Abstract
Objectives
The aim of this study was to explore the prevalence of type 1 diabetes in patients with schizophrenia and their total medical costs and risk of hospitalization.
Methods
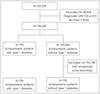
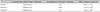
This study used Health Insurance Review and Assessment Service data in Korea. To examine total medical costs and risk of hospitalization, we selected 1,510 subjects with schizophrenia (half with and half without type 1 diabetes) that were 1:1 matched via propensity score matching. In health care system perspective, total medical costs included out-of-pocket and insurer's costs. Logistic regression models were used to examine the risk of hospitalization.
Results
The prevalence of type 1 diabetes in patients with schizophrenia was 3.87 per 1,000 person year. Among patients with schizophrenia, the amount of total average medical costs and hospitalization costs in patients with type 1 diabetes was 1.49 and 1.59 times higher than those in patients without it, respectively. The odds of hospitalization were higher among patients with type 1 diabetes compared with those without it (odds ratio, OR=1.97 ; 95% CI 1.60–2.43).
Figures and Tables
References
1. World Health Organization. Prevention of Mental Disorders: Effective Interventions and Policy Options. Geneva: World Health Organization;2004. p. 15–16.
2. Bloom D, Cafiero E, Jané-Llopis E, Abrahams-Gessel S, Bloom L, Fathima S, et al. The global economic burden of noncommunicable diseases. Geneva: World Economic Forum;2012.
3. Korea Health Industry Development Industry. Mental illness sector R & D trends and implications (HT R&D No 2013-006). Osong: 2013.
4. Chang SM, Cho SJ, Jeon HJ, Hahm BJ, Lee HJ, Park JI, et al. Economic burden of schizophrenia in South Korea. J Korean Med Sci. 2008; 23:167–175.



5. Ministry of Health & Welfare. The epidemiological survey of mental disorders in Korea. Sejong: 2016.
6. Simeone JC, Ward AJ, Rotella P, Collins J, Windisch R. An evaluation of variation in published estimates of schizophrenia prevalence from 1990-2013: a systematic literature review. BMC Psychiatry. 2015; 15:193.



7. Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014; 10:425–448.


8. Mitchell AJ, Vancampfort D, Sweers K, Van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders-a systematic review and meta-analysis. Schizophr Bull. 2011; 39:306–318.



9. Ratliff JC, Palmese LB, Reutenauer EL, Srihari VH, Tek C. Obese schizophrenia spectrum patients have significantly higher 10-year general cardiovascular risk and vascular ages than obese individuals without severe mental illness. Psychosomatics. 2013; 54:67–73.


10. Hert M, Schreurs V, Vancampfort D, Winkel R. Metabolic syndrome in people with schizophrenia: a review. World Psychiatry. 2009; 8