This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Severe acute malnutrition (SAM) is an important public health problem which contributes to significant number of under five deaths. Protocol based management significantly decreases risk of deaths in children with medical complications.
Methods
Outcome of children aged 2 months–5 years admitted and fulfilling definition of SAM having diarrhea (group A) was compared to children with SAM having medical complications other than diarrhea (group B). Both groups were managed according to standard recommended protocols and monitored and followed up for 12 weeks after discharge.
Results
The average weight gain, defaulter rate, primary failure, secondary relapse rate and readmission rate were similar in both groups. Length of stay in group A was three days longer (p-value=0.039). Discharge rate was comparable with overall 68% of children successfully discharged and 50% of children reaching weight/height >−2 standard deviation at follow-up of 12 weeks.
Conclusion
The current management protocol is equally effective for managing children with SAM having diarrhea. Good adherence to management protocol of dehydration and timely modification of therapeutic feeds in children with persistent diarrhea results in satisfactory weight gain.
Keywords: Malnutrition, Cachexia, Dehydration
INTRODUCTION
Severe acute malnutrition (SAM) is one of the major causes of morbidity and mortality among children in developing countries and is an important contributing factor to deaths occurring from preventable causes in children less than five years of age [
1]. According to the National Family Health Survey-4 in India, 21% of children under five were underweight (low weight for height) and among them, more than 7.5% suffered from SAM [
2].
Globally, around 10 million children die every year, more than 1.5 million of them from diarrhea [
3]. Diarrhea is the most common morbidity in SAM children and the relationship between malnutrition and diarrhea is bidirectional. Malnutrition predisposes to a greater incidence of diarrhea and the duration of diarrhea and malnutrition is worsened by diarrhea.
With the use of a standardized World Health Organization (WHO) case management protocol and nutritional rehabilitation in hospitals, the case fatality rates can be dramatically reduced from over 30% to 5%–10% [
1]. The Ministry of Health & Family Welfare (MoHFW), Government of India (GOI) has released guidelines for the facility-based management of children with SAM. The WHO recommends community-based management with ready-to-use therapeutic foods for children over six months of age with SAM without medical complications. In the inpatient setting, special therapeutic diets (F-75/F-100) are recommended for the stabilization and rehabilitation of children with SAM. The WHO also recommends Rehydration Solution for Malnutrition (ReSoMal) for rehydration of severe, acutely malnourished children with lower sodium levels and higher glucose and potassium levels. However, if F-75/F-100 and ReSoMal are unavailable, the MoHFW guidelines recommend the use of locally-prepared starter and catch-up diets and low osmolality oral rehydration solution (ORS) with added potassium for rehydration of children with SAM [
1].
Severely malnourished children with diarrhea may also have osmotic diarrhea due to carbohydrate intolerance as a result of villous atrophy. The sugars (including glucose) in diets and rehydration fluids may result in increased fluid losses from the gut in these children, worsening diarrhea [
4]. Thus, there is the probability that therapeutic foods can aggravate diarrhea and these children may need additional care or diet modifications.
At present, it is not known whether the currently recommended management protocol is equally effective for the management of children with SAM with diarrhea or other medical complications. This research paper highlights the outcomes of these children managed with the standard WHO protocol.
MATERIALS AND METHODS
Children aged 2 to 59 months meeting the case definition of SAM (for children >6 months of age: weight for height ≤−3 standard deviation (SD) and/or mid-upper arm circumference [MUAC] <11.5 cm and/or edema of both feet; and for infants <6 months: weight for height ≤−3SD and/or edema of both feet) were included in the study and divided into two groups. Group A included SAM children with diarrhea and group B included SAM children with medical complications other than diarrhea. Approval was obtained from the institutional ethics committee and informed consent was obtained before the participants were enrolled. Enrolled children were admitted from pediatric wards of Kalawati Saran Children's Hospital, New Delhi, India from November 2015 to March 2017. Detailed history and physical examination findings were recorded on a pre-structured form. Children with secondary causes of malnutrition like human immunodeficiency virus (HIV), tuberculosis, gastroesophageal reflux disease, chronic liver disease, chronic kidney disease, congenital heart disease, neurological disabilities, suspected cases of inborn errors of metabolism, dysmorphologies, congenital malformations and any surgical cause of diarrhea were excluded.
