1. Dimitriou R, Tsiridis E, Giannoudis PV. Current concepts of molecular aspects of bone healing. Injury. 2005; 36:1392–1404. PMID:
16102764.

2. Delloye C, Cornu O, Druez V, Barbier O. Bone allografts: what they can offer and what they cannot. J Bone Joint Surg Br. 2007; 89:574–579. PMID:
17540738.
3. Dalkýz M, Ozcan A, Yapar M, Gökay N, Yüncü M. Evaluation of the effects of different biomaterials on bone defects. Implant Dent. 2000; 9:226–235. PMID:
11307409.

4. Kim YK, Yun PY, Lim SC, Kim SG. Sinus bone graft using OSTEON® and BioOss®: histologic comparative study. Implantology. 2007; 11:4–18.
5. Kim YK. Systematic classification and application of alloplastic bony substitutes and autogenous teeth bone graft material. J Dent Implant Res. 2009; 28:77–88.
6. Tadic D, Epple M. A thorough physicochemical characterisation of 14 calcium phosphate-based bone substitution materials in comparison to natural bone. Biomaterials. 2004; 25:987–994. PMID:
14615163.

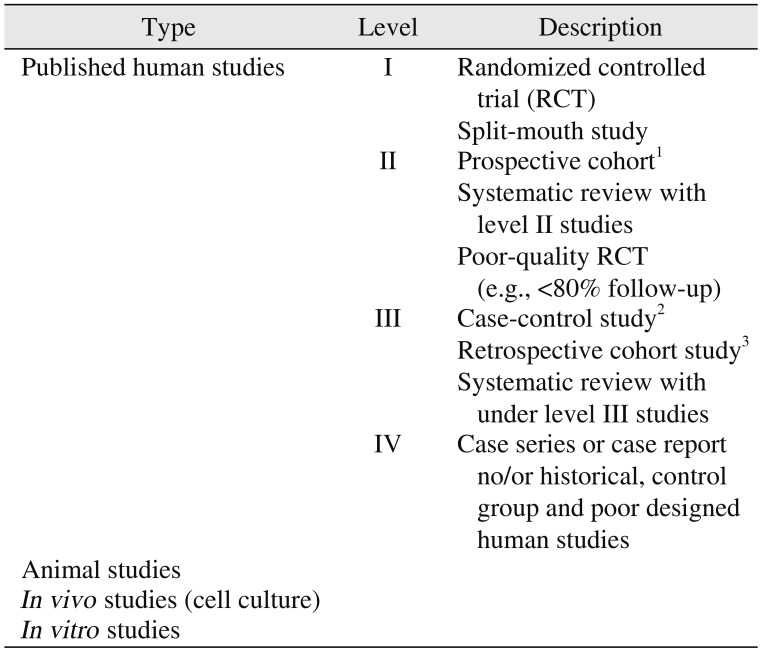
9. Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003; 85:1–3.

10. Kurien T, Pearson RG, Scammell BE. Bone graft substitutes currently available in orthopaedic practice: the evidence for their use. Bone Joint J. 2013; 95:583–597. PMID:
23632666.
18. Lim HC, Jung UW, You H, Lee JS. Randomized clinical trial of ridge preservation using porcine bone/cross-linked collagen vs. bovine bone/non-cross-linked collagen: cone beam computed tomographic analysis. Clin Oral Implants Res. 2017; 28:1492–1500. PMID:
28370361.

19. Lee JH, Lee JS, Baek WS, Lim HC, Cha JK, Choi SH, et al. Assessment of dehydrothermally cross-linked collagen membrane for guided bone regeneration around peri-implant dehiscence defects: a randomized single-blinded clinical trial. J Periodontal Implant Sci. 2015; 45:229–237. PMID:
26732806.

20. Benic GI, Joo MJ, Yoon SR, Cha JK, Jung UW. Primary ridge augmentation with collagenated xenogenic block bone substitute in combination with collagen membrane and rhBMP-2: a pilot histological investigation. Clin Oral Implants Res. 2017; 28:1543–1552. PMID:
28574217.

