1. Orsi IA, Soares RG, Villabona CA, Panzeri H. Evaluation of the flexural strength and elastic modulus of resins used for temporary restorations reinforced with particulate glass fibre. Gerodontology. 2012; 29:e63–e68. PMID:
20735489.

2. Regish KM, Sharma D, Prithviraj DR. Techniques of fabrication of provisional restoration: an overview. Int J Dent. 2011; 2011:134659. PMID:
22013441.

3. Alharbi N, Osman R, Wismeijer D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J Prosthet Dent. 2016; 115:760–767. PMID:
26803175.

4. Davidowitz G, Kotick PG. The use of CAD/CAM in dentistry. Dent Clin North Am. 2011; 55:559–570. PMID:
21726690.

5. Lee WS, Lee DH, Lee KB. Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system. J Adv Prosthodont. 2017; 9:265–270. PMID:
28874993.

6. Stansbury JW, Idacavage MJ. 3D printing with polymers: Challenges among expanding options and opportunities. Dent Mater. 2016; 32:54–64. PMID:
26494268.

7. Shamseddine L, Mortada R, Rifai K, Chidiac JJ. Marginal and internal fit of pressed ceramic crowns made from conventional and computer-aided design and computer-aided manufacturing wax patterns: An in vitro comparison. J Prosthet Dent. 2016; 116:242–248. PMID:
26948080.
8. Park JM, Hong YS, Park EJ, Heo SJ, Oh N. Clinical evaluations of cast gold alloy, machinable zirconia, and semiprecious alloy crowns: A multicenter study. J Prosthet Dent. 2016; 115:684–691. PMID:
26794694.

9. Koch GK, Gallucci GO, Lee SJ. Accuracy in the digital workflow: From data acquisition to the digitally milled cast. J Prosthet Dent. 2016; 115:749–754. PMID:
26803173.

10. Berman B. 3-D printing: The new industrial revolution. Business Horizons. 2012; 55:155–162.

11. Burns DR, Beck DA, Nelson SK. Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J Prosthet Dent. 2003; 90:474–497. PMID:
14586312.

12. Mai HN, Lee KB, Lee DH. Fit of interim crowns fabricated using photopolymer-jetting 3D printing. J Prosthet Dent. 2017; 118:208–215. PMID:
28089333.
13. Koumjian JH, Nimmo A. Evaluation of fracture resistance of resins used for provisional restorations. J Prosthet Dent. 1990; 64:654–657. PMID:
2079670.

14. Gegauff AG, Wilkerson JJ. Fracture toughness testing of visible light- and chemical-initiated provisional restoration resins. Int J Prosthodont. 1995; 8:62–68. PMID:
7710627.
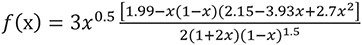
15. Moon JE, Kim SH, Lee JB, Han JS, Yeo IS, Ha SR. Effects of airborne-particle abrasion protocol choice on the surface characteristics of monolithic zirconia materials and the shear bond strength of resin cement. Ceram Int. 2016; 42:1552–1562.

16. Ha SR, Kim SH, Lee JB, Han JS, Yeo IS. Improving shear bond strength of temporary crown and fixed dental prosthesis resins by surface treatments. J Mater Sci. 2016; 51:1463–1475.

17. Chen HL, Lai YL, Chou IC, Hu CJ, Lee SY. Shear bond strength of provisional restoration materials repaired with light-cured resins. Oper Dent. 2008; 33:508–515. PMID:
18833857.

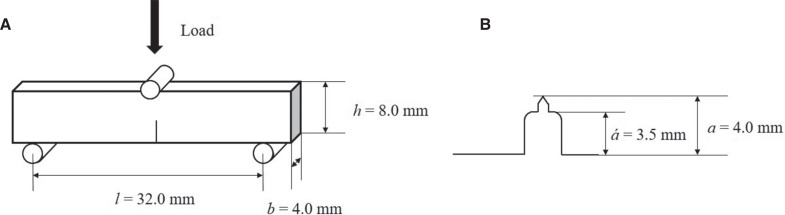
18. Im YW, Jun SK, Kim SC, Kim DA, Kim GR, Kim NS, Lee HH. Standardized test methods for mechanical properties of dental prosthetic/restorative materials and their applications. Korean J Dent Mater. 2015; 42:259–270.

19. Brosh T, Pilo R, Bichacho N, Blutstein R. Effect of combinations of surface treatments and bonding agents on the bond strength of repaired composites. J Prosthet Dent. 1997; 77:122–126. PMID:
9051597.

20. Ozcan M. Evaluation of alternative intra-oral repair techniques for fractured ceramic-fused-to-metal restorations. J Oral Rehabil. 2003; 30:194–203. PMID:
12535148.
21. Shahverdi S, Canay S, Sahin E, Bilge A. Effects of different surface treatment methods on the bond strength of composite resin to porcelain. J Oral Rehabil. 1998; 25:699–705. PMID:
9758401.

22. Suliman AH, Swift EJ Jr, Perdigao J. Effects of surface treatment and bonding agents on bond strength of composite resin to porcelain. J Prosthet Dent. 1993; 70:118–120. PMID:
8396642.