Baseline analyses, including blood sugar, complete blood counts, serum electrolytes, chest X-rays, Mantoux tests, routine and microscopic urinalyses, and stool culture sensitivities, were done and all children were managed according to the standard protocol [
1] in the Nutritional Rehabilitation Centre (NRC) hospital. Children with medical complications other than diarrhea were administered an appetite test at admission to determine the type of feeding for initial management. Dehydration was managed using low osmolality ORS with added potassium supplements (20 mEq/L) and all patients received age-appropriate doses of multivitamins and minerals according to the WHO protocol. Iron was added during the rehabilitative phase. All children were monitored for complications of hypoglycemia, hypothermia, shock, dehydration, and congestive cardiac failure. Each child's progress was monitored daily by calculating the weight gain (gm/kg/day), 24-hour dietary intake, the disappearance of edema, and weekly length/height and MUAC.
All children with diarrhea were started on a milk-based, non-cereal starter diet and an algorithmic approach was used for diet planning. Children with SAM with acute diarrhea were started on 2-hourly starter therapeutic feedings (F-75), however, if the number of stools remained high (>10 stools/day), along with weight loss, even after 48 hours of starter diet, it was changed to a cereal-based starter diet or curd feed. All children not responding to this diet were changed to a lactose-free diet. All children with persistent diarrhea were examined to rule out comorbidities like pneumonia, urinary tract infections, HIV, and tuberculosis. HIV or tuberculosis-positive children were excluded from the study but continued to be managed in the NRC according to the protocol. All children with continuing diarrhea were managed with the unit protocol. Once the catch-up diets were well-tolerated, medical complications resolved, and satisfactory weight gain achieved (i.e., more than 5 gm/kg/day), they were allowed three feedings of semi-solids like Khichri (a mixture of cooked rice and dal), Dalia (a mixture of milk and broken wheat), bananas, curd-rice, and other locally-available diets. The children were considered fit to be discharged from the hospital when they met the discharge criteria [
1].
After discharge, they were followed up after one week, then every 15 days up to 12 weeks. Outcome parameters, including mean weight gain, the length of stay (in days), the death rate during hospitalization or after discharge during follow-up, default rates, successful discharge rates, secondary relapse rates, and the proportion with failures (primary and secondary), were calculated for both groups. GOI-recommended guidelines were used to define all the rates. The default rate was defined as the number of children who defaulted during the reporting period divided by the total number of participants. The successful discharge rate was the proportion of children who met the discharge criteria (weight gain >5 gm/kg/day on three consecutive days and resolution of medical conditions). The secondary relapse rate was defined as patients who were discharged as cured within the last two months but were again eligible for admission. Primary failure was defined as failure to regain appetite or to start losing edema by day four or the presence of edema or the failure to gain at least 5 gm/kg/day by day 10. Secondary failure was defined as failure to gain at least 5 gm/kg/day for three consecutive days during the rehabilitation phase.
Outcomes were also determined by the following criteria at the 12-week follow-up: The proportion of children gaining 15% of their admission weight, the proportion of children reaching −2SD or above the weight/height standard, and the proportion of children reaching an MUAC of 12.5 cm.
RESULTS
During the study period (November 2015–March 2017), a total of 163 children admitted to the NRC and pediatric wards were screened. Out of these 163, 85 children were admitted with diarrhea (group A) and 78 with medical complications other than diarrhea (group B).
Fig. 1 depicts the flow chart of patient inclusion in the study. Out of these 163 patients, 43 patients were excluded (25 children in group A and 18 patients in group B), thus, 120 children (60 each in groups A and B) were available for the analysis. Major morbidities in the enrolled children included diarrhea (50%), pneumonia (40%), bronchiolitis (8.3%), and severe anemia (8.3%) (
Fig. 2). The majority of patients in each group were 6 to 12 months old and males outnumbered females in both groups.
 | Fig. 1
Flow chart of inclusion of patients in the study.
SAM: severe acute malnutrition, TORCH: toxoplasmosis, other (syphilis), rubella, cytomegalovirus, herpes simplex, GDD: Global developmental delay, GOI: Government of India.

|
 | Fig. 2 Clinical profile of patients included in study.
|
Among the children admitted with diarrhea, 71.1% had acute watery diarrhea and 58.3% were dehydrated. Pneumonia was seen as a co-morbidity in 5% of the children in group A and an additional 5% had edema. Among the children with acute diarrhea, 46.6% required dietary modification in the form of cereal-based or lactose-free starter diets, while 62.5% with persistent diarrhea required dietary modification due to continuous diarrhea and the associated weight loss (
Fig. 3). Most children had suboptimal feeding practices. All children aged 2 to 6 months were either mixed fed or top fed and bottle feeding was a common practice in both groups.
 | Fig. 3 Type of starter diet required during stabilization phase in group A: with diarrhea.
|
Overall, 68% of the children were successfully discharged and 50% reached a weight/height > −2SD on follow-up. The average weight gain, deaths (during hospitalization), successful discharge rates, default rates, primary failures, secondary relapse rates, and readmission rates were similar in both groups (
Table 1). The average length of stay was three days longer in patients with diarrhea compared to those with complications other than diarrhea (13.25±6.36 vs. 10.73±5.35 days) and the difference was statistically significant (
p=0.039). The secondary failure rate was higher in patients with complications other than diarrhea than in patients with diarrhea (25 [42.4%] vs. 13 [23.2%],
p=0.024). At follow-up, both the groups had similar outcome parameters (weight gain >15% from admission, weight/height >−2SD or above, and MUAC >12.5 cm) (
Table 2).
Table 1
Outcome indicators of the study in children in both the study groups
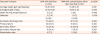
|
Outcome indicator |
SAM with diarrhea (n=60) |
SAM with complications other than diarrhea (n=60) |
p-value |
|
Average weight gain (gm/kg/day) |
10.35±6.65 |
10.39±6.27 |
0.782 |
|
Average length of stay |
13.25±6.36 |
10.73±5.35 |
0.039 |
|
Death (during hospitalisation) |
2 (3.3) |
0 (0) |
0.496 |
|
Defaulter |
2 (3.4) |
1 (1.7) |
1.000 |
|
(n=56) |
(n=59) |
|
|
Successful discharge rate |
37 (66.1) |
42 (71.2) |
0.838 |
|
Primary failure |
20 (35.7) |
16 (27.1) |
0.320 |
|
Secondary failure |
13 (23.2) |
25 (42.4) |
0.024 |
|
Secondary relapse rate |
8 (14.3) |
7 (11.9) |
0.783 |
|
Readmission rate |
4 (7.1) |
2 (3.4) |
0.783 |

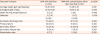
Table 2
Follow-up indicators of the study in the two groups

|
Outcome indicator |
SAM with diarrhea (n=53) |
SAM with complications other than diarrhea (n=54) |
p-value |
|
Gaining 15% weight from admission weight |
27 (51) |
35 (64.8) |
0.146 |
|
Weight/height −2SD or above |
24 (45.3) |
29 (53.7) |
0.384 |
|
MUAC >12.5 cm |
16 (30.2) |
18 (33.3) |
0.727 |

DISCUSSION
Most of the children with SAM in this study were less than 24 months old, indicating the higher vulnerability of this age group for developing malnutrition. Since feeding practices were suboptimal in all children, this reinforces the importance of exclusive breastfeeding during the first 6 months of life to prevent malnutrition.
The average weight gain was similar in both groups, around 10.37 gm/kg/day, which was acceptable according to Sphere standards (>8 gm/kg/day) [
5] and higher than that achieved in previous studies in India [
67]. Thus, the study showed that, even in children with diarrhea and SAM, satisfactory weight gain could be achieved with protocol-based management. The average length of hospital stay was 12.12±5.89 days, indicating that most patients were stabilized and discharged within two weeks, which is in agreement with the national and international guidelines for minimum stay durations of one to four weeks [
5]. The length of stay in SAM children with diarrhea was three days longer than those with medical complications other than diarrhea, showing that children with diarrhea needed longer times for stabilization before discharge.
In the present study, an overall case fatality rate of 2.5% was observed, which was within the acceptable level of care in the Sphere standards [
5] and similar to other studies from the NRC of India [
68]. However, it was lower than a study from Bangladesh [
9]. The lower mortality rate in the present study could be due to differences in secondary causes in the study population, such like HIV, tuberculosis, and surgical causes which were excluded in our study. The availability of resources and skilled round-the-clock staff in the present study, conducted at a tertiary care hospital, may also have contributed to the lower mortality rate. Previous studies from Kenya and Zambia reported higher mortalities in SAM children admitted with diarrhea than those without. However, the mortality rates were similar to our study [
1011].
The default rate in the present study was 2.5%, which is acceptable according to Sphere standards (<15%) and lower than those from Bangladesh and Uttar Pradesh (UP), India (19.3% and 47.2%, respectively) [
5812].The successful discharge rate in our study was higher than that of the NRC in UP (24.2%) but lower than that reported from Bangladesh (88.4%) [
812]. The proportion of treated children gaining 15% weight over their admission weight, reaching weight for height ≥−2 SD, and those attaining MUAC >12.5 cm was similar to the study from Bangladesh (62.4%) and higher than the study from UP (46.8%) [
89]. The outcome variables were also similar in both groups, showing that even children with SAM with diarrhea recovered well if managed with protocol-based care.
In conclusion, this study showed that the current management protocol was equally effective in children with SAM with diarrhea and SAM with other medical complications. Good weight gain was observed in both groups. However, children with SAM and diarrhea needed longer hospital stays.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download