21. Kwak EJ, Cha IH, Nam W, Yook JI, Park YB, Kim HJ. Effects of locally administered rhBMP-2 and bisphosphonate on bone regeneration in the rat fibula. Oral Dis. 2018; 24:1042–1056. PMID:
29582561.

22. Papež J, Dostálová T, Chleborád K, Kříž P, Strnad J. Chronological age as factor influencing the dental implant osseointegration in the jaw bone. Prague Med Rep. 2018; 119:43–51.

23. Petrenko YA. Properties of mesenchymal stromal cells during 3D culturing within scaffolds of different origin. Probl Cryobiol. 2012; 22:144–147.
24. Horkavcová D, Zítková K, Rohanová D, Helebrant A, Cílová Z. The Resorption of ß-TCP and HA materials under conditions similar to those in living organisms. Ceram Silik. 2010; 54:398–404.
25. Strnadová M, Strnad Z, Šponer P, Jirošova J, Strnad J. In vivo behaviour of the synthetic porous hydroxyapatite prepared by low temperature microwave processing and comparison with deproteinized bovine bone. Key Eng Mater. 2012; 493-494:236–241.
26. Rohanová D, Horkavcová D, Helebrant A, Boccaccini AR. Assessment of in vitro testing approaches for bioactive inorganic materials. J Non-Cryst Solid. 2016; 432:53–59.

27. Lee DSH, Pai Y, Chang S. Effect of thermal treatment of the hydroxyapatite powders on the micropore and microstructure of porous biphasic calcium phosphate composite granules. J Biomater Nanobiotechnology. 2013; 4:114–118.

28. Dorozhkin SV. Calcium orthophosphate-based bioceramics and its clinical applications. In : Kaur G, editor. Clinical applications of biomaterials: state-of-the-art progress, trends, and novel approaches. Cham: Springer;2017. p. 123–226.
29. Dorozhkin SV. Multiphasic calcium orthophosphate (CaPO4) bioceramics and their biomedical applications. Ceram Int. 2016; 42:6529–6554.
30. Lee SM. Clinical evaluation of efficacy and safety of NOVOSIS-inject containing bmp-2 for socket preservation after extraction of a single-rooted tooth. Clin Oral Implant Res. 2018; 29:318.
31. Chang AR, Cho TH, Hwang SJ. Receptor activator of nuclear factor kappa-B ligand-induced local osteoporotic canine mandible model for the evaluation of peri-implant bone regeneration. Tissue Eng Part C Methods. 2017; 23:781–794. PMID:
28741427.

32. Song J, Kim J, Woo HM, Yoon B, Park H, Park C, et al. Repair of rabbit radial bone defects using bone morphogenetic protein-2 combined with 3D porous silk fibroin/β-tricalcium phosphate hybrid scaffolds. J Biomater Sci Polym Ed. 2018; 29:716–729. PMID:
29405844.

33. Park HJ, Min KD, Lee MC, Kim SH, Lee OJ, Ju HW, et al. Fabrication of 3D porous SF/β-TCP hybrid scaffolds for bone tissue reconstruction. J Biomed Mater Res A. 2016; 104:1779–1787. PMID:
26999521.

34. Alharissy M, AbouSulaiman A, Manadili A, Dayoub S. Radio graphic alternations in alveolar bone dimensions following socket preservation using two bone substitutes. J Int Dent Med Res. 2018; 11:906–910.
35. Naineni R, Ravi V, Subbaraya DK, Prasanna JS, Panthula VR, Koduganti RR. Effect of alendronate with β - TCP bone substitute in surgical therapy of periodontal intra-osseous defects: a randomized controlled clinical trial. J Clin Diagn Res. 2016; 10:ZC113–ZC117.

36. Miramond T, Borget P, Baroth S, Guy D. Comparative critical study of commercial calcium phosphate bone substitutes in terms of physic-chemical properties. Key Eng Mater. 2014; 587:63–68.

37. Jang CH, Cho YB, Yang HC, Kim JS, Choi CH, Jang SJ, et al. Effect of piperacillin-tazobactam coated β-tricalcium phosphate for mastoid obliteration in otitis media. Int J Pediatr Otorhinolaryngol. 2011; 75:631–634. PMID:
21388691.

