This article has been
cited by other articles in ScienceCentral.
Abstract
A previously healthy 2.5-year-old male child presented with vomiting, diarrhea, and fever. During hospitalization he developed odynophagia and refusal to eat. His symptoms did not respond to acid suppressant therapy. He underwent upper endoscopy which showed severe inflammation, ulcerations and abundant necrosis. Histopathological features and serological testing were consistent with herpetic esophagitis. He had no history of recurrent infections or history of sick contacts. His immunological work up showed normal level of immunoglobulins and his White Blood Cells subpopulations were normal. His HSV serology was positive. The patient was started on acyclovir 5 mg/kg q 8 hours. He resolved his symptoms within 24 hours of treatment.
Keywords: Herpes simplex, Ulcer, Esophagitis, Acyclovir, Child
INTRODUCTION
Herpes simplex virus (HSV) is a cause of severe erosive esophagitis, in immunocompromised hosts. Esophagitis in such hosts represents reactivation of the virus, due to immune suppression [
1]. Although herpes infection is common even in immune competent individuals, herpes simplex esophagitis (HSE) is rare. This may reflect a lack of awareness of the condition or the self-limiting nature, of the disease in most instances [
2].
HSE shares typical presentation with more common diseases, such as reflux, leaving many HSE patients undiagnosed [
2]. We describe here a young child presented with suspected gastroenteritis, who developed odynophagia, and refused to eat even after diarrhea and vomiting were resolved. His endoscopic and pathologic findings, were consistent with HSE. The patient responded to acyclovir treatment, with complete resolution.
CASE REPORT
A previously healthy 2.5-year-old male presented with vomiting, diarrhea, and fever beginning 2 days previously. He had moderate dehydration, requiring intravenous fluid therapy. His symptoms improved after 2 days of admission, but refused to eat, which was thought to be secondary to oral thrush. Although the thrush was resolved, he continued to refuse feeding and complained of odynophagia. Acid suppressant therapy was started, with no improvement. He had no mouth ulcers, and no history of recent corrosive drug ingestion. He had no history of recurrent infections, or of growth or developmental concerns. He had no skin rashes and the family denied contact with patients with skin rashes.
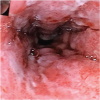
Upper endoscopy revealed a severely inflamed esophagus, with exudation and necrosis involving the mid and lower esophagus (
Fig. 1). Histopathology showed mucosal infiltrate with heavy acute inflammation, with no significant eosinophilic infiltrate (
Fig. 2A). Few cells exhibited herpetic cytopathic changes (
Fig. 2B). Periodic acid–Schiff staining for fungal infection was negative. Unfortunately, at the time of presentation, polymerase chain reaction (PCR) at the biopsy tissue, was not available at our facility.
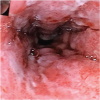 | Fig. 1 Endoscopic examination reveals severe inflammation, with ulceration and exudate.
|
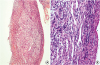 | Fig. 2 Histopathologic examination of the esophageal mucosa biopsy (hematoxylin and eosin staining). (A) Fragments of ulcer slough and granulation tissue, are also observed. Few cells exhibit cytopathic changes suggestive of herpetic viral etiology; in the form of multinucleation, chromatin margination, and vague nuclear inclusions. Denuded mucosa, ulcer slough, and granulation can be observed (100×). (B) A high-power view (400×) of the same tissue fragment, shows viral cytopathic changes (multinucleation, chromatin margination, and vague nuclear inclusions).
|
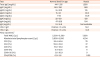
Testing for HSV immunoglobulins (Igs) type G and M (IgG and IgM) were positive. The patient had no leukopenia and immunological workup was normal, including total Igs, IgG subclasses (
Table 1). Flow cytometry to evaluate specific cell populations and subpopulations to identify major primary immunodeficiency, was normal also (
Table 1). The patient was started on acyclovir 5 mg/kg/dose TID for 10 days intravenously. The patient improved dramatically, and symptoms resolved completely. On follow up, the patient showed no recurrence of symptoms or features of either immunodeficiency, or difficulty with swallowing.
