Abstract
Purpose
The aim of this study was to determine if preoperative temporary discontinuation of antiplatelet medication (aspirin, clopidogrel, or cilostazol) is a safe procedure that does not increase early postoperative bleeding and allogenic blood transfusion after a total knee arthroplasty.
Materials and Methods
A retrospective analysis was conducted among consecutive patients who underwent navigation assisted primary total knee arthroplasty performed by a single surgeon, from January 2013 to December 2016. A total of 369 patients enrolled in this study were divided into two groups, 271 patients with no history of antiplatelet therapy and 98 patients who underwent 7 days of temporary withdrawal of antiplatelet therapy. Comparative analysis between the two groups, on the variation of hemoglobin and hematocrit during the first and second postoperative days, was conducted to determine the amount of early postoperative bleeding and the frequency of allogenic blood transfusion during hospitalization.
Results
The variation of hemoglobin, hematocrit during the first and second postoperative days and the frequency of allogenic blood transfusion between no history of antiplatelet medication and discontinuation antiplatelet medication before 7 days from surgery were similar in both groups. Of the 369 patients, 149 patients received a blood transfusion during their hospitalization. Compared to patients who did not receive a blood transfusion, those who did received blood transfusion were significantly older in age, smaller in height, lighter in weight, and showed significantly lower preoperative hemoglobin and hematocrit values. No statistically significant differences in sex, preoperative American Society of Anesthesiologists scores, and the history of antiplatelet medication until 7 days prior to surgery were observed between the two groups according to blood transfusion.
Conclusion
Compared to patients with no history of antiplatelet medication, the temporary discontinuation of antiplatelet medication 7 days prior to surgery in patients undergoing antiplatelet medication did not increase the amount of postoperative bleeding or the need for allogenic blood transfusion.
Figures and Tables
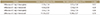
Table 2
The χ2 Test between Transfusion and the History of Antiplatelet Medication until 7 Days Prior to Surgery

References
1. Hernández-Vaquero D, Fernández-Carreira JM, Pérez-Hernández D, Fernández-Lombardía J, García-Sandoval MA. Total knee arthroplasty in the elderly. Is there an age limit? J Arthroplasty. 2006; 21:358–361.

2. Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141:e326S–e350S.
3. Mont MA, Jacobs JJ. AAOS clinical practice guideline: preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. J Am Acad Orthop Surg. 2011; 19:777–778.


4. Gross JB. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983; 58:277–280.

5. American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Practice guidelines for perioperative blood transfusion and adjuvant therapies: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Anesthesiology. 2006; 105:198–208.

6. Ahmed I, Chan JK, Jenkins P, Brenkel I, Walmsley P. Estimating the transfusion risk following total knee arthroplasty. Orthopedics. 2012; 35:e1465–e1471.

7. Cip J, Widemschek M, Benesch T, Waibel R, Martin A. Does single use of an autologous transfusion system in TKA reduce the need for allogenic blood?: a prospective randomized trial. Clin Orthop Relat Res. 2013; 471:1319–1325.


8. Sehat KR, Evans R, Newman JH. How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee. 2000; 7:151–155.

9. Nichols CI, Vose JG. Comparative risk of transfusion and incremental total hospitalization cost for primary unilateral, bilateral, and revision total knee arthroplasty procedures. J Arthroplasty. 2016; 31:583–589.e1.


10. Friedman R, Homering M, Holberg G, Berkowitz SD. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. J Bone Joint Surg Am. 2014; 96:272–278.


11. Carling MS, Jeppsson A, Eriksson BI, Brisby H. Transfusions and blood loss in total hip and knee arthroplasty: a prospective observational study. J Orthop Surg Res. 2015; 10:48.



12. Schwab PE, Lavand'homme P, Yombi J, Thienpont E. Aspirin mono-therapy continuation does not result in more bleeding after knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017; 25:2586–2593.


13. Harker LA. The kinetics of platelet production and destruction in man. Clin Haematol. 1977; 6:671–693.


14. Mufarrih SH, Qureshi NQ, Ali A, Malik AT, Naim H, Noordin S. Total knee arthroplasty: risk factors for allogeneic blood transfusions in the South Asian population. BMC Musculoskelet Disord. 2017; 18:359.

15. Conteduca F, Massai F, Iorio R, Zanzotto E, Luzon D, Ferretti A. Blood loss in computer-assisted mobile bearing total knee arthroplasty. A comparison of computer-assisted surgery with a conventional technique. Int Orthop. 2009; 33:1609–1613.

16. Hinarejos P, Corrales M, Matamalas A, Bisbe E, Cáceres E. Computer-assisted surgery can reduce blood loss after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2009; 17:356–360.


17. Mohanlal PK, Sandiford N, Skinner JA, Samsani S. Comparision of blood loss between computer assisted and conventional total knee arthroplasty. Indian J Orthop. 2013; 47:63–66.







 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download