38. Zijderveld SA, Zerbo IR, van den, Schulten EA, ten Bruggenkate CM. Maxillary sinus floor augmentation using a beta-tricalcium phosphate (Cerasorb) alone compared to autogenous bone grafts. Int J Oral Maxillofac Implants. 2005; 20:432–440. PMID:
15973955.
39. Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Worthington HV, Coulthard P. The efficacy of horizontal and vertical bone augmentation procedures for dental implants - a Cochrane systematic review. Eur J Oral Implantol. 2009; 2:167–184. PMID:
20467628.
40. Horch HH, Sader R, Pautke C, Neff A, Deppe H, Kolk A. Synthetic, pure-phase beta-tricalcium phosphate ceramic granules (Cerasorb) for bone regeneration in the reconstructive surgery of the jaws. Int J Oral Maxillofac Surg. 2006; 35:708–713. PMID:
16690249.

41. Horowitz RA, Mazor Z, Miller RJ, Krauser J, Prasad HS, Rohrer MD. Clinical evaluation alveolar ridge preservation with a beta-tricalcium phosphate socket graft. Compend Contin Educ Dent. 2009; 30:588–590. 592594 passimquiz 604, 606. PMID:
19998726.
42. Döri F, Arweiler N, Gera I, Sculean A. Clinical evaluation of an enamel matrix protein derivative combined with either a natural bone mineral or beta-tricalcium phosphate. J Periodontol. 2005; 76:2236–2243. PMID:
16332235.
43. Bokan I, Bill JS, Schlagenhauf U. Primary flap closure combined with Emdogain alone or Emdogain and Cerasorb in the treatment of intra-bony defects. J Clin Periodontol. 2006; 33:885–893. PMID:
17092241.
44. Harel N, Moses O, Palti A, Ormianer Z. Long-term results of implants immediately placed into extraction sockets grafted with β-tricalcium phosphate: a retrospective study. J Oral Maxillofac Surg. 2013; 71:e63–e68. PMID:
23351769.

45. Klein M, Goetz H, Pazen S, Al-Nawas B, Wagner W, Duschner H. Pore characteristics of bone substitute materials assessed by microcomputed tomography. Clin Oral Implants Res. 2009; 20:67–74.

46. Neamat A, Gawish A, Gamal-Eldeen AM. beta-Tricalcium phosphate promotes cell proliferation, osteogenesis and bone regeneration in intrabony defects in dogs. Arch Oral Biol. 2009; 54:1083–1090. PMID:
19828137.
47. Kasten P, Beyen I, Niemeyer P, Luginbühl R, Bohner M, Richter W. Porosity and pore size of beta-tricalcium phosphate scaffold can influence protein production and osteogenic differentiation of human mesenchymal stem cells: an in vitro and in vivo study. Acta Biomater. 2008; 4:1904–1915. PMID:
18571999.
48. Bernhardt A, Lode A, Peters F, Gelinsky M. Novel ceramic bone replacement material Osbone® in a comparative in vitro study with osteoblasts. Clin Oral Implants Res. 2011; 22:651–657. PMID:
21044164.

49. Bernhardt A, Dittrich R, Lode A, Despang F, Gelinsky M. Nanocrystalline spherical hydroxyapatite granules for bone repair: in vitro evaluation with osteoblast-like cells and osteoclasts. J Mater Sci Mater Med. 2013; 24:1755–1766. PMID:
23625348.

50. Klein MO, Kämmerer PW, Scholz T, Moergel M, Kirchmaier CM, Al-Nawas B. Modulation of platelet activation and initial cytokine release by alloplastic bone substitute materials. Clin Oral Implants Res. 2010; 21:336–345. PMID:
20074241.

51. Bernhardt A, Lode A, Peters F, Gelinsky M. Comparative evaluation of different calcium phosphate-based bone graft granules -an in vitro study with osteoblast-like cells. Clin Oral Implants Res. 2013; 24:441–449. PMID:
22092911.
52. Ghanaati S, Barbeck M, Orth C, Willershausen I, Thimm BW, Hoffmann C, et al. Influence of β-tricalcium phosphate granule size and morphology on tissue reaction in vivo. Acta Biomater. 2010; 6:4476–4487. PMID:
20624495.

