1. Otrock ZK, Eby CS. Clinical characteristics, prognostic factors, and outcomes of adult patients with hemophagocytic lymphohistiocytosis. Am J Hematol. 2015; 90:220–224. PMID:
25469675.
2. McCall CM, Mudali S, Arceci RJ, Small D, Fuller S, Gocke CD, et al. Flow cytometric findings in hemophagocytic lymphohistiocytosis. Am J Clin Pathol. 2012; 137:786–794. PMID:
22523218.
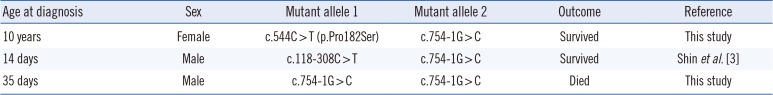
3. Shin SY, Lee K, Jang MA, Lee ST, Yoo KH, Koo HH, et al. First report on familial hemophagocytic lymphohistiocytosis with an abnormal immunophenotype and T cell monoclonality in Korea. Ann Lab Med. 2015; 35:155–158. PMID:
25553300.
4. Wada T, Sakakibara Y, Nishimura R, Toma T, Ueno Y, Horita S, et al. Down-regulation of CD5 expression on activated CD8+ T cells in familial hemophagocytic lymphohistiocytosis with perforin gene mutations. Hum Immunol. 2013; 74:1579–1585. PMID:
24051121.
5. Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007; 48:124–131. PMID:
16937360.
6. Stevens SJ, Pronk I, Middeldorp JM. Toward standardization of Epstein-Barr virus DNA load monitoring: unfractionated whole blood as preferred clinical specimen. J Clin Microbiol. 2001; 39:1211–1216. PMID:
11283029.
7. Jamal S, Picker LJ, Aquino DB, McKenna RW, Dawson DB, Kroft SH. Immunophenotypic analysis of peripheral T-cell neoplasms. A multiparameter flow cytometric approach. Am J Clin Pathol. 2001; 116:512–526. PMID:
11601136.
8. Brisse E, Wouters CH, Matthys P. Advances in the pathogenesis of primary and secondary haemophagocytic lymphohistiocytosis: differences and similarities. Br J Haematol. 2016; 174:203–217. PMID:
27264204.
9. Ishii E. Hemophagocytic lymphohistiocytosis in children: pathogenesis and treatment. Front Pediatr. 2016; 4:47. PMID:
27242976.
10. Sieni E, Cetica V, Mastrodicasa E, Pende D, Moretta L, Griffiths G, et al. Familial hemophagocytic lymphohistiocytosis: a model for understanding the human machinery of cellular cytotoxicity. Cell Mol Life Sci. 2012; 69:29–40. PMID:
21990010.
11. Sieni E, Cetica V, Hackmann Y, Coniglio ML, Da Ros M, Ciambotti B, et al. Familial hemophagocytic lymphohistiocytosis: when rare diseases shed light on immune system functioning. Front Immunol. 2014; 5:167. PMID:
24795715.
12. Yoon HS, Kim HJ, Yoo KH, Sung KW, Koo HH, Kang HJ, et al.
UNC13D is the predominant causative gene with recurrent splicing mutations in Korean patients with familial hemophagocytic lymphohistiocytosis. Haematologica. 2010; 95:622–626. PMID:
20015888.
13. Koh KN, Im HJ, Chung NG, Cho B, Kang HJ, Shin HY, et al. Clinical features, genetics, and outcome of pediatric patients with hemophagocytic lymphohistiocytosis in Korea: report of a nationwide survey from Korea Histiocytosis Working Party. Eur J Haematol. 2015; 94:51–59. PMID:
24935083.
14. Manji F, Wilson E, Mahe E, Gill J, Conly J. Acute HIV infection presenting as hemophagocytic lymphohistiocytosis: case report and review of the literature. BMC Infect Dis. 2017; 17:633. PMID:
28931369.
15. Brisse E, Wouters CH, Andrei G, Matthys P. How viruses contribute to the pathogenesis of hemophagocytic lymphohistiocytosis. Front Immunol. 2017; 8:1102. PMID:
28936212.
16. Marsh RA. Epstein-Barr virus and hemophagocytic lymphohistiocytosis. Front Immunol. 2017; 8:1902. PMID:
29358936.
17. Ishii E, Ohga S, Imashuku S, Yasukawa M, Tsuda H, Miura I, et al. Nationwide survey of hemophagocytic lymphohistiocytosis in Japan. Int J Hematol. 2007; 86:58–65. PMID:
17675268.
18. Imashuku S. Clinical features and treatment strategies of Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis. Crit Rev Oncol Hematol. 2002; 44:259–272. PMID:
12467966.
19. Kawa K. Epstein-Barr virus--associated diseases in humans. Int J Hematol. 2000; 71:108–117. PMID:
10745621.
20. Dojcinov SD, Fend F, Quintanilla-Martinez L. EBV-positive lymphoproliferations of B- T- and NK-cell derivation in non-immunocompromised hosts. Pathogens. 2018; 7.
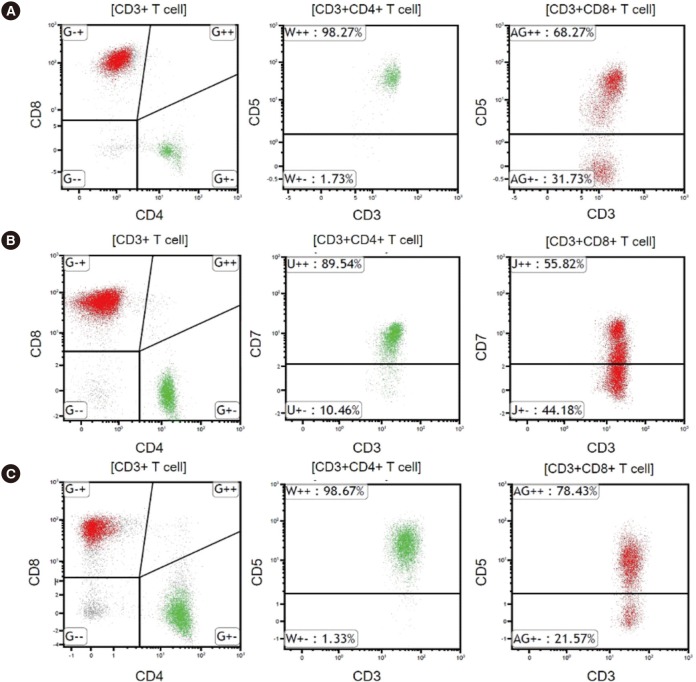
21. Lin MT, Chang HM, Huang CJ, Chen WL, Lin CY, Lin CY, et al. Massive expansion of EBV+ monoclonal T cells with CD5 down regulation in EBV-associated haemophagocytic lymphohistiocytosis. J Clin Pathol. 2007; 60:101–103. PMID:
17213357.
22. Weisberger J, Cornfield D, Gorczyca W, Liu Z. Down-regulation of pan-T-cell antigens, particularly CD7, in acute infectious mononucleosis. Am J Clin Pathol. 2003; 120:49–55. PMID:
12866372.
23. Wada T, Kurokawa T, Toma T, Shibata F, Tone Y, Hashida Y, et al. Immunophenotypic analysis of Epstein-Barr virus (EBV)-infected CD8(+) T cells in a patient with EBV-associated hemophagocytic lymphohistiocytosis. Eur J Haematol. 2007; 79:72–75. PMID:
17532761.
24. Karandikar NJ, Kroft SH, Yegappan S, Rogers BB, Aquino VM, Lee KM, et al. Unusual immunophenotype of CD8+ T cells in familial hemophagocytic lymphohistiocytosis. Blood. 2004; 104:2007–2009. PMID:
15205266.
25. Toga A, Wada T, Sakakibara Y, Mase S, Araki R, Tone Y, et al. Clinical significance of cloned expansion and CD5 down-regulation in Epstein-Barr Virus (EBV)-infected CD8+ T lymphocytes in EBV-associated hemophagocytic lymphohistiocytosis. J Infect Dis. 2010; 201:1923–1932. PMID:
20443735.
26. Manno EC, Salfa I, Palma P, Bertaina A, Lombardi A, Moretta F, et al. Familial hemophagocytic lymphohistiocytosis type 3 diagnosed at school age: a case report. J Pediatr Hematol Oncol. 2014; 36:e128–e130. PMID:
23669735.
27. Tembhare P, Yuan CM, Xi L, Morris JC, Liewehr D, Venzon D, et al. Flow cytometric immunophenotypic assessment of T-cell clonality by Vbeta repertoire analysis: detection of T-cell clonality at diagnosis and monitoring of minimal residual disease following therapy. Am J Clin Pathol. 2011; 135:890–900. PMID:
21571962.
28. Mehta RS. Hemophagocytic lymphohistiocytosis (HLH): a review of literature. Medical Oncology. 2013; 30:740. PMID:
24105023.
29. Imashuku S, Teramura T, Tauchi H, Ishida Y, Otoh Y, Sawada M, et al. Longitudinal follow-up of patients with Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis. Haematologica. 2004; 89:183–188. PMID:
15003893.
30. Ohga S, Kudo K, Ishii E, Honjo S, Morimoto A, Osugi Y, et al. Hematopoietic stem cell transplantation for familial hemophagocytic lymphohistiocytosis and Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis in Japan. Pediatr Blood Cancer. 2010; 54:299–306. PMID:
19827139.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download