II. Case Report
A 51-year-old male patient was admitted to the Department of Oral and Maxillofacial Surgery at Pusan National University Dental Hospital (Yangsan, Korea) for pain and discomfort in the mandibular anterior region. The patient did not manifest any underlying disorders or noticeable lab results except controlled hypertension.
Under routine clinical examination, the patient reported pain and light mobility in four mandibular anterior teeth. Panoramic radiography and cone-beam computed tomography (CT) revealed an irregular 38×31 mm lesion of the mandibular anterior region.(
Fig. 1) Because radiologic findings did not provide conclusive evidence for diagnosis, incisional biopsy was conducted under local anesthesia. Based on histopathologic examination conducted at the Department of Pathology of Pusan National University Yangsan Hospital, the lesion was diagnosed as ameloblastoma.(
Fig. 2)
Given the aggressive behavior of ameloblastoma, excision and mandibular reconstruction with iliac-block bone were performed under general anesthesia.(
Fig. 3) The main mass from surgery was determined by Department of Pathology staff to be poorly differentiated ameloblastic carcinoma. However, the clinical features of the main mass did not correspond to those of a poorly differentiated ameloblastic carcinoma. The authors requested a histopathologic examination by the Department of Oral Pathology at Pusan National Dental University for more accurate analysis. Given the presence of multiple clear cells and clinical features, CCOC was the final diagnosis.(
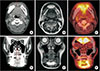
Fig. 4) After a one-month-long healing period, CT, magnetic resonance imaging, and positron emission tomography-CT scans were performed.(
Fig. 5) A segmental mandibulectomy in the anterior region was performed along with bilateral neck dissection, followed by reconstruction with a right fibular free flap. Supraomohyoid neck dissection included levels I to III on the right and levels I and II on the left. Frozen biopsy on the margins of the lesion presented normal tissue findings. Permanent biopsy results produced negative findings from the margins and suspected neck areas for possible metastasis, with the exception of the resection area. The surgical site exhibited positive recovery, requiring neither adjuvant chemotherapy nor radiotherapy. Continuous follow-up for seven months after surgery found no evidence of recurrence.(
Fig. 6)
IV. Discussion
CCOC is a rare odontogenic tumor that shows distinctive vacuolated clear cells. According to previous studies, it is most frequently seen in female patients, especially those in middle age
3. Various clinical symptoms have been reported, including pain, distressing jaw enlargement, cortical bone damage, paresthesia, tooth mobility, and root resorption
4. According to a recent, systematic review of CCOC patients, recurrence and metastasis are often observed
5. Approximately 41% of patients experienced a local recurrence, 19% showed a regional metastasis to a level I lymph node, and 11.9% presented a distant metastasis, mostly to a lung. The morality rate was 14.3%, while survival rates at 5, 10, and 20 years were 87%, 76%, and 46%, respectively. Although the first report on CCOC was published more than 30 years ago, disease etiology and predictive factors of cell differentiation remain poorly understood.
Differentiating CCOC from other diseases on a histological basis may be challenging. The histological patterns of CCOC include biphasic, monophasic, and ameloblastomatous variants
6. The biphasic pattern, the most common variant, is associated with nests of clear cells integrated with islands of eosinophilic, polygonal epithelial cells. The monophasic pattern contains nests and cords of clear cells only. The ameloblastomatous pattern, the least common variant, resembles ameloblastomas that occasionally include palisading, peripheral clear cells
78910.
Recently, a DNA microarray technique has allowed for more accurate diagnosis of CCOC through genetic profiling. Some studies have reported that frequent fission of the EWSR1 gene can provide a basis for diagnosis, as 83.3% of CCOCs manifest such genetic expresion, commonly with ATF1
11. However, clear cell carcinoma of minor salivary glands is also associated with such distinct characteristics, making it difficult to distinguish between CCOC and clear cell carcinoma of minor salivary glands
511. Immunohistochemistry may be beneficial in this respect, as CCOC presents negative results for vimentin and muscle actin, while clear cell salivary gland tumors react positively with vimentin, muscle actin, cytokeratin, and S-100 protein
1213. Even in cases of biphasic-pattern CCOC, differentiating it from metastatic renal cell carcinoma may be difficult without incorporating the glycogen-negative tendency of CCOC
814.A few other tumors, including ameloblastomas, ameloblastic carcinomas, calcifying epithelial odontogenic tumors, infected cysts, and squamous cell carcinomas, also involve differential diagnostic problems requiring accurate and reliable diagnostic criteria of CCOC
1516.
In this case, diagnosis of a malignant tumor was initially based on clinical and radiographic findings, but the lesion was later classified as ameloblastoma through incisional biopsy. The tissue displayed multiple clear cells, and an ameloblastic pattern was weakly observed. However, differential diagnosis of CCOC may be difficult due to its infrequency. Moreover, ameloblastic-pattern CCOC is uncommon, leading to misdiagnosis by unexperienced pathologists. Based on histopathologic findings, the authors considered the lesion an aggressive benign tumor, and the initial surgery was performed accordingly. However, during the operation, adhesion of the lesion to genioglossus muscle was observed, and bone destruction was more aggressive than expected. After histopathological reinvestigation, and considering the intraosseous origin of bone destruction, we determined the mass as CCOC. Ameloblastic carcinoma was one of our differential diagnoses, but CCOC was more plausible due to clear cell portions and less ameloblastic differentiation. Other considerations included clear cell carcinoma of the salivary gland and possible metastasis from renal cell carcinoma. The intraosseous origin of the lesion and immunohistochemical findings helped exclude a salivary gland tumor, and the histological appearance and vascularity pattern made the lesion distinguishable from metastasis of renal cell carcinoma.
Various treatment protocols for CCOC have been suggested in previous studies. Conservative approaches, such as curettage and enucleation, were followed until CCOC was reclassified as a malignancy, at which time many surgeons began performing wide surgical excision. Depending on lymph node involvement, neck dissection and surgical resection with a wide safety margin are now the gold standard for CCOC treatment
1718. A recurrence rate of 40% and a lymph node involvement rate of 10% have been reported
57. Adjuvant therapy is not required in many cases, and lesion size and location, aggressiveness, and positive margin of resection must be considered beforehand
91718. In this case, the patient underwent both surgical resection with neck dissection and mandibular reconstruction with the fibular free flap. Because neither frozen biopsy of resection margins nor biopsy of the neck region showed a positive result, adjuvant therapy was not required.
A follow-up assessment for high-grade oral tumors was ordered due to the high recurrence rate of CCOC. In addition, long-term follow-up is mandatory for potential recurrence after as long as 20 years
5. Patients should be well informed and understand the necessity for follow-up visits and management.
Because an unsuitable treatment protocol based on misdiagnosis from the initial assessment was followed, a second surgical interference for the intraosseous carcinoma was inevitable in this case. Prognosis was optimistic as the correct diagnosis was made within a short time and the proper surgical treatment was applied. However, if the first diagnosis had been accurate, the patient would not have undergone additional surgery, and his prognosis would have been more favorable. We conclude that, if malignant tendency of a lesion is recognized at first diagnosis, circumspective investigation of the specimen by an adept pathologist should be requested to establish an accurate diagnosis and choose the appropriate therapeutic approach.








 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download