Table 1
Viral titers and immunological work up results
|
Test |
Normal level for age |
Result |
|
Total IgG (mg/dL) |
441–1,135 |
1,290 |
|
IgG1 (mg/dL) |
240–780 |
983 |
|
IgG2 (mg/dL) |
55–200 |
135 |
|
IgG3 (mg/dL) |
15–93 |
89.5 |
|
IgG4 (mg/dL) |
1–94 |
84.9 |
|
IgA (mg/dL) |
22–159 |
129 |
|
IgM (mg/dL) |
47–200 |
164 |
|
IgE (mg/dL) |
1.9–16.9 |
Not available |
|
HSV-1 IgM |
Positive >11 units |
50.1 |
|
HSV-1 IgG |
Positive >11 units |
34.2 |
|
Flow cytometry*
|
|
|
|
Total WBC (/µL) |
5,500–15,500 |
7,200 |
|
Absolute total lymphocyte count (/µL) |
3,000–9,500 |
4,104 |
|
CD3 (%) |
59.4–84.6 |
78 |
|
CD4 (%) |
29.0–59.0 |
37 |
|
CD8 (%) |
19.0–48.0 |
39 |
|
CD19 (%) |
6.4–22.6 |
11 |
|
CD16+56 (%) |
5.6–30.9 |
9 |
|
CD4/CD8 (%) |
0.9–3.6 |
0.95 |

Consent for publication
The patient's parent gave their consent for publication of this Case report and any accompanying images. None of the images contain any patient's identifiers. The Institutional Review Board was not required.
DISCUSSION
HSV is a common infection in children. Gingivostomatitis represents the most common presentation. Concomitant involvement of oropharyngeal and esophageal mucosa, may be under-recognized. Herpetic esophagitis is commonly described in immunocompromised and debilitated patients. However, immunocompetent children can also acquire the disease [
1].
Diagnosis of HSE can be confirmed by demonstrating classical endoscopic findings, and evidence of herpetic infection (viral culture, PCR, or serology) in addition to characteristic viral cytopathologic findings. In late stages of HSE, mucosal necrosis dominates [
3].
The majority of reported immunocompetent patients with HSE had no history of exposure to HSV prior to presentation, and lacked clinical evidence of herpetic lesions elsewhere on the body [
24]. Consistently, our patient had no history of exposure to HSV, and no other signs of concurrent herpes infection. Most of the patients presented with abrupt esophageal symptoms. Odynophagia, heart burn, and fever, were the most common reported symptoms of HSE [
2]. In our patient; presentation with acute gastroenteritis masked abruptness of esophageal symptoms, a complication of persistent vomiting.
HSE affects a large portion of the esophagus in the majority of patients. The mid or distal esophagus is most commonly affected [
25]. In our patient, diagnosis was established by classical site involvement of the esophagus, with ulceration and significant amount of exudate. Histopathologic examination demonstrated classical viral cytopathic changes. Diagnosis was confirmed by highly positive HSV IgM, and seroconversion of HSV IgG into positive.
Although HSE is a self-limiting condition, antiviral treatment may shorten the illness, and reduce patients' suffering [
5]. Furthermore, gastrointestinal bleeding and esophageal perforation complicate the course. Acyclovir is a nucleoside analog highly active against herpes virus. The efficacy of acyclovir in treating immunocompetent hosts with esophagitis, has not been examined in major clinical trials. A small series of pediatric patients treated with 5 mg/kg/dose TID, showed dramatic response with no significant side effects [
3]. Our patient received the same dose, which he tolerated very well. He showed significant improvement, by the second day of therapy.
HSE is an acute infection, believed to resolve totally with no significant morbidities. However, new reports identified a relationship between herpetic and eosinophilic esophagitis (EoE) [
6]. The underlying mechanism is unclear; HSE may predispose patients to develop EoE, or esophageal injury from EoE, may predispose patients to viral infection [
6]. Even absence of histological features of EoE on diagnosis, is not sufficient to exclude EoE. This may necessitate prolonged follow up with those patients. Although the period of follow up in our patient is not that lengthy (4 months), the patient demonstrated no pain or difficulty in swallowing since treatment.
In conclusion, although HSE is rare in immunocompetent patients, this case provides an example of occurrence in a pediatric patient, with symptoms masked by concurrent gastroenteritis. Identifying HSE in such patients is critical, because treatment with antiviral therapy can quickly resolve the disease.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download