1. Ramazani N. Different aspects of general anesthesia in pediatric dentistry: A review. Iran J Pediatr. 2016; 26:e2613.

2. Patel V, Singh N, Saksena AK, Singh S, Sonkar SK, Jolly SM. A comparative assessment of intranasal and oral dexmedetomidine for procedural sedation in pediatric dental patients. J Indian Soc Pedod Prev Dent. 2018; 36:370–375.


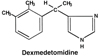
3. Devasya A, Sarpangala M. Dexmedetomidine: A review of a newer sedative in dentistry. J Clin Pediatr Dent. 2015; 39:401–409.


4. Chue PS, Chue JA. A review of the clinical uses of dexmedetomidine. Int J Clin Anesthesiol. 2017; 5:1080.
5. Khan ZP, Ferguson CN, Jones RM. alpha-2 and imidazoline receptor agonists:Their pharmacology and therapeutic role. Anaesthesia. 1999; 54:146–165.


6. Yuen VM. Dexmedetomidine: perioperative applications in children. Paediatr Anaesth. 2010; 20:256–264.


7. Bergendahl H, Lonnqvist PA, Eksborg S. Clonidine: an alternative to benzodiazepines for premedication in children. Curr Opin Anaesthesiol. 2005; 18:608–613.


8. Nishina K, Mikawa K, Shiga M, et al. Clonidine in pediatric anesthesia. Paediatr Anaesth. 1999; 9:187–202.

9. Lonnqvist PA, Bergendahl HT, Eksborg S. Pharmacokinetics of clonidine after rectal administration in children. Anesthesiology. 1994; 81:1097–1101.


10. Keles S, Kocaturk O. The effect of oral dexmedetomidine premedication on preoperative cooperation and emergence delirium in children undergoing dental procedures. BioMed Res Int. 2017; 2017:6742183.

11. Mittal NP, Goyal M. Dexmedetomidine: a potential agent for use in procedural dental sedation. Indian J Dent. 2014; 5:21–27.

12. Surendar MN, Pandey RK, Saksena AK, Kumar R, Chandra G. A comparative evaluation of intranasal dexmedetomidine, midazolam and ketamine for their sedative and analgesic properties: a triple blind randomized study. J Clin Pediatr Dent. 2014; 38:255–261.

13. Naaz S, Ozair E. Dexmedetomidine in Current Anaesthesia Practice- A Review. J Clin Diagn Res. 2014; 8:GE01–GE04.

14. Tobias JD, Berkenbosch JW. Initial experience with dexmedetomidine in paediatric-aged patients. Paediatr Anaesth. 2002; 12:171–175.


15. Karl HW, Rosenberger JL, Larach MG, Ruffle JM. Transmucosal administration of midazolam for premedication of pediatric patients. Comparison of the nasal and sublingual routes. Anesthesiology. 1993; 78:885–891.


16. Pimlott SJ, Addy M. Evaluation of a method to study the uptake of prednisolone sodium phosphate from different oral mucosal sites. Oral Surg Oral Med Oral Pathol. 1985; 60:35–37.


17. Berkenbosch JW, Tobias JD. Development of bradycardia during sedation with dexmedetomidine in an infant concurrently receiving digoxin. Pediatr Crit Care Med. 2003; 4:203–205.


19. Lammers CR, Rosner JL, Crockett DE, et al. Oral midazolam with an antacid increases the speed of onset of sedation in children prior to general anesthesia. Anesth Analg. 1999; 88:S300.

20. Sheta SA, Al-Sarheed MA, Abdelhalim AA. Intranasal dexmedetomidine vs midazolam for premedication in children undergoing complete dental rehabilitation: a double-blinded randomized controlled trial. Paediatr Anaesth. 2014; 24:181–189.


22. Kain ZN, Mayes LC, Wang SM, Caramico LA, Hofstadter MB. Parental presence during induction of anesthesia versus sedative premedication: which intervention is more effective? Anesthesiology. 1998; 89:1147–1156.

23. Schmidt AP, Valinetti EA, Bandeira D, Bertacchi MF, Simões CM, Auler JO Jr. Effects of preanesthetic administration of midazolam, clonidine, or dexmedetomidine on postoperative pain and anxiety in children. Paediatr Anaesth. 2007; 17:667–674.


24. Petroz GC, Sikich N, James M, van Dyk H, Shafer SL, Schily M, et al. A phase I, two-center study of the pharmacokinetics and pharmacodynamics of dexmedetomidine in children. Anesthesiology. 2006; 105:1098–1110.

25. Shukry M, Clyde MC, Kalarickal PL, Ramadhyani U. Does dexmedetomidine prevent emergence delirium in children after sevoflurane-based general anesthesia? Paediatr Anaesth. 2005; 15:1098–1104.


27. Yuen VM, Hui TW, Irwin MG, Yuen MK. A Comparison of intranasal dexmedetomidine and oral midazolam for premedication in pediatric anesthesia: a double-blinded randomized controlled trial. Anesth Analg. 2008; 106:1715–1721.


29. Blaudszun G, Lysakowski C, Elia N, Tramèr MR. Effect of perioperative systemic α2 agonists on postoperative morphine consumption and pain intensity systematic review and meta-analysis of randomized controlled trials. Anesthesiology. 2012; 116:1312–1322.


30. McGraw T, Kendrick A. Oral midazolam premedication and postoperative behaviour in children. Paediatr Anaesth. 1998; 8:117–121.


32. McCormack L, Chen JW, Trapp L, Job A. A comparison of sedation-related events for two multiagent oral sedation regimens in pediatric dental patients. Pediatr Dent. 2014; 36:302–308.

33. Levine MF, Spahr-Schopfer IA, Hartley E, Lerman J, MacPherson B. Oral midazolam premedication in children: the minimum time interval for separation from parents. Can J Anaesth. 1993; 40:726–729.


34. Sheta SA, AlSarheed M. Oral midazolam premedication for children undergoing general anaesthesia for dental care. Int J Pediatr. 2009; 2009:274380.

35. McMillan CO, Spahr-Schopfer IA, Sikich N, Hartley E, Lerman J. Premedication of children with oral midazolam. Can J Anaesth. 1992; 39:545–550.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download