This article has been
cited by other articles in ScienceCentral.
Abstract
A case of acute quadriplegia resulting from reduction of atlantoaxial subluxation due to os odontoideum is rare. Patient with os odontoideum are at a greater risk for atlantoaxial instability and resultant spinal cord compression. In our case, the patient exhibited mild myelopathic symptoms before the onset of acute quadriplegia. Owing to the clinical presentations, the spinal cord not only seemed to suffer a mechanical compression but also an insufficiency of blood supply to the spinal artery and its branches. No other report has described the findings from magnetic resonance imaging before and after the onset of acute myelopathy after surgery. The aim of our case report is to highlight the pathophysiology and appropriate management strategy of a patient with severe progressive spinal cord myelopathy after surgery, secondary to chronic atlantoaxial subluxation due to os odontoideum. This case depicts the presence of this rare yet possible complication, and emphasizes the importance of preoperative evaluation in cases with chronic progressive myelopathy. Moreover, urgent postoperative treatment and rehabilitation are important for the recovery of neurological symptoms.
Go to :

Keywords: Quadriplegia, Myelopathy, Rehabilitation
INTRODUCTION
Os odontoideum is an independent ossicle with smooth circumferential cortical margins that stands apart from a hypoplastic dens. Since it was first described as early as 1886, there has been controversial about its etiology.
157) There are 2 main theories about os odontoideum. One suggests that it is a congenital lesion, whereas the second claims that it is acquired after trauma. Regardless of the etiology, patients with os odontoideum are at greater risk for atlantoaxial instability and resultant spinal cord. Also, acute progression of myelopathy into quadriplegia resulting from after treatment of os odontoideum is rare. No other report has described magnetic resonance imaging (MRI) findings noted before and after the onset of acute myelopathy after surgery. This report describes a rare case of quadriplegia resulting from reduction of atlantoaxial subluxation due to os odontoideum and to highlight appropriate management and etiology of a patient with severe spinal cord myelopathy after reduction and decompression secondary to chronic atlantoaxial subluxation due to os odontoideum.
Go to :