53. Handschel J, Berr K, Depprich R, Naujoks C, Kübler NR, Meyer U, et al. Compatibility of embryonic stem cells with biomaterials. J Biomater Appl. 2009; 23:549–560. PMID:
18757497.

54. Zheng H, Bai Y, Shih MS, Hoffmann C, Peters F, Waldner C, et al. Effect of a β-TCP collagen composite bone substitute on healing of drilled bone voids in the distal femoral condyle of rabbits. J Biomed Mater Res B Appl Biomater. 2014; 102:376–383. PMID:
24039106.

55. Bizenjima T, Takeuchi T, Seshima F, Saito A. Effect of poly (lactide-co-glycolide) (PLGA)-coated beta-tricalcium phosphate on the healing of rat calvarial bone defects: a comparative study with pure-phase beta-tricalcium phosphate. Clin Oral Implants Res. 2016; 27:1360–1367. PMID:
26748831.

56. Bernhardt A, Lode A, Peters F, Gelinsky M. Optimization of culture conditions for osteogenically-induced mesenchymal stem cells in β-tricalcium phosphate ceramics with large interconnected channels. J Tissue Eng Regen Med. 2011; 5:444–453. PMID:
20848550.

57. Kurkcu M, Benlidayi ME, Cam B, Sertdemir Y. Anorganic bovinederived hydroxyapatite vs β-tricalcium phosphate in sinus augmentation: a comparative histomorphometric study. J Oral Implantol. 2012; 38:519–526. PMID:
23072285.

58. Khojasteh A, Eslaminejad MB, Nazarian H. Mesenchymal stem cells enhance bone regeneration in rat calvarial critical size defects more than platelete-rich plasma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:356–362. discussion 363. PMID:
18424120.

59. Badwelan M, Alkindi M, Ramalingam S, Nooh N, Al Hezaimi K. The efficacy of recombinant platelet-derived growth factor on beta-tricalcium phosphate to regenerate femoral critical sized segmental defects: longitudinal in vivo micro-CT study in a rat model. J Invest Surg. 2018; DOI:
10.1080/08941939.2018.1519048. [Epub ahead of print].

60. Giuliani A, Manescu A, Larsson E, Tromba G, Luongo G, Piattelli A, et al. In vivo regenerative properties of coralline-derived (biocoral) scaffold grafts in human maxillary defects: demonstrative and comparative study with beta-tricalcium phosphate and biphasic calcium phosphate by synchrotron radiation x-ray microtomography. Clin Implant Dent Relat Res. 2014; 16:736–750. PMID:
23350548.

61. Arbez B, Kün-Darbois JD, Convert T, Guillaume B, Mercier P, Hubert L, et al. Biomaterial granules used for filling bone defects constitute 3D scaffolds: porosity, microarchitecture and molecular composition analyzed by microCT and Raman microspectroscopy. J Biomed Mater Res B Appl Biomater. 2019; 107:415–423. PMID:
29675998.

62. Emanuel N, Rosenfeld Y, Cohen O, Applbaum YH, Segal D, Barenholz Y. A lipid-and-polymer-based novel local drug delivery system--BonyPid™: from physicochemical aspects to therapy of bacterially infected bones. J Control Release. 2012; 160:353–361. PMID:
22507550.

63. Catros S, Zwetyenga N, Bareille R, Brouillaud B, Renard M, Amédée J, et al. Subcutaneous-induced membranes have no osteoinductive effect on macroporous HA-TCP in vivo. J Orthop Res. 2009; 27:155–161. PMID:
18683892.

64. Salim AS, Al Hijazi A. Evaluation of the effect of synthetic biomaterial (calcium phosphate ceramic) on healing of extracted tooth socket. J Baghdad College Dent. 2010; 22:57–61.
65. Kursun-Çakmak ES, Akbulut N, Öztas DD. Comparative evaluation of the radiopacity of bone graft materials used in dentistry. J Contemp Dent. 2017; 7:150–155.

