Introduction
Among the countries in the Organization for Economic Cooperation and Development, South Korea has indicated a relatively low oral contraceptive usage rate of 3% and a high artificial abortion rate [
12]. Although artificial abortion is legally prohibited in Korea, 26% of married women have undergone artificial abortion. Among unmarried women, 7% experienced pregnancy and 91% of the women who had experienced pregnancy underwent artificial abortion [
3]. It should be noted that the contraceptive practice rate among sexually active middle and high school students is as low as 39% [
4]. On the other hand, the abuse of emergency contraceptive pills (ECPs), involving the intake of the pill more than twice a month, increased by 2.3 times from 2012 to 2015 and by 2.5 times in teenagers over the course of 3 years [
5]. This indicates that ECP abuse without regular contraception is still an issue of concern in South Korea.
The availability of ECP as either over-the-counter/behind-the-counter (BTC) or as a prescription drug has been one of the most controversial issues in South Korea. While most of the oral contraceptives are classified as BTC, all ECP single agents have been classified as prescription-only products since their first introduction in South Korea in 2001. Since then, despite attempts to reclassify the ECP to BTC, it is still available through prescription-only in South Korea, owing to strong religious and social reasons as well as medical opinion against the reclassification. Conflicting opinions have been issued regarding the need for a prescription to obtain ECP. The Korean Association of Obstetricians & Gynecologists opposed the reclassification of ECP stating that regular contraception would be less favored if ECP was to be converted to a BTC drug, as the contraceptive usage rate of Koreans is already low [
6].
However, there have been no studies that directly investigated individual physicians for their opinions on the reclassification of ECP. Therefore, this study investigated the attitude of Korean physicians regarding women's access to ECPs and the reclassification of ECP to a BTC drug.
Results
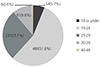
Each month, Korean physicians prescribed ECP to an average of 14.9±23.9 women during the past year (between December 2013 and November 2014
). The number of women who were prescribed for ECP was highest among the 19–24 age group (51.6%), followed by the 25–29 (25.1%), the 30–39 (9.6%), and the 40–49 (0.6%) age groups. Women under the age of 18 constituted 5.7% (
Fig. 1).
Fig. 1
Age group of women with the most frequent emergency contraceptive pill prescription rate (n=946).
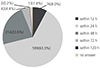
In terms of the duration following sexual intercourse until the visit to the clinic or hospital for ECP prescription, 63.3% of physicians answered that it was within 24 hours and 97% of physicians replied that it was within 72 hours (
Fig. 2).
Fig. 2
Time lapse between sexual intercourse and emergency contraceptive pill prescription (n=946).
The most commonly prescribed emergency contraceptive method by the physicians surveyed was levonorgestrel (LNG) alone, accounting for 66% of all prescriptions, followed by ulipristal acetate (UPA; 30.0%). The Yuzpe method and copper intrauterine device were most frequently prescribed by 2.1% and 0.2% of physicians, respectively.
1. Physicians' awareness of ECP access among women and barriers limiting women's access
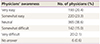
Twenty-point four percent of physicians reported that it was very easy for women to access ECP, and 23.3% of physicians stated that it was somewhat easy. However, 15.0% and 2.1% of physicians responded that it was somewhat difficult or very difficult to obtain ECP, respectively (
Table 1). Regarding the barriers limiting women's access to ECP, 24.8% of physicians stated that women lacked information about ECP and 22.5% of physicians answered that women were likely to be emotionally burdened by a visit to a clinic or hospital to obtain ECP prescription. Another 12.2% of physicians responded that women were concerned about the recording of their sexual privacy (
Table 2). A request for ECP prescription without recording personal information was made by patients to 51% of the physicians.
