Abstract
Materials and Methods
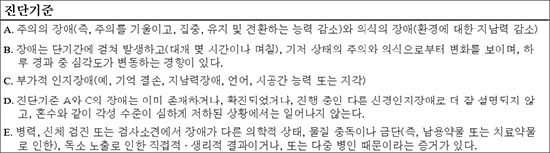
A total of 2,122 cases, who were older than 20 years and underwent orthopedic surgery at a single medical center during a one year period were included. Among them, 132 patients who were diagnosed with delirium after surgery under the Diagnostic and Statistical Manual of Mental Disorders-V criteria and medicated under the consultation of a psychiatrist were included in the study The differences in the incidence of delirium and several affecting factors were analyzed.
Results
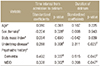
The overall incidence of delirium after surgery was 6.2% (132 in 2,122 cases). The mean age of the delirium group was 77.4 years (range, 54–92 years), which was higher than that of the non-delirium group (58.1 years). The percentage of women in the delirium group was 63.6% (84 in 132 cases), which was higher than that of the women in the non-delirium group (49.0%). The incidence of delirium after surgery was 9.3% (85 in 916 cases) due to trauma and 3.9% (47 in 1206 cases) due to disease. The incidence of postoperative delirium according to the surgical region was 29.2% (7 in 24 cases) in two or more regions, 13.7% (72 in 526 cases) in the hip, and 9.6% (14 in 146 cases) in the spine, 3.5% (20 in 577 cases) in the knee-lower leg, 2.5% (5 in 199 cases) in the foot-ankle, 2.4% (11 in 457 cases) in the shoulder-elbow, and 1.6% (3 in 189 cases) in the forearm-wrist-hand. Delirium occurred more rapidly in women and surgery due to disease, and the duration of delirium was longer in patients with dementia and major depressive disorders.
Conclusion
The incidence of postoperative delirium was high in cases of surgery due to trauma and in cases of surgery in two or more sites. The incidence of postoperative delirium according to a single surgical region was higher in the order of the hip, spine, and knee. Active intervention is needed regarding the correctable risk factor.
Figures and Tables
References
1. Statistics Korea. Population projections for Korea (2015~2065). Daejeon: Statistics Korea;2016. p. 56–59.
2. Zywiel MG, Hurley RT, Perruccio AV, Hancock-Howard RL, Coyte PC, Rampersaud YR. Health economic implications of perioperative delirium in older patients after surgery for a fragility hip fracture. J Bone Joint Surg Am. 2015; 97:829–836.


3. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlinton: American Psychiatric Publishing;2013. p. 596–598.
4. Dyer CB, Ashton CM, Teasdale TA. Postoperative delirium. A review of 80 primary data-collection studies. Arch Intern Med. 1995; 155:461–465.


5. Robertson BD, Robertson TJ. Postoperative delirium after hip fracture. J Bone Joint Surg Am. 2006; 88:2060–2068.


6. Hwang SK, Lee CH. Postoperative delirium after hip arthroplasty in the elderly. J Korean Hip Soc. 2010; 22:151–158.

7. Lee JK, Park YS. Delirium after spinal surgery in Korean population. Spine (Phila Pa 1976). 2010; 35:1729–1732.


8. Chung KS, Lee JK, Park JS, Choi CH. Risk factors of delirium in patients undergoing total knee arthroplasty. Arch Gerontol Geriatr. 2015; 60:443–447.


9. Song WS, Choi JC, Lee YS, et al. The risk factors of delirium in elderly patients with hip fracture: a prospective study. J Korean Hip Soc. 2008; 20:293–298.

10. Kim KH, Kho DH, Shin JY, Choi JY, Kim ES, Kim DH. Risk factors of postoperative delirium in elderly patients with hip fractures. J Korean Fract Soc. 2008; 21:189–194.

11. Kang KB, Suh DH, Oh SR. Delirium after intertrochanteric fractures of femur in elderly patients. J Korean Fract Soc. 2011; 24:131–137.

12. Wang L, Seok S, Kim S, Kim K, Lee S, Lee K. The risk factors of postoperative delirium after total knee arthroplasty. J Knee Surg. 2017; 30:600–605.


13. Kawaguchi Y, Kanamori M, Ishihara H, et al. Postoperative delirium in spine surgery. Spine J. 2006; 6:164–169.


15. Wang J, Li Z, Yu Y, Li B, Shao G, Wang Q. Risk factors contributing to postoperative delirium in geriatric patients postorthopedic surgery. Asia-Pac Psychiatry. 2015; 7:375–382.






 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download