66. You H, Yoon SR, Lim HC, Lee JS, Jung UW, Choi SH. Bone regenerative efficacy of limited-dose escherichia coli-derived rh-BMP-2 with biphasic calcium phosphate carrier in rabbit calvarial defect model. Implant Dent. 2016; 25:16–23. PMID:
26606286.

67. Kumar A, Mahendra J, Samuel S, Govindraj J, Loganathan T, Vashum Y, et al. Platelet-rich fibrin/biphasic calcium phosphate impairs osteoclast differentiation and promotes apoptosis by the intrinsic mitochondrial pathway in chronic periodontitis. J Periodontol. 2019; 90:61–71. PMID:
29958327.

70. Lee MJ, Kim BO, Yu SJ. Clinical evaluation of a biphasic calcium phosphate grafting material in the treatment of human periodontal intrabony defects. J Periodontal Implant Sci. 2012; 42:127–135. PMID:
22977742.

71. Alagl AS, Madi M. Localized ridge augmentation in the anterior maxilla using titanium mesh, an alloplast, and a nano-bone graft: a case report. J Int Med Res. 2018; 46:2001–2007. PMID:
29529906.

72. Kim BS, Yang SS, You HK, Shin HI, Lee J. Fucoidan-induced osteogenic differentiation promotes angiogenesis by inducing vascular endothelial growth factor secretion and accelerates bone repair. J Tissue Eng Regen Med. 2018; 12:e1311–e1324. PMID:
28714275.

73. Yang DH, Park HN, Bae MS, Lee JB, Heo DN, Lee WJ, et al. Evaluation of GENESIS-BCP™ scaffold composed of hydroxyapatite and β-tricalcium phosphate on bone formation. Macromol Res. 2012; 20:627–633.

74. Kim BS, Lee J. Enhanced bone healing by improved fibrin-clot formation via fibrinogen adsorption on biphasic calcium phosphate granules. Clin Oral Implants Res. 2015; 26:1203–1210. PMID:
24888232.

75. Seok H, Lee SK, Kim SG, Kang TY, Lee MJ, Chae WS. Migration of alloplastic bone graft material in infected conditions: a case study and animal experiment. J Oral Maxillofac Surg. 2014; 72:1093.e1–1093.e11. PMID:
24709514.

76. Kim BS, Yang SS, Lee J. Precoating of biphasic calcium phosphate bone substitute with atelocollagen enhances bone regeneration through stimulation of osteoclast activation and angiogenesis. J Biomed Mater Res A. 2017; 105:1446–1456. PMID:
28177580.

77. Lee SH, Kim SW, Lee JI, Yoon HJ. The effect of platelet-rich fibrin on bone regeneration and angiogenesis in rabbit cranial defects. Tissue Eng Regen Med. 2015; 12:362–370.

78. Kim MS, Lee JH, Jung UW, Kim CS, Choi SH, Cho KS. A cumulative survival rate of implants installed on posterior maxilla augmented using MBCP after 2 years of loading: a retrospective clinical study. J Korean Acad Periodontol. 2008; 38:669–678.

79. Lee JH, Jung UW, Kim CS, Choi SH, Cho KS. Maxillary sinus augmentation using Macroporous Biphasic Calcium Phosphate (MBCP™): three case report with histologic evaluation. J Korean Acad Periodontol. 2006; 36:567–577.

80. Le Guehennec L, Goyenvalle E, Aguado E, Pilet P, Bagot D'Arc M, Bilban M, et al. MBCP biphasic calcium phosphate granules and tissucol fibrin sealant in rabbit femoral defects: the effect of fibrin on bone ingrowth. J Mater Sci Mater Med. 2005; 16:29–35. PMID:
15754141.

81. Lee JH, Jung UW, Kim CS, Choi SH, Cho KS. Histologic and clinical evaluation for maxillary sinus augmentation using macroporous biphasic calcium phosphate in human. Clin Oral Implants Res. 2008; 19:767–771. PMID:
18705808.

