Abstract
Supratentorial extraventricular anaplastic ependymoma (SEAE) in adults is a relatively rare intracranial tumor. Because of the very low prevalence, only a few cases have been reported. According to a recent study, SEAE is associated with a poor prognosis and there is no definite consensus on optimal treatment. We report a case of an adult SEAE patient who had no recurrence until seven years after a gross total resection (GTR) followed by conventional radiotherapy. A 42-year-old male had a persistent mild headache, left facial palsy, dysarthria, and left hemiparesis. Preoperative neuroimaging revealed an anaplastic astrocytoma or supratentorial ependymoma in the right frontal lobe. A GTR was performed, followed by adjuvant radiotherapy. Histologic and immunohistochemical results revealed anaplastic ependymoma. After seven years of initial therapy, a regular follow-up MRI showed a 3-cm-sized partially cystic mass in the same area as the initial tumor. The patient underwent a craniotomy, and a GTR was performed. Histopathologic examination revealed recurrence of the SEAE. External radiotherapy was performed. The patient has been stable without any disease progression or complications for 12 months since the surgery for recurrent SEAE.
Intracranial ependymoma is an uncommon central nervous system (CNS) tumor. Among all CNS tumor, it accounts for only 2–3% [1]. Most of these intracranial ependymomas arise from the cerebral ventricles in the infratentorium or the central canal of the spinal cord, but rarely develop from supratentorial area without any relation to the cerebral ventricle or the choroid plexus [234]. Only a few cases of supratentorial extraventricular anaplastic ependymoma (SEAE) have been reported in the literatures due to very low prevalence. We report a case of recurrent SEAE in adult patient.
A 42-year-old male patient visited the emergency department with persistent mild headache, left facial palsy, dysarthria, and left hemiparesis. These symptoms started 3 days ago, and increased over time. Neurological examination disclosed grade 4 paresis of the left limb and left facial palsy. MRI showed a 5.7-cm-sized mass surrounding with vasogenic edema in the frontal lobe (Fig. 1A). That mass included a cystic portion and it was shown the strong enhancement after intravenous gadolinium injection (Fig. 1B, C). Based on the MRI results, anaplastic astrocytoma or supratentorial ependymoma were expected. Surgical resection was performed via craniotomy and gross total resection (GTR) of the tumor was achieved (Fig. 1D).
Histological and immunohistochemical results revealed anaplastic ependymoma, World Health Organization (WHO) grade III (Fig. 2). Histological examination of resected specimen revealed a highly cellular tumor composed of numerous pseudorosettes and regional necrosis without pseudopalisades. Immunochemical result of glial fibrillary acidic protein revealed strong positivity in the tumor cells. Endothelial membrane antigen had negative reactivity. Staining of neuronal markers, including chromogranin A, cytokeratin protein, S100 and synaptophysin, was negative. The Ki-67 labeling index was strong proliferative activity and aggressiveness as 10–20%.
Whole-spine MRI and cerebrospinal fluid cytology were performed for systemic evaluation, and there was no definite evidence of systemic dissemination.
External radiotherapy was performed for 6 weeks with the dose of 5,600 cGy in 6 weeks after operation. The patient did not receive any chemotherapy.
The patient underwent annual follow-up MRI evaluations, and there was no evidence of radiographic progression and there were no definite neurologic deficits for over 6 years.
After 7 years, a regular follow up MRI showed a 3-cm-sized partially cystic mass in the right frontal lobe. The patient was symptom-free and there were no definite abnormal results on physical examination, Karnofsky Performance Status score was 100. The patient underwent a craniotomy and GTR of the tumor was achieved (Fig. 3).
Pathologic examination of the biopsy revealed recurrent anaplastic ependymoma, WHO grade III. Whole-spine MRI was enforced for examination of cerebrospinal seeding, and there was no definite abnormal signal change. External radiotherapy was performed for 4 weeks with the dose of 4,000 cGy in 3 weeks after operation and no chemotherapy was performed. The patient was discharged without any symptoms or meaningful results in radiologic examination. For 12 months after the operation of recurrent SEAE, he has been stable without any disease progression.
SEAE is a very rare CNS tumor, and only a few cases have been previously reported in the literature [56]. The pathophysiology of this type of tumor is not yet fully established. Vernet et al. [7] reported that this type of tumor may derive from 1) germinal matrix migration disorders, 2) neuroectodermal neoplasms that differentiate into the ependymal lineage, and 3) neoplastic growth of an ectopic ependymal cell [7].
SEAE has been reported to have a poorer prognosis than an infratentorial ependymoma [28]. Wang et al. [9] reported that 5-year progression-free survival and overall survival (OS) rates of SEAE were 33% and 52% in 38 of 55 SEAE patients. Byun et al. [6] recently reported the median OS and 5-year OS of SEAE was 31.7 months and 30% in 6 of 15 SEAE patients. Recurrent SEAE has a very poor prognosis. Byun et al. [6] reported that three of four recurrent SEAE patients died due to disease progression in spite of surgery, radiotherapy and chemotherapy treatment.
Because of its very low prevalence, no definite general consensus of optimal treatment exists for SEAE. Several reports have expressed that GTR with adjuvant radiotherapy is the main treatment of SEAE [6910]. In the case of recurrence, reoperation for the purpose of complete resection is considered [9]. Several authors reported that possible poor prognostic factors of intracranial ependymoma: incomplete tumor resection, young age, histological anaplagia, supratentoral, extraventricular location and unenforced adjuvant radiotherapy [810]. In SEAE, GTR, and adjuvant radiotherapy are important prognostic factors and adjustable factors.
In the present case, GTR was achieved with craniotomy and external radiotherapy was done for 6 weeks with the dose of 5,600 cGy (Fig. 1D). After 7 years, the patient recurred on the same site. We performed to redo surgery. GTR was achieved and external radiotherapy was done for 4 weeks with the dose of 4,000 cGy (Fig. 3D). In spite of recurrent SEAE has a very poor prognosis, the patient has been stable for 7 years without any disease progression and complication.
In conclusion, our case verifies that GTR and adjuvant radiotherapy should be the most important factors for treatment of SEAE. Future additional follow up studies and large-scale multicenter studies are required.
Figures and Tables
Fig. 1
Preoperative imaging studies and a follow-up MRI after surgery. A: The tumor had a heterogenous signal intensity with vasogenic edema on T2-weighted imaging, B: The tumor had a isodense intensity on T1-weighted imaging, C: The tumor showed a heterogenous and peripheral rim enhancement on contrast-enhanced T1-weighted imaging, D: A follow-up MRI in 1 days after surgery showed no definite remnant mass lesion on contrast-enhanced T1-weighted imaging.

Fig. 2
Histopathological findings. A: Hematoxylin and eosin-stained section express increased cellularity with perivascualr pseudorosettes (original magnification ×100). B: Immunohistochemical stainings for Ki-67 revealed strong proliferative activity and aggressiveness as 10–20% (original magnification ×100). C: Immunohistochemical stainings for glial fibrillary acidic protein revealed strong positivity in the tumor cells (original magnification ×100).
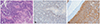
Fig. 3
Magnetic resonance images expressed a recurrent tumor in right frontal lobe. A: T2-weighted image demonstrated a recurrent tumor with heterogenous signal intensity and vasogenic edema. B, C: Contrast-enhanced T1-weighted MRI axial and coronal image showing a partially cystic mass with enhancing nodule on peripheral portion. D: A follow-up MRI in 1 day after surgery showed no definite remnant mass lesion on contrast-enhanced T1-weighted imaging.

References
1. Chen L, Zou X, Wang Y, Mao Y, Zhou L. Central nervous system tumors: a single center pathology review of 34,140 cases over 60 years. BMC Clin Pathol. 2013; 13:14.

2. Reni M, Brandes AA, Vavassori V, et al. A multicenter study of the prognosis and treatment of adult brain ependymal tumors. Cancer. 2004; 100:1221–1229.


3. Miyazawa T, Hirose T, Nakanishi K, Uozumi Y, Tsuzuki N, Shima K. Supratentorial ectopic cortical ependymoma occurring with intratumoral hemorrhage. Brain Tumor Pathol. 2007; 24:35–40.


4. Roncaroli F, Consales A, Fioravanti A, Cenacchi G. Supratentorial cortical ependymoma: report of three cases. Neurosurgery. 2005; 57:E192.

5. Lavrador JP, Oliveira E, Teixeira JC, Lopes JP, Pimentel J, Carvalho MH. Adult supratentorial extraventricular anaplastic ependymoma: therapeutic approach and clinical review. Asian J Neurosurg. 2018; 13:105–109.



6. Byun J, Kim JH, Kim YH, Cho YH, Hong SH, Kim CJ. Supratentorial extraventricular ependymoma: retrospective analysis of 15 patients at a single institution. World Neurosurg. 2018; 118:e1–e9.

7. Vernet O, Farmer JP, Meagher-Villemure K, Montes JL. Supratentorial ectopic ependymoma. Can J Neurol Sci. 1995; 22:316–319.


8. Guyotat J, Signorelli F, Desme S, et al. Intracranial ependymomas in adult patients: analyses of prognostic factors. J Neurooncol. 2002; 60:255–268.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download