CASE REPORT
A 33-year-old woman presented with neck pain and progressive myelopathic symptom. She reported significant falling injury as a child. At presentation, she had slowly progressive numbness in both arms and legs. On examination, she had a history of many years of previously uninvestigated occipital pain, but was otherwise well. A neurological examination detected no motor weakness of either upper or lower extremities other severity. But she had a Hoffman's reflex on the right and bilateral finger jerks, hypesthesia on the upper extremity. She held her neck stiffly to minimize her symptoms. Dynamic X-rays and cervical computed tomography (CT) showed an atlanto-axial instability in flexion and extension and revealed a dystopic os odontoideum with 10 mm of sagittal atlanto-axial instability as well as a few millimeters of lateral atlantoaxial subluxation (
FIGURE 1). The minimal canal diameter was 8.5 mm. The C1/2 interlaminar space was widening, whereas a CT angiography depicted a normal course and diameter of the vertebral artery. A MRI showed evidence of high T2 signal intensity and wasting of the cord and severe spinal cord compression at the atlantoaxial level (
FIGURE 2A). Under general anesthesia, the surgical treatment consisted of the posterior decompression and posterior fixation, bone fusion under the surgical navigation system guidance (StealthStation
® TREON Plus; Medtronic Navigation Inc., Louisville, CO, USA) and intraoperative monitoring (NIMS
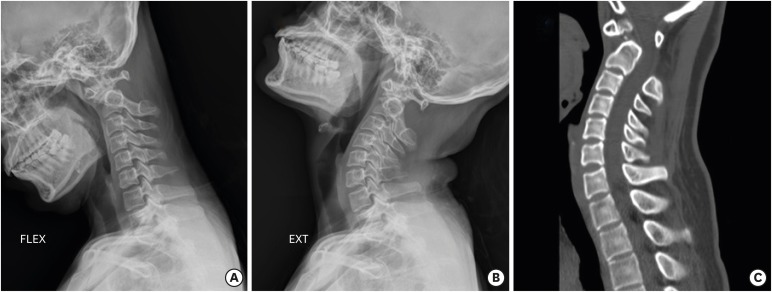
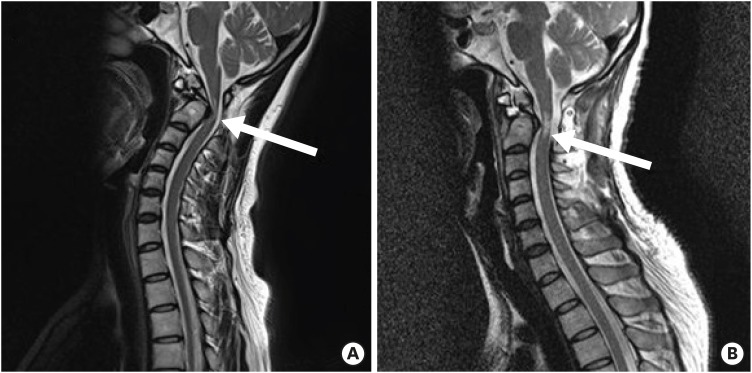
®; Medtronic, Minneapolis, MN, USA). Our procedure was done carefully with microscope and high-speed drill. There were no complications of vital sign and skills and no abnormal electrophysiologic response during the surgery. Postoperative dynamic X-rays and CT scan revealed complete reduction at the C1/2 level and decompressed high cervical level (
FIGURE 3). However, on postoperative neurologic evaluation a flaccid quadriplegia with abbreviation injury scale (AIS) scale B; and anesthesia on all extremity were both noticed. A postoperative emergency MRI revealed sufficient decompression of the spinal canal at C1/2 level, however, showed increased a high signal intensity change in the spinal cord spread from the level of C1/2 on T2-weighted image (
FIGURE 2B). We decided to do the high dose steroid tapering therapy and use naloxone, mannitol. After postoperative 1 week, the symptoms of the patient were improved and we started physical therapy by consultation of rehabilitation department. Fortunately, the patient made a good recovery with some neurological sequelae 1 month later. At 6 months follow-up the patient had nearly returned to her previous activities: AIS scale E. She could do general livings finally.
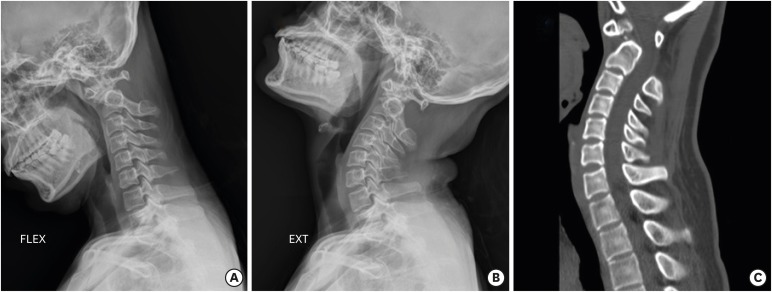 | FIGURE 1
Lateral radiographs of the cervical spine during flexion (A), extension (B) showing atlantoaxial instability, and (C) Cervical computed tomography showing a dystopic-type os odontoideum and significant C1/2 subluxation, severe widening C1/2 interlaminar space.
FLEX: flexion, EXT: extension.

|
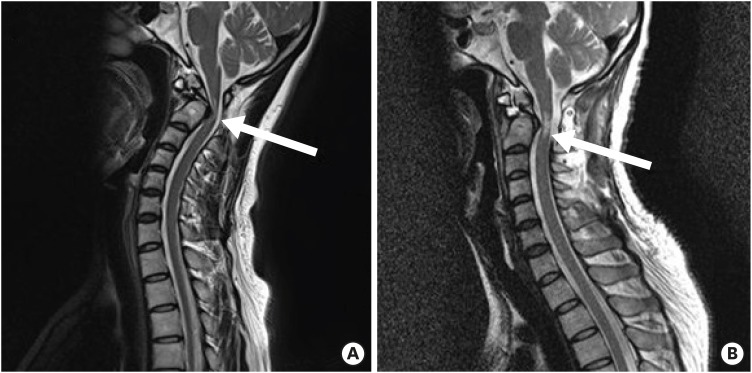 | FIGURE 2
(A) Preoperative sagittal T2-wighted MRI revealing a kinking of spinal cord and myelomalacia at the C1/2 level (left arrow). (B) Postoperative sagittal T2-wighted MRI showing increased a high signal intensity change in the spinal cord spread from the level of C1/2 (right arrow).
MRI: magnetic resonance imaging.