23. Cavalcanti AN, De Lima AF, Peris AR, Mitsui FH, Marchi GM. Effect of surface treatments and bonding agents on the bond strength of repaired composites. J Esthet Restor Dent. 2007; 19:90–98. PMID:
17374114.

24. Ataol AS, Ergun G. Repair bond strength of resin composite to bilayer dental ceramics. J Adv Prosthodont. 2018; 10:101–112. PMID:
29713430.

25. Lee YG, Moon SR, Cho YG. Effect of cutting instruments on the dentin bond strength of a self-etch adhesive. J Korean Acad Cons Dent. 2010; 35:13–19.

26. Gregory WA, Pounder B, Bakus E. Bond strengths of chemically dissimilar repaired composite resins. J Prosthet Dent. 1990; 64:664–668. PMID:
2150415.

27. da Costa TR, Serrano AM, Atman AP, Loguercio AD, Reis A. Durability of composite repair using different surface treatments. J Dent. 2012; 40:513–521. PMID:
22410401.

28. Özcan M, Corazza PH, Marocho SM, Barbosa SH, Bottino MA. Repair bond strength of microhybrid, nanohybrid and nanofilled resin composites: effect of substrate resin type, surface conditioning and ageing. Clin Oral Investig. 2013; 17:1751–1758.

29. Bacchi A, Consani RL, Sinhoreti MA, Feitosa VP, Cavalcante LM, Pfeifer CS, Schneider LF. Repair bond strength in aged methacrylate- and silorane-based composites. J Adhes Dent. 2013; 15:447–452. PMID:
23593643.
30. Kimyai S, Oskoee SS, Mohammadi N, Rikhtegaran S, Bahari M, Oskoee PA, Vahedpour H. Effect of different mechanical and chemical surface treatments on the repaired bond strength of an indirect composite resin. Lasers Med Sci. 2015; 30:653–659. PMID:
23873595.

31. Ozcan M, Alander P, Vallittu PK, Huysmans MC, Kalk W. Effect of three surface conditioning methods to improve bond strength of particulate filler resin composites. J Mater Sci Mater Med. 2005; 16:21–27. PMID:
15754140.
32. Swift EJ Jr, LeValley BD, Boyer DB. Evaluation of new methods for composite repair. Dent Mater. 1992; 8:362–365. PMID:
1303383.

33. Lucena-Martín C, González-López S, Navajas-Rodríguez de Mondelo JM. The effect of various surface treatments and bonding agents on the repaired strength of heat-treated composites. J Prosthet Dent. 2001; 86:481–488. PMID:
11725276.

34. Oztas N, Alaçam A, Bardakçy Y. The effect of air abrasion with two new bonding agents on composite repair. Oper Dent. 2003; 28:149–154. PMID:
12670070.
35. Azarbal P, Boyer DB, Chan KC. The effect of bonding agents on the interfacial bond strength of repaired composites. Dent Mater. 1986; 2:153–155. PMID:
2943623.

36. Saunders WP1. Effect of fatigue upon the interfacial bond strength of repaired composite resins. J Dent. 1990; 18:158–162. PMID:
2205638.

37. Crumpler DC, Bayne SC, Sockwell S, Brunson D, Roberson TM. Bonding to resurfaced posterior composites. Dent Mater. 1989; 5:417–424. PMID:
2700978.

38. Eli I, Liberman R, Levi N, Haspel Y. Bond strength of joined posterior light-cured composites: comparison of surface treatments. J Prosthet Dent. 1988; 60:185–189. PMID:
3050036.

39. Hisamatsu N, Atsuta M, Matsumura H. Effect of silane primers and unfilled resin bonding agents on repair bond strength of a prosthodontic microfilled composite. J Oral Rehabil. 2002; 29:644–648. PMID:
12153453.

40. Ozcan M, Barbosa SH, Melo RM, Galhano GA, Bottino MA. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent Mater. 2007; 23:1276–1282. PMID:
17174388.

41. Lee HY, Han GJ, Chang J, Son HH. Bonding of the silane containing multi-mode universal adhesive for lithium disilicate ceramics. Restor Dent Endod. 2017; 42:95–104. PMID:
28503474.

42. El Zohairy AA, De Gee AJ, Hassan FM, Feilzer AJ. The effect of adhesives with various degrees of hydrophilicity on resin ceramic bond durability. Dent Mater. 2004; 20:778–787. PMID:
15302458.
43. Takahashi M1, Nakajima M, Hosaka K, Ikeda M, Foxton RM, Tagami J. Long-term evaluation of water sorption and ultimate tensile strength of HEMA-containing/-free one-step self-etch adhesives. J Dent. 2011; 39:506–512. PMID:
21575671.

44. Fahmy NZ, Sharawi A. Effect of two methods of reinforcement on the fracture strength of interim fixed partial dentures. J Prosthodont. 2009; 18:512–520. PMID:
19432757.

45. Balkenhol M, Köhler H, Orbach K, Wöstmann B. Fracture toughness of cross-linked and non-cross-linked temporary crown and fixed partial denture materials. Dent Mater. 2009; 25:917–928. PMID:
19249090.

46. Tahayeri A, Morgan M, Fugolin AP, Bompolaki D, Athirasala A, Pfeifer CS, Ferracane JL, Bertassoni LE. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater. 2018; 34:192–200. PMID:
29110921.







 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download