Table 1
Physicians' awareness of emergency contraceptive pill access among women (n=946)
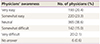
|
Physicians' awareness |
No. of physicians (%) |
|
Very easy |
193 (20.4) |
|
Somewhat easy |
220 (23.3) |
|
Neutral |
365 (38.6) |
|
Somewhat difficult |
142 (15.0) |
|
Very difficult |
20 (2.1) |
|
No answer |
6 (0.6) |
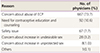
Table 2
Barriers limiting women's access to emergency contraceptive pill (n=946)
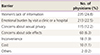
|
Barrier |
No. of physicians (%) |
|
Women's lack of information |
235 (24.8) |
|
Emotional burden by visit a clinic or a hospital |
213 (22.5) |
|
Concerns about sexual privacy |
115 (12.2) |
|
Concerns about side effects |
60 (6.3) |
|
Inconvenience |
18 (1.9) |
|
Cost |
10 (1.1) |
|
Others |
2 (0.2) |
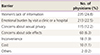
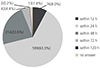
2. Physician's opinions about the switch of ECP from a prescription to a BTC drug
Our survey indicated that 92% of physicians preferred to maintain ECP as a prescription drug while 6.1% desired a switch to a BTC drug. The reasons why physicians opposed the switch of ECP to a BTC drug were because of concerns about its potential abuse (76.7%), followed by the need for contraceptive education and counseling (10.6%), safety issues (7.7%), concerns about an increase in undesirable sexual practices (3.2%), and concerns about an increase in unprotected sex (0.98%) (
Table 3). Conversely, among the physicians who preferred the reclassification of ECP to a BTC drug, the most common reasons were women’s rights to choose contraception (55.2%), followed by easy access to ECPs (19.0%), minimal side effects (8.6%), decrease in medical expenses (6.9%), reduced risk of unwanted pregnancies (6.9%), and protection of sexual privacy (1.7%).
Table 3
The reasons for opposing the switch of emergency contraceptive pill (ECP) to a behind-the-counter drug (n=870)
|
Reason |
No. of physicians (%) |
|
Concern about abuse of ECP |
667 (73.7) |
|
Need for contraceptive education and counseling |
92 (10.6) |
|
Safety issue |
67 (7.7) |
|
Concern about increase in undesirable sex |
28 (3.2) |
|
Concern about increase in unprotected sex |
8 (1.0) |
|
Others |
1 (0.1) |
3. Prevention of ECP abuse
The abuse of ECP is defined by the regular use of ECPs each time women engaged in unprotected sex instead of regular contraception.
In order to prevent ECP abuse, physicians believed that the most important factors to be considered were education on contraception (79.0%), restriction of repetitive prescriptions within the same menstrual cycle (7.7%), improved accessibility (5.3%), and a price increase of ECP (0.7%) (
Table 4).
Table 4
Most important factors for prevention of emergency contraceptive pill abuse

|
Factor |
No. of physicians (%) |
|
Contraceptive education |
747 (79.0) |
|
Restriction of repetitive prescription within the same menstrual cycle |
73 (7.7) |
|
Improved accessibility |
50 (5.3) |
|
Price increase |
7 (0.7) |
|
Others |
2 (0.2) |
|
No answer |
67 (7.1) |
Discussion
Emergency contraception refers to the use of drugs or copper intrauterine devices to prevent pregnancy shortly after unprotected intercourse [
8]. Several interventions have been developed for emergency contraception and their effectiveness as well as safety are well known [
91011]. LNG only and UPA pills are available over- or behind-the counter without a prescription in a significant number of countries, based on their relative safety profile and evidence suggesting their role in effectively delaying ovulation [
12]. However, ECPs are only available through prescription in South Korea. In August 2012, the Korean Ministry of Food and Drug Safety attempted to repeal an existing policy and reclassify ECP to approve ECP's BTC availability; however, the ministry abandoned the reclassification following an intense debate among the groups involved [
13]. The Korean Association of Obstetricians and Gynecologists also opposed the switch to BTC [
6]. However, no reported survey of Korean physicians, including individual gynecologists, was available.
The results of this study showed that almost every physician prescribed ECP within 72 hours following unprotected intercourse and LNG was the most commonly prescribed emergency contraception method by Korean physicians. This finding is in contrast to the report indicating that two-thirds of all ECPs sold in Germany were UPA since the availability of ECP as a BTC drug in March 2015 [
14]. A majority (92%) of Korean physicians preferred to maintain ECP as a prescription drug to prevent its potential abuse and to promote counseling and education for regular contraception. The Korean Association of Obstetricians and Gynecologists also currently recommends that ECP should be converted to BTC only after Korean women are educated on contraceptive usage because the rate of oral contraceptive consumption is relatively low in Korean women. In fact, despite the fact that oral contraceptive usage among Korean women has steadily increased from 2.1% in 2010 to 2.8% in 2014, it is still relatively low compared with the UK (21.6%), Canada (16.3%), Belgium (38.8%), Australia (19.9%), and USA (13.4%) [
15]. The rate of oral contraceptive pill use in Korean women is similar to that of Japanese (2.3%), Malaysian (2.7%), and Indonesian women (2.7%) [
16]. Japan and Indonesia still classify ECPs as a prescription drug [
17], similar to Korea.