|
 | FIGURE 3
Postoperative lateral radiographs of the cervical flexion (A) and extension (B) showing an instrumented construct with anatomical reduction of C1/2. (C) Postoperative computed tomography showing well screw placement.
FLEX: flexion, EXT: extension.

|
This research was approved by Institutional Review Board of Inje University Busan Paik Hospital (IRB 2019-04-007) and the board waived the requirement to obtain informed consent.
Go to :

DISCUSSION
The atlantoaxial instability is associated with a translation of the C1 body and the os odontoideum relative to C2. Anterolisthesis describes the anterior subluxation of the C1-os odontoideum complex in relation to C2 during flexion. Translational instability and dislocation result in a posterior spinal cord injury. In posterior subluxation the os odontoideum and C1 are translating posteriorly into the spinal canal during extension. Anterolisthesis seems to be more often; however, some patients have instability in both directions.
2)
Because the biomechanically, a compromise of the integrity of the odontoid-transverse ligament complex must weaken atlantoaxial stability, this instability can result in severe spinal cord injury in even minor events, Successful treatment of os odontoideum aims to stabilize the C1/C2 joint with or without decompression.
In a like our case, although rare, it is critical problem unexpectedly developing neurologic compromise after treatment. It appears to be caused by reperfusion after decompression of a chronic compressive lesion of the cervical cord. In our worst case, the injury can lead to quadriplegia microcirculatory disturbance due to reperfusion can occur in any level and any region where surgical decompression was performed for the chronic compressive lesion. The severity and territory of the symptom depend on the area where neurons are really damaged. These results support hypothesis that the etiology of the paralysis is a transient disturbance of the spinal cord following a decompression procedure.
4) Results from postoperative MRI in patients with distal and diffuse paresis of all extremity are also congruous with the reperfusion injury hypothesis.
8)
Reoxygenation-reperfusion injury to the ischemic brain and thoracic spinal cord are well-known in clinics. Incomplete ischemia and subsequent reperfusion in an animal model demonstrated that following typical ischemic injury to the spinal cord, release of free fatty acids, increase of Ca
2 intake, and vascular permeability impair tissue metabolism.
3) These can limit the possibility of enhanced recovery and deteriorate neurologic function in the reperfusion period. Therefore, the mechanism on brain and thoracic spinal cord injury might also underlie cervical spinal cord injury.
Also, many authors have reported that free radicals played an important role in palsy resolution in the reperfused spinal cord.
6)
Our case presented here is the important report that detected the pre- and post-operative condition of the spinal cord using MRI. The pre-operative MRI showed a relatively narrow spinal canal and severe compression of spinal cord by subluxation due to os odontoideum. The patient exhibited mild myelopathic symptoms before the acute onset of quadriplegia. On admission, the spinal cord may have been at a critical time leading to infarction of the spinal cord or spinal shock. However, we could not predict that this case would progress to complete paraplegia after surgery.This case suggests the importance of considering that patients with chronic subluxation with developmental canal stenosis seen on MRI, especially those with severe compression at the high cervical level due to os odontoideum, may represent a critical condition that can progress to acute paraplegia after surgery. Furthermore, the possibility of rapid progression of myelopathy secondary to cervical motion associated with physical examination or changing position during surgery should be remembered.
Our surgical procedure was planned to complete the translational reduction and to perform posterior instrumentation. The use of somatosensory evoked potential and motor evoked potential may help to detect any sensory deficit,weakness early and is therefore recommended. However, we must keep in mind this method could not guarantee status of patient. Furthermore, the possibility of rapid progression of myelopathy secondary to cervical motion associated with physical examination or changing position during surgery should be remembered. Once acute neurologic deterioration developed, it seems better to perform urgently all examination and treatment preparing for spinal cord.
Go to :

CONCLUSION
If chronic myelopathy was found in os odontoideum patients, carefully decompressive surgery and subsequent fixation is required. Also, because progressive myelopathy can present with variable symptoms, it is important that surgeons recognize and aggressively evaluate postoperative neurologic sign to prevent a potentially life-threatening complication. We recommend that surgeons inform patients of the potential risk of a spinal cord deficit after complex cervical decompression surgery.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download