Abstract
Purpose
Materials and Methods
Results
ACKNOWLEDGEMENTS
Notes
Author Contributions:
Conceptualization: Yun-Gyoung Hur, Sang-Nae Cho.
Data curation: Yun-Gyoung Hur, Ji Young Hong, Dong Hwan Choi.
Formal analysis: Yun-Gyoung Hur.
Funding acquisition: Sang-Nae Cho.
Investigation: Yun-Gyoung Hur, Ji Young Hong, Dong Hwan Choi, Ahreum Kim, Soyeong Park, Minsuk Kwon, Kyungjoon Kang, Jeong-Min Lee, Yoonsuk Lee.
Methodology: Yun-Gyoung Hur, Ji Young Hong, Dong Hwan Choi, Hoodon Joo, Sang-Nae Cho.
Project administration: Yun-Gyoung Hur.
Resources: Yun-Gyoung Hur, Ji Young Hong, Sang-Nae Cho.
Software: Jeong-Min Lee, Hoodon Joo.
Supervision: Yun-Gyoung Hur, Sang-Nae Cho.
Validation: Yun-Gyoung Hur, Ji Young Hong, Dong Hwan Choi, Ahreum Kim.
Visualization: Yun-Gyoung Hur.
Writing—original draft: Yun-Gyoung Hur.
Writing—review & editing: Yun-Gyoung Hur, Hazel M. Dockrell.
References
Fig. 1
Diagnostic value of the ichroma™ IGRA-TB test in identifying M. tb infection. The IFN-γ responses measured by ichroma™ IGRA-TB cartridges distinguished infected individuals with an AUC of 0.9706 (95% CI, 0.92–1.00, p<0.001) in ROC curve analysis (p<0.001). IGRA, IFN-γ release assay; TB, tuberculosis; CI, confidence interval; AUC, area under the curve; ROC, receiver operating characteristic.
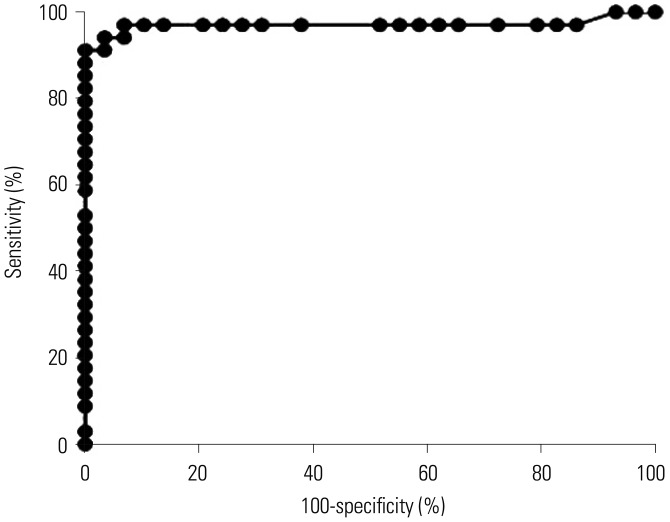
Fig. 2
Association of IFN-γ release between two different assays. The association of the IFN-γ responses between the QFT-GIT and ichroma™ IGRA-TB tests was analyzed by Spearman's correlation coefficient. The graph shows a very strong positive correlation of IFN-γ values between the two tests (r=0.91, p<0.001). QFT-GIT, QuantiFERON-TB Gold In-Tube; IGRA, IFN-γ release assay; TB, tuberculosis.
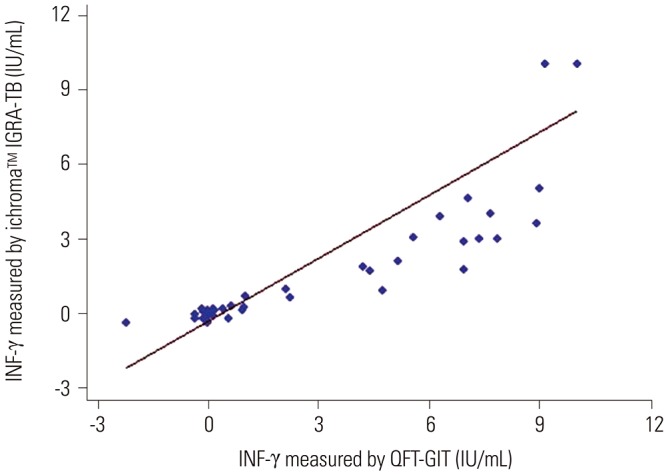
Table 1
Characteristics of the Study Participants
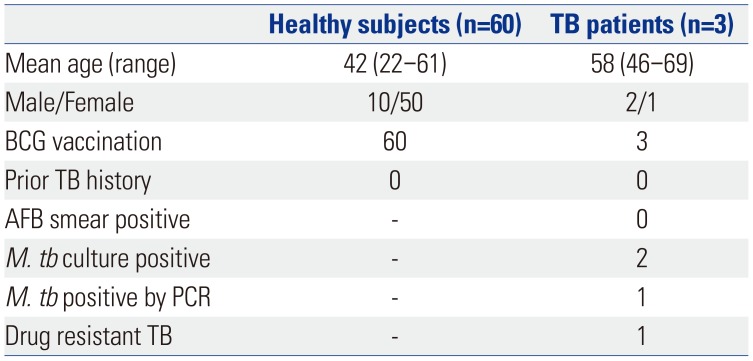
Table 2
Percent Positivity and Percent Negativity by QFT-GIT and ichroma™ IGRA-TB Tests in Healthy Subjects
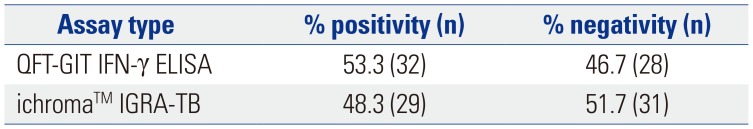
| Assay type | % positivity (n) | % negativity (n) |
|---|---|---|
| QFT-GIT IFN-γ ELISA | 53.3 (32) | 46.7 (28) |
| ichroma™ IGRA-TB | 48.3 (29) | 51.7 (31) |
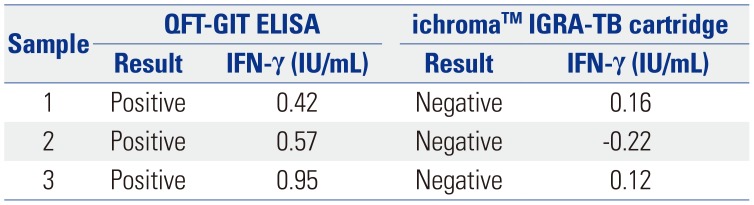
Table 3
Subjects Who Showed Differences in IFN-γ Positivity between the QFT-GIT and ichroma™ IGRA-TB Tests
| Sample | QFT-GIT ELISA | ichroma™ IGRA-TB cartridge | ||
|---|---|---|---|---|
| Result | IFN-γ (IU/mL) | Result | IFN-γ (IU/mL) | |
| 1 | Positive | 0.42 | Negative | 0.16 |
| 2 | Positive | 0.57 | Negative | -0.22 |
| 3 | Positive | 0.95 | Negative | 0.12 |
QFT-GIT, QuantiFERON-TB Gold In-Tube; ELISA, enzyme-linked immunosorbent assay; IGRA, IFN-γ release assay; TB, tuberculosis.
The three positive IFN-γ responders on the QFT-GIT test were weakly positive (≥0.35 but <1.0 IU/mL), and those responders did not show positive responses on the test with the ichroma™ IGRA-TB cartridge (≤0.21 IU/mL).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download