82. Wagner W, Wiltfang J, Pistner H, Yildirim M, Ploder B, Chapman M, et al. Bone formation with a biphasic calcium phosphate combined with fibrin sealant in maxillary sinus floor elevation for delayed dental implant. Clin Oral Implants Res. 2012; 23:1112–1117. PMID:
22892064.

83. Kim CS, Kim SC, Claire D, Elodie S, Daculsi G. Eight-year clinical follow-up of sinus grafts with micro-macroporous biphasic calcium phosphate granules. Key Eng Mater. 2014; 587:321–324.
84. Rodríguez C, Jean A, Mitja S, Daculsi G. Five years clinical follow up bone regeneration with CaP bioceramics. Key Eng Mater. 2008; 361-363:1339–1342.

85. Jégoux F, Goyenvalle E, Cognet R, Malard O, Moreau F, Daculsi G, et al. Reconstruction of irradiated bone segmental defects with a biomaterial associating MBCP+(R), microstructured collagen membrane and total bone marrow grafting: an experimental study in rabbits. J Biomed Mater Res A. 2009; 91:1160–1169. PMID:
19148925.
86. Miramond T, Aguado E, Goyenvalle E, Moreau F, Borget P, Daculsi G. Osteopromotion of biphasic calcium phosphate granules in critical size defects after osteonecrosis induced by focal heating insults. IRBM. 2013; 34:337–341.

87. Pereira RC, Benelli R, Canciani B, Scaranari M, Daculsi G, Cancedda R, et al. Beta tricalcium phosphate ceramic triggers fast and robust bone formation by human mesenchymal stem cells. J Tissue Eng Regen Med. 2019; DOI:
10.1002/term.2848. [Epub ahead of print].

88. Miramond T, Corre P, Borget P, Moreau F, Guicheux J, Daculsi G, et al. Osteoinduction of biphasic calcium phosphate scaffolds in a nude mouse model. J Biomater Appl. 2014; 29:595–604. PMID:
24919403.

89. Houshmand B, Tabibzadeh Z, Motamedian SR, Kouhestani F. Effect of metformin on dental pulp stem cells attachment, proliferation and differentiation cultured on biphasic bone substitutes. Arch Oral Biol. 2018; 95:44–50. PMID:
30048855.

90. Miramond T, Borget P, Baroth S, Daculsi G. Comparative critical study of commercial calcium phosphate bone substitutes in terms of physic-chemical properties. Key Eng Mater. 2014; 587:63–68.

91. Kim KI, Park S, Im GI. Osteogenic differentiation and angiogenesis with cocultured adipose-derived stromal cells and bone marrow stromal cells. Biomaterials. 2014; 35:4792–4804. PMID:
24655782.

92. Wang W, Yeung KWK. Bone grafts and biomaterials substitutes for bone defect repair: a review. Bioact Mater. 2017; 2:224–247. PMID:
29744432.
93. Habibovic P, Kruyt MC, Juhl MV, Clyens S, Martinetti R, Dolcini L, et al. Comparative in vivo study of six hydroxyapatite-based bone graft substitutes. J Orthop Res. 2008; 26:1363–1370. PMID:
18404698.

94. Kim YK, Yun PY, Kim SG, Lim SC. Analysis of the healing process in sinus bone grafting using various grafting materials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:204–211. PMID:
18801669.

95. Lim HC, Kim KT, Lee JS, Jung UW, Choi SH. In vivo comparative investigation of three synthetic graft materials with varying compositions processed using different methods. Int J Oral Maxillofac Implants. 2015; 30:1280–1286. PMID:
26574853.

96. Lim HC, Zhang ML, Lee JS, Jung UW, Choi SH. Effect of different hydroxyapatite:β-tricalcium phosphate ratios on the osteoconductivity of biphasic calcium phosphate in the rabbit sinus model. Int J Oral Maxillofac Implants. 2015; 30:65–72. PMID:
25265122.

97. Kim DM, Nevins ML, Lin Z, Fateh A, Kim SW, Schupbach P, et al. The clinical and histologic outcome of dental implant in large ridge defect regenerated with alloplast: a randomized controlled preclinical trial. J Oral Implantol. 2013; 39:148–153. PMID:
23611677.

98. Lim HC, Hong JY, Lee JS, Jung UW, Choi SH. Late-term healing in an augmented sinus with different ratios of biphasic calcium phosphate: a pilot study using a rabbit sinus model. J Periodontal Implant Sci. 2016; 46:57–69. PMID:
26937294.

99. Abdulghani MM, Farha LS. Clinical and experimental study to evaluate the effect of biphasic calcium phosphate collagen composite (cpcc) on healing of bone defects after oral surgical procedures. Al-Kindy College Med. 2017; 13:11–20.
100. Hussein LA, Hassan TAL. The effectiveness of oxidized regenerated cellulose as a graft material in transalveolar osteotome sinus lift procedure. J Craniofac Surg. 2017; 28:1766–1771. PMID:
28891903.

101. Park YH, Choi SH, Cho KS, Lee JS. Dimensional alterations following vertical ridge augmentation using collagen membrane and three types of bone grafting materials: a retrospective observational study. Clin Implant Dent Relat Res. 2017; 19:742–749. PMID:
28556452.

102. Kim DM, Camelo M, Nevins M, Fateh A, Schupbach P, Nevins M. Alveolar ridge reconstruction with a composite alloplastic biomaterial. Int J Periodontics Restorative Dent. 2012; 32:e204–e209. PMID:
23057064.
103. Chee YD, Seon HK. Increase of the width of peri-implant keratinized tissue using apically positioned flap: case report. J Dent Rehabil Appl Sci. 2013; 29:407–417.

104. Lee JB. Selectable implant removal methods due to mechanical and biological failures. Case Rep Dent. 2017; 2017:9640517. PMID:
28758035.

105. Badiea RA. Evaluation of treatment of intra-bony defects with a mixture of β-tricalcium phosphate - hydroxyapatite granules and oily calcium hydroxide suspension. J Baghdad College Dent. 2013; 25:103–109.
106. Seo GY, Thoma DS, Jung UW, Lee JS. Increasing the tissue thickness at implant sites using guided bone regeneration and an additional collagen matrix: histologic observations in beagle dogs. J Biomed Mater Res B Appl Biomater. 2019; 107:741–749. PMID:
30080303.

107. Bucchi C, Borie E, Arias A, Dias FJ, Fuentes R. Radiopacity of alloplastic bone grafts measured with cone beam computed tomography: an analysis in rabbit calvaria. Bosn J Basic Med Sci. 2016; 17:61–66. PMID:
27968706.

108. Chung SM, Jung IK, Yoon BH, Choi BR, Kim DM, Jang JS. Evaluation of different combinations of biphasic calcium phosphate and growth factors for bone formation in calvarial defects in a rabbit model. Int J Periodontics Restorative Dent. 2016; 36(Suppl):s49–s59. PMID:
27031634.

109. Al Mukhtar YH, Abid WK. Effect of Osteon II collagen with hyaluronic acid and collagen membrane on bone healing process in rabbits: a radiograghical study. Int J Enhanc Res Sci Tech Eng. 2016; 5:36–46.
110. Khojasteh A, Motamedian SR, Rad MR, Shahriari MH, Nadjmi N. Polymeric vs hydroxyapatite-based scaffolds on dental pulp stem cell proliferation and differentiation. World J Stem Cells. 2015; 7:1215–1221. PMID:
26640621.
111. Tallarico M, Xhanari E, Cocchi F, Canullo L, Schipani F, Meloni SM. Accuracy of computer-assisted template-based implant placement using a conventional impression and scan model or digital impression: a preliminary report from a randomized controlled trial. J Oral Sci Rehabil. 2017; 3:8–16.
112. Kang KJ, Lee MS, Moon CW, Lee JH, Yang HS, Jang YJ. In vitro and in vivo dentinogenic efficacy of human dental pulp-derived cells induced by demineralized dentin matrix and HA-TCP. Stem Cells Int. 2017; 2017:2416254. PMID:
28761445.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download