Abstract
The cause of a pilonidal cyst is unclear, and treatment is still under debate. In Korea, the incidence of this disease is lower than that of Western countries, and it has often been misdiagnosed as a simple abscess. When pilonidal cysts are diagnosed, the principle of treatment is not to leave a residue, and a wide excision is needed to reduce the recurrence rate. This paper introduces a wide excision technique using Indigo-carmine dye to minimize the recurrence of a pilonidal cyst.
Figures and Tables
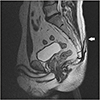 | Figure 1On the T2 weighted image (T2WI) of magnetic resonance imaging, 0.4×6.3×1.0 cm mass was found in the subcutaneous fat layer at the auricular area (arrow). The mass showed high, homogenous signal intensity and a homogenous signal intensity in the T2WI. No invasion into the muscular, epidural, medullary layer was observed. |
 | Figure 2Under general anesthesia, the patient was placed in the prone position, exposed to the sacrum, and prepared for sterilization. |
 | Figure 3Opening of the coccygeal area is the difference that helps distinguish a simple abscess from a pilonidal cyst. The probe is used to identify the range of the pilonidal cyst through this opening. |
 | Figure 4Indigo-carmine reagent is injected through the opening and waits for approximately 5 minutes to allow the inside of the cyst to stain sufficiently. |
 | Figure 5To determine the approximate extent of the lesion, palpation is needed, and then an incision line is drawn, including as much as 1 cm beyond the expected range including normal tissue. Both ends of the resection line are drawn in a spindle shape to prevent a dog ear deformity at the time of suturing. |
 | Figure 6Excision is performed on the presacral fascia layer, and care should be taken not to expose the sacral bone. |
 | Figure 7Excision is performed on the presacral fascia layer, and care should be taken not to expose the sacral bone. |
 | Figure 8Excision is performed on the presacral fascia layer. Ensure that no stained tissues remain on the resected surface. |
References
1. Akinci OF, Coskun A, Uzunköy A. Simple and effective surgical treatment of pilonidal sinus: asymmetric excision and primary closure using suction drain and subcuticular skin closure. Dis Colon Rectum. 2000; 43:701–706. discussion 706–7.

2. Hegele A, Strombach FJ, Schönbach F. Reconstructive surgical therapy of infected pilonidal sinus. Chirurg. 2003; 74:749–752.

3. Chamberlain JW, Vawter GF. The congenital origin of pilonidal sinus. J Pediatr Surg. 1974; 9:441–444.


4. Karydakis G. Hair insertion (pilonidal sinus). Hellenic Arm Forc Med Rev. 1968; 2:273–285.
6. Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. 1992; 62:385–389.


7. Hong CH, Ryoo SM. Pilonidal cysts occurring in the sacrococcygeal region and that were misdiagnosed as a simple abscess. J Korean Orthop Assoc. 2010; 45:97–100.

8. Benfatto G, Catania G, Altadonna V, et al. Drainage useful in the excision and closure “per primam” of pilonidal sinus: technical notes. Chir Ital. 2003; 55:621–624.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download