Abstract
Purpose
To determine possible differences in dry eye syndrome in relation to surgery methods, especially between small incision lenticule extraction (SMILE) and femtosecond laser-assisted laser in situ keratomileusis (FS-LASIK), in Korean patients.
Methods
This study involved 20 patients (20 eyes) who were treated with SMILE surgery and 23 patients (23 eyes) who were treated with FS-LASIK. The Schirmer test, tear film breakup time (TBUT), corneal staining score (CSS), and measurement of changes in the lipid layer thicknesses at one week, and 1 and 3 months after surgery were performed. Possible correlations between indicators of dry eye syndrome were then analyzed.
Results
There was a significant time difference in some indices. The TBUT was 5.52 ± 1.50 s after one week for SMILE patients and 4.59 ± 2.50 s for FS-LASIK patients (p = 0.02). The CSS was 0.50 ± 0.51 after 1 week for SMILE patients and 1.14 ± 0.99 after 1 week for FS-LASIK patients (p = 0.04). The CSS was 0.50 ± 0.51 after 1 month for SMILE patients and 1.10 ± 0.93 after 1 month for FS-LASIK patients (p = 0.03). Three months later, the CSS was 0.39 ± 0.50 for SMILE patients and 0.94 ± 0.85 for FS-LASIK patients (p = 0.03). However, the Schirmer test did not show a significant difference postoperatively for SMILE and FS-LASIK patients at 1 week (p = 0.44), 1 month (p = 0.68), and 3 months (p = 0.23). Additionally, the thickness of the tear film lipid layer did not show a significant difference during the same periods (p = 0.36, p = 0.43, and p = 0.72, respectively).
Figures and Tables
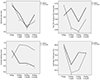 | Figure 1Ocular surface parameters after SMILE and FS-LASIK. Ocular surface parameters including Schirmer test, tear break-up time, corneal staining score, lipid layer thickness were compared between patients undergoing SMILE and FS-LASIK. SMILE = small incision lenticule extraction; FS-LASIK = femtosecond laser assisted in situ keratomileusis. *p < 0.05 in SMILE, **p < 0.05 in FS-LASIK. |
Table 2
Preoperative, 1 week, 1 month, and 3 months after refractive surgery

Values are presented as mean ± standard deviation unless otherwise indicated.
SMT = schirmer test; SMILE = small incision lenticule extraction; FS-LASIK = femtosecond laser-assisted in situ keratomileusis; TBUT = tear film breakup time; CSS = corneal staining score; LLT = lipid layer thickness.
*Wilcoxon signed-rank test; †pair t-test; ‡Mann-Whitney U test; §Student's t-test.
References
1. Zhang Y, Shen Q, Jia Y, et al. Clinical outcomes of SMILE and FS-LASIK used to treat myopia: a meta-analysis. J Refract Surg. 2016; 32:256–265.

2. Shen Z, Shi K, Yu Y, et al. Small incision lenticule extraction (SMILE) versus femtosecond laser-assisted in situ keratomileusis (FS-LASIK) for myopia: a systematic review and meta-analysis. PLoS One. 2016; 11:e0158176.

3. Kobashi H, Kamiya K, Shimizu K. Dry eye after small incision lenticule extraction and femtosecond laser-assisted LASIK: meta-analysis. Cornea. 2017; 36:85–91.
4. Shah R, Shah S, Sengupta S. Results of small incision lenticule extraction: all-in-one femtosecond laser refractive surgery. J Cataract Refract Surg. 2011; 37:127–137.

5. Xie W. Recent advances in laser in situ keratomileusis-associated dry eye. Clin Exp Optom. 2016; 99:107–112.

6. Denoyer A, Landman E, Trinh L, et al. Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology. 2015; 122:669–676.
7. Bron AJ. The Doyne Lecture. Reflections on the tears. Eye (Lond). 1997; 11(Pt 5):583–602.
8. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003; 22:640–650.

9. De Paiva CS, Chen Z, Koch DD, et al. The incidence and risk factors for developing dry eye after myopic LASIK. Am J Ophthalmol. 2006; 141:438–445.

11. Tomlinson A, Bron AJ, Korb DR, et al. The international workshop on meibomian gland dysfunction: report of the diagnosis subcommittee. Invest Ophthalmol Vis Sci. 2011; 52:2006–2049.

12. Li M, Zhao J, Shen Y, et al. Comparison of dry eye and corneal sensitivity between small incision lenticule extraction and femtosecond LASIK for myopia. PLoS One. 2013; 8:e77797.

13. Demirok A, Ozgurhan EB, Agca A, et al. Corneal sensation after corneal refractive surgery with small incision lenticule extraction. Optom Vis Sci. 2013; 90:1040–1047.

14. Wang B, Naidu RK, Chu R, et al. Dry eye disease following refractive surgery: a 12-month follow-up of SMILE versus FS-LASIK in high myopia. J Ophthalmol. 2015; 2015:132417.

15. Pflugfelder SC, Tseng SC, Sanabria O, et al. Evaluation of subjective assessments and objective diagnostic tests for diagnosing tear-film disorders known to cause ocular irritation. Cornea. 1998; 17:38–56.

16. Kojima T, Ishida R, Dogru M, et al. A new noninvasive tear stability analysis system for the assessment of dry eyes. Invest Ophthalmol Vis Sci. 2004; 45:1369–1374.

17. Maurice D. The Charles Prentice award lecture 1989: the physiology of tears. Optom Vis Sci. 1990; 67:391–399.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download