This article has been
cited by other articles in ScienceCentral.
Abstract
Iatrogenic injuries due to intramuscular (IM) injection, although less frequently reported than before, are still common. The sciatic nerve is the most commonly injured nerve because of an IM injection owing to its large size and the buttock being a common injection site. Iatrogenic injury to the sciatic nerve resulting from a misplaced gluteal IM injection is a persistent problem worldwide affecting patients in economically rich and poor countries alike. The consequences of sciatic nerve injection injury (SNII) are potentially devastating and may result in serious neurological and medico-legal problems. A 68-year-old male presented with intractable neuropathic pain from SNII that occurred during gluteal IM injection of an analgesic for post-appendectomy pain. This chronic SNII pain did not improve despite his gradual recovery from weakness in the left foot. Partial improvement was seen following an external neurolysis, performed three months post-appendectomy. SNII is a preventable complication of gluteal IM injection. While the complete avoidance of gluteal IM injection is desirable, should need arise, the use of an appropriate administrative technique is recommended.
Go to :

Keywords: Intramuscular injections, Iatrogenic nerve injury, Neurolysis, Neuropathic pain, Sciatic nerve
INTRODUCTION
Intramuscular (IM) injection is an important means of administering medications. However, iatrogenic nerve injury has long been recognized as a common complication of IM injection.
1) The sciatic nerve is the most commonly injured nerve following IM injection because of its large size and the fact that the buttock is a common injection site.
2345) Although the incidence of sciatic nerve injection injury (SNII) has decreased over the last few decades,
3) it remains a persistent world-wide problem that affects patients in both wealthy and poorer healthcare systems.
24)
The presentations of SNIIs may range from minor transient pain to severe sensory disturbance and motor loss with poor recovery.
347) A serious medicolegal claim may ensue.
4) The pathophysiology of IM injection injury varies depending on both the injection site and the agent injected.
9) An intrafascicular injection may result in severe nerve damage depending on both the agent used and the dosage.
489) Many patients who experience such damage fail to make a full recovery, even with microsurgical repair.
3510) Affected patients typically experience immediate pain radiating down the limb, with weakness and numbness evolving more gradually and exacerbated by secondary scarring.
48) Pain following injury to a nerve is remarkable in its severity, its intractability, and in the consistency of its features, all of which should lead directly to a diagnosis.
11) SNII may result in excruciating and incapacitating pain that is resistant to analgesia.
4511)
We report a 68-year-old male who patient presented with chronic intractable neuropathic pain from SNII that occurred during gluteal IM injection of an analgesic for post-appendectomy pain. The patient's chronic neuropathic pain was partially improved with an external neurolysis performed at three months postoperatively. SNII is a preventable complication of gluteal IM injection.
347) While total avoidance of gluteal IM injection is desirable, if a gluteal injection is necessary, the use of an appropriate administrative technique is recommended.
347)
Go to :

CASE REPORT
A 68-year-old male patient presented with gait disturbance due to weakness of his left leg and foot as well as severe aching and electrical-shooting pain along his left posterolateral thigh, leg, and foot, all of a 3-month duration. Three months prior, he had undergone an appendectomy for abdominal pain. At 3 days postoperative, he asked a nurse for pain control because of gradually developing abdominal pain. During an IM injection of an analgesic medication in his left buttock, a severe electric shock-like pain developed. Despite reporting a severe electrical shock-like pain in his leg during this IM injection, the nurse reassured him that it would be okay. Three hours later, the patient found that he could not walk due to weakness in his left foot. Severe aching and electricity-like pain developed in his left posterolateral thigh, leg, and foot. The doctor in charge and nurse admitted that the IM injection in the left buttock injured his left sciatic nerve. They recommended conservative treatment with medical and rehabilitation therapies.
