This article has been
cited by other articles in ScienceCentral.
Dear Editor:
Primary cutaneous mucinous carcinoma (PCMC) is a rare malignant tumor which usually appears on the periocular region and mimics metastatic skin carcinoma
12. We have encountered a case of PCMC that appeared on the abdomen.
A 72-year-old male presented with an asymptomatic nodular lesion on his right lower abdomen. He first noticed the nodular lesion approximately 2 years ago. Clinical examination revealed a slight reddish surface colored, elastic hard nodule, measuring approximately 2 cm, on his right lower abdomen (
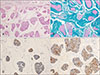
Fig. 1). The regional lymph nodes were not involved. The skin lesion was completely resected under local anesthesia and the margins were free of tumor in this case. Microscopic examination revealed numerous small tumor cell islands with pools of mucinous materials in the dermis (
Fig. 2A). Alcian blue staining of mucin was positive at pH 2.5 (
Fig. 2B). The numerous mucin also indicated positive periodic acid-Schiff stain.
Immunohistochemical studies were performed on formalin-fixed, paraffin embedded tissue, using cytokeratin (CK) 7, 20, epithelioid membrane antigen (EMA), gross cystic disease fluid protein (GCDFP)-15, thyroid transcription factor 1 (TTF1), napsin A, and CDX2 antibodies. Among them, CK7, GCDFP-15, and EMA were predominantly stained in the tumor cells consist with islands (
Fig. 2C, D). We received the patient's consent form about publishing all photographic materials.
PCMC is sometimes misdiagnosed as metastatic skin carcinoma, especially colon cancer, and lung cancer
12. Therefore, internal malignancies should be ruled out since the subcutaneous lesion could represent metastatic skin tumor. Immunohistochemically, mostly the metastatic mucinous carcinoma of colon cancer indicated CK20 and CDX2 were stained in tumor cells
34. In contrast, the metastatic carcinoma of lung cancer showed tumor cells were stained with CK7, TTF1 and napsin A
45. In our case, the tumor cells were negative for TTF1, napsin A, and CDX2. Furthermore, no distant metastasis was found by positron emission tomography Image, pelvic computed tomography, and chest X-P. Therefore, these findings supported diagnosis of PCMC.
Kamalpour et al.
2 summarized one hundred fifty-nine cases of PCMC, of which 86.2% (137/159) appeared on the head and neck. The eccrine sweat gland abundant lesion, such as axilla and genital areas are especially found.
However, it may occur other sites and its rate was 3.8% (6/159). Breiting et al.
4 reported 15 PCMC during 25 years. Among them, one PCMC appeared on the abdomen. Our case is also seen on the lower abdomen but not on the head and neck. It seemed to be appeared on the location of which no abundant sweat glands. Local recurrence occurs frequently about 30% to 40%, but distant and lymph node metastases were rare and the rate is about 6%. In addition, lesion location on the trunk compared to head and neck indicated bad outcome having recurrence or metastasis
2. PCMC is unclear what factor may lead to high local recurrent rate
12. The patient had no evidence of local recurrence after a follow-up period of 2 years. Although the skin lesion was completely resected for this case, careful follow-up should be recommended.





 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download