinal findings in eyes with blunt ocular trauma. Commotio retinae in 17 eyes (24%), Beriln's edema in seven eyes (10%), retinal hemorrhage in three eyes (4%) were detected and retinal breaks were not detected in group without wide fundus photography. Commotio retinae in 45 eyes (49%), Beriln's edema in 10 eyes (11%), retinal hemorrhage in 10 eyes (11%) and retinal breaks in two eyes (2%) were detected in group with wide angle fundus photography (*p < 0.05). |
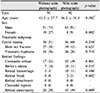
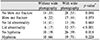
 | Figure 2Facial photography (A), traditional fundus photography (B), and ultra-wide fundus photography (C) in a 69-year-old woman with ocular blunt trauma due to slip down. Left eyelid swelling with abrasion were shown and blow-out fracture (medial orbital wall) was found in orbital computed tomography. Ultra-Wide fundus photography show commotio retinae (yellow arrowheads) and retinal hemorrhage (red arrowhead) more prominently than conventional fundus photographs. |
Table 1
The demographics and the comparison of the two groups; patients who underwent ultra-wide fundus photography (with wide photography) and patients who underwent examinations without ultra-wide fundus photography (without wide photography)
References
1. Song MH, Kim JW, Chung SK. The statistical observation of ocular injury. J Korean Ophthalmol Soc. 2009; 50:580–587.

2. Han YS, Shyn KH. A statistical observation of the ocular injuries. J Korean Ophthalmol Soc. 2005; 46:117–124.
3. Neubauer AS, Kernt M, Haritoglou C, et al. Nonmydriatic screening for diabetic retinopathy by ultra-widefield scanning laser ophthalmoscopy (Optomap). Graefes Arch Clin Exp Ophthalmol. 2008; 246:229–235.

4. Lee DH, Kim SS, Kim M, Koh HJ. Identifiable peripheral retinal lesions using ultra-wide field scanning laser ophthalmoscope and its usefulness in myopic patients. J Korean Ophthalmol Soc. 2014; 55:1814–1820.
5. Silva PS, Cavallerano JD, Sun JK, et al. Nonmydriatic ultrawide field retinal imaging compared with dilated standard 7-field 35-mm photography and retinal specialist examination for evaluation of diabetic retinopathy. Am J Ophthalmol. 2012; 154:549–559.e2.

6. Mackenzie PJ, Russell M, Ma PE, et al. Sensitivity and specificity of the optos optomap for detecting peripheral retinal lesions. Retina. 2007; 27:1119–1124.

7. Mudvari SS, Virasch VV, Singa RM, MacCumber MW. Ultra-wide-field imaging for cytomegalovirus retinitis. Ophthalmic Surg Lasers Imaging. 2010; 41:311–315.

8. Khandhadia S, Madhusudhana KC, Kostakou A, et al. Use of Optomap for retinal screening within an eye casualty setting. Br J Ophthalmol. 2009; 93:52–55.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download