In a study of contraceptive practices involving Korean middle and high school adolescents, only 20–26% of the students who had engaged in sexual intercourse replied that they always practice contraception. On the other hand, 45–49% reported that they never used contraception at all [
18]. In another report on contraception in Korean youth, Korean teenagers were most unlikely to use contraceptives, while contraceptive users were most likely to use condoms and only 3–4% of adolescents reported taking oral contraceptives. Among unmarried, sexually active young adults aged 20 and above, 13.4% of men and 6.7% of women experienced pregnancy. Of these individuals who had experienced pregnancy, 72.7% of men and 100% of women selected artificial abortion [
19]. In a survey of 15- to 18-year-old girls who were exposed to oral contraceptives in South Korea, majority of them had been taught about condom usage but were ignorant about oral contraceptives and other contraceptive practices. They were not well informed about the options and methods of oral contraceptives and ECP, and often had false medical knowledge about oral contraceptives and ECP [
20]. The rate of ECP use among adolescents was 0.98–1.3%, which was much lower than condom use (36.7%), withdrawal (8.3%), and rhythm (2.6%).
Korean physicians responded that contraceptive education (79.0%) was the most important factor to be considered to prevent the abuse of ECP, followed by restriction of repetitive prescriptions within the same menstrual cycle (7.7%).
Lack of information was the most common barrier restricting women's access to ECP. A survey of Korean women's awareness of ECPs found that Korean women, in spite of taking ECPs, were worried that ECPs induced serious side effects and were associated with fetal anomalies following pregnancy [
21]. This suggests a negative and false perception about the safety of ECP and lack of information on the part of Korean women.
In addition to insufficient information, 22.5% of physicians recognized that there was a psychological issue with regards to women visiting clinics or hospitals to obtain ECP prescriptions. The fact that 51% of physicians had been asked to prescribe ECP without recording personal information, underscores the need for a policy to further improve ECP access in Korea. The fact that the survey indicates that 17% of physicians found ECP access difficult, suggests the need for greater and improved access.
This study suggests a need for practical and active education on contraception among youth and adults in Korea. The education is required to enhance proper awareness of regular and emergency contraception. Additionally, efforts are needed to ensure that women with accurate information on contraception can easily access ECP.
To the best of our knowledge, this is the first survey that evaluated the Korean physicians' attitude toward ECP regarding women's access and reclassification of ECP.
The study's limitation relates to its non-representative character in that the survey cannot be generalized to the entire physician community in South Korea, although it was conducted among approximately 1,000 physicians. Furthermore, since most of the subjects were obstetricians and gynecologists (74.4%), it does not represent the opinion of other physicians. It is necessary to survey the broader physician population given that 37% of ECPs were prescribed by physicians who were not obstetricians or gynecologists [
22]. Second, physicians' opinions about access and barriers to ECPs may differ from those of women in need of ECPs. Further studies are needed to identify the gaps between physicians and women. These efforts are expected to lower the barriers among women in need of contraception.
In conclusion, most Korean physicians opposed the reclassification of ECP to a BTC drug, due to their belief in increasing the role of educational initiatives about contraception and contraceptive practices, before improving the access to ECP. Physicians stated that insufficient information about ECP and the emotional burden among women visiting clinics or hospitals acted as the biggest barriers in promoting access to ECP among women. This study suggests that contraceptive education for youth and adults in Korea should be more realistic and active, with an emphasis on regular contraception. Furthermore, efforts are needed to ensure accuracy of information on contraception, to facilitate women's access to ECP.
The majority of physicians were of the opinion that ECP should remain as a prescription drug because of concerns about its potential abuse. Before the reclassification, contraceptive education for youth and adults should be more realistic and active, with an emphasis on the importance of regular contraception. Furthermore, efforts are needed to ensure that women with accurate information can access ECPs conveniently without privacy concerns.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download