With physical therapy, the weakness in his left leg and foot improved progressively within a month. He had begun to walk again despite residual weakness of flexion in his left knee, ankle, and toes. Despite the gradual improvement of the patient's left leg and foot, the severe aching and electricity-like pain did not respond to any medical treatment, including gabapentin, pregabalin, tramadol, oxycontin, and amitriptyline. The application of transdermal fentanyl showed a side effect of dizziness and was discontinued. He was then referred to our senior author (Byung-chul Son) for the management of the continuous disabling pain in his left leg and foot. The patient had undergone bilateral total hip replacement for avascular necrosis of the head of the femur seven year prior to the accident. His family and medical history were unremarkable, including diabetes and a thyroid problem.
The patient was thin (body mass index, 16.29 kg/m
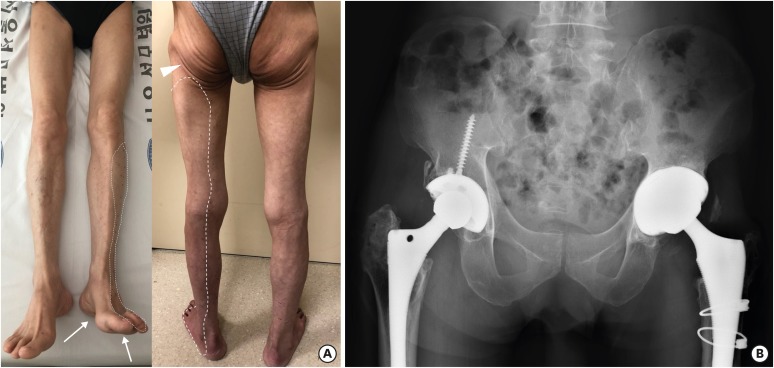
2) and his bilateral buttock was atrophied following bilateral total hip arthroplasty (
FIGURE 1). Upon examination, atrophy of the muscles of the posterior thigh and calf, as well as some degree of calcaneovalgus deformity was evident with toe claws. No weakness in the ankle dorsiflexion and eversion in his left foot was found. However, plantar flexion, foot inversion, and toe flexion showed significant weakness (NMT grade II). Deep tendon reflex was diminished in his left ankle. Hypesthesia and paresthesia were present on the left posterolateral thigh, leg, and foot (
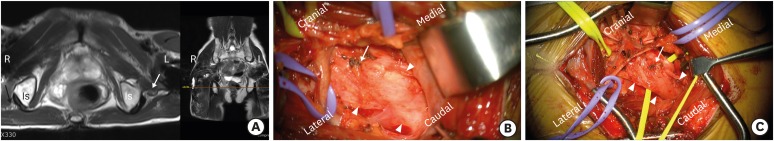
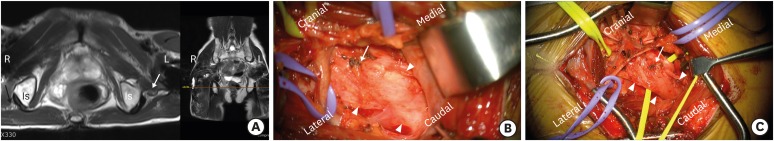
FIGURE 1A). The pain in his leg was described as mainly aching and electric-shock-like with moderate to severe severity (5–8/10 on numerical rating scale [NRS]-11 ranging from 0 to 10). A constant and intermittent attack of electric shock-like pain occurred spontaneously every 10 minutes. Magnetic resonance imaging of the pelvis revealed a high signal intensity and swelling of the left sciatic nerve (
FIGURE 2A). Diffuse atrophic changes in the muscles of the left hip and thigh were observed. Electromyography showed an incomplete sciatic nerve injury more severely involving the tibial division. Considering the chronicity and medical intractability of his leg pain, exploration, and neurolysis were recommended.
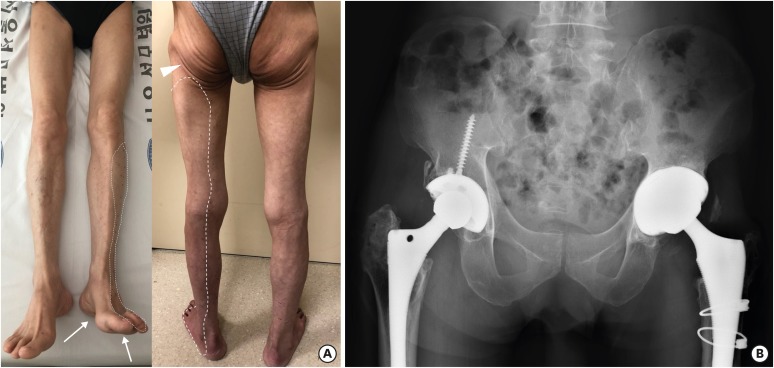 | FIGURE 1 (A) Anterior-posterior photographs of patient with left sciatic nerve injection injury. His left foot shows calcaneal position (arrows) indicating more severe involvement of the tibial division. Atrophy of the gluteal muscles in the buttock is evident due to previous total hip atrophy. The arrowhead indicates the site of injection. The dotted area shows the area of aching and electrical shock-like pain, hypesthesia, and dysesthesia. (B) X-ray film showing bilateral total hip arthroplasty.
|
 | FIGURE 2
(A) An axial T2-weighted image of the pelvis showing the right and left sciatic nerves. Compared to the right sciatic nerve (black arrow), the left sciatic nerve is atrophic and does not show a normal reticular pattern. (B) An intraoperative photograph showing the adhesion and scarring around the left sciatic nerve (arrowheads). The left sciatic nerve was pale and swollen. The arrow indicates the site of the misplaced IM injection. (C) An intraoperative photograph after decompression and external neurolysis of the left sciatic nerve (arrowheads). The arrow indicates the site of the misplaced IM injection.
Is: ischial spine, L: left, R: right, IM: intramuscular.

|
Exploration of the left sciatic nerve at the buttock was performed via a transgluteal approach. After transverse dissection of the gluteus maximus muscle, the underlying course of the sciatic nerve was addressed under microscopic vision. The sciatic nerve was severely entrapped by the surrounding whitish adhesion, so it was carefully dissected free (
FIGURE 2B). The proximal course of the sciatic nerve underneath the piriformis muscle was dissected as well. A small adhesion scar severing the integrity of sciatic nerve, which was an inadvertent IM injection point, was found in the dorsal side of the sciatic nerve, and the adhesion was carefully dissected free (
FIGURE 2C). External neurolysis of the sciatic nerve was then performed.
Immediately following the external neurolysis, the intermittent attacks of electrical shock-like pain disappeared. However, the constant aching and electrical pain did not change, nor did the weakness in his left foot. There was no change in the sensory examination. The residual weakness and continuous pain in his left leg and foot did not show any change at a six-month postoperative follow-up. He himself assessed the surgery to be successful in relieving repeated bouts of electrical shock-like pain. However, his NRS-11 was 4–5/10 at the last follow-up.
Go to :

DISCUSSION
Sciatic nerve and intramuscular injection injury
The sciatic nerve is the nerve most frequently affected by IM injection because of its large size and the fact that the buttock area is a common injection site.
6) SNII is most prevalent in newborn children, the elderly (>75 years of age), and underweight patients.
567) Injection is the most common injury mechanism affecting the sciatic nerve at the buttock level.
5) According to Kline et al.,
5) injection is the most common injury mechanism affecting the sciatic nerve at the buttock level, accounting for more than half of the cases (136/230 patients) examined in their 24-year study. Younger age groups (<1 year of age) may be particularly at risk of SNII due to their smaller gluteal covering and volume of gluteal mass to the size of the sciatic nerve.
1013) Older patients who are thin and emaciated as well as those with debilitating diseases also have a predisposition to SNII, because they have a smaller amount of gluteal soft-tissue covering than do other people.
514)
The sciatic nerve is formed from the anterior and posterior divisions of the L4, L5, S1, and S2 spinal nerves, and the anterior division of the S3 spinal nerve. The anterior divisions form the tibial division of the sciatic nerve, while the posterior divisions form the peroneal nerve. The two divisions usually run together in the pelvis, then pass beneath the piriformis muscle, with the peroneal division lying lateral to the tibial division.
512) The sciatic nerve is located in the middle of the gluteal region and usually passes deep to the piriformis muscle. IM injection outside of the upper quadrant of the buttock (dorsogluteal region) is a major cause of SNII, with the sciatic nerve being more prone to damage when the injection site is more medial and/or inferior.
7) The peroneal division of the sciatic nerve is more frequently injured than the tibial division because of its more lateral position, as well as the relative tethering of the nerve course.
5813) Anatomical variations of the nerves and the piriformis, such as an absence of (or abnormal subdivision of) the piriformis muscle, as well as the passing of the peroneal division through the piriformis muscle, may be associated with SNII.
810)
Pathophysiology of injection injury to the nerve
SNII may occur with various therapeutics and agents.
15) The most common IM injection agents that were injected into the nerve were a combination of analgesic and antiemetic drugs. Other agents include antibiotic and local anesthetic medications, vitamin preparations, vaccines, and even steroid drugs.
5) The postulated mechanisms of injury include direct needle trauma, secondary constriction by scar, and neurotoxicity of the agent injected.
16) Direct intrafascicular injection of the medications can result in varying degrees of axonal and myelin degeneration, depending on both the agent injected and dose of the drug used.
916) However, the anatomical proximity of the injection to the nerve is considered to be the single most crucial factor in determining the degree of nerve damage, with injection directly into the nerve being the most destructive mechanism.
5)
The clinical findings of SNII are characteristic.
517) Typically, needle placement results in an immediate electric-like shock sensation down the extremity. Concomitantly, upon injection of the agent, the most frequent presentation included severe radicular pain and paresthesia, with almost immediate onset of variable motor and sensory deficits.
516) The patient usually experienced a severe pain, described as the occurrence of burning, searing, electricity, or numbness along the course of the affected area.
17) In about 10% of cases, a delayed onset of pain and paresthesia and/or progressive loss of motor function appeared minutes to hours following injection.
5) This may be related to the placement of injection being either adjacent to the nerve or into the epineurium.
5) Damage to the sciatic nerve can produce effects ranging from minor motor and sensory abnormalities to complete paralysis and causalgia, an excruciating and incapacitating pain that is resistant to analgesic treatment.
5) In the case of a complete lesion, the motor loss is usually greater than the sensory loss.
17)
Treatment of SNII
Electrodiagnostic studies including nerve conduction studies and electromyography studies are invaluable in defining the location and grading the severity of injection injury and predicting recovery.
512141617) Like other kinds of traumatic peripheral nerve injury, the differentiation of neuropraxia from neurotmesis and axonotmesis is crucial.
518)
It is generally recommended to wait for three to six months before surgical exploration if the injury is not severely incapacitating and the pain is minimal.
513) Neuropraxia carries a good prognosis, but if the diagnosis is in doubt, any delay may cause continued compression or ischemia, thus extending the lesion to axonotmesis or even neurotmesis.
19) Early exploration has been suggested for persistent and intractable pain, or with clinical evidence of neurotmesis and a lack of recovery from presumed axonotmesis at the predicted time and deterioration of the lesion while the patient is under observation.
11) By means of early exploration, any constricting or deforming agent could be removed through irrigation and early decompression. Simple neurolysis is performed in cases of compression by hematoma or stricture by scar tissue.
11) In the current case, neuropathic pain due to SNII was remarkable and early decompression with external neurolysis was performed. The constriction and entrapping scar were removed, which resulted in the alleviation of intermittent electrical shock-like pain. During surgical exploration, the importance of the presence/absence of the nerve action potential distal to the injury site has been stressed.
5) If nerve action potential is present beyond the lesion, external neurolysis alone or with internal neurolysis is indicated. However, if there is no nerve action potential beyond the lesion, suture or graft repair is required.
5101213)
Go to :

CONCLUSION
A patient suffering chronic neuropathic pain from injury to the sciatic nerve caused by misplaced IM injection is reported. SCII is still common and can result in serious neurologic sequela. Attention must be paid to avoiding iatrogenic nerve injuries by IM injection in the medical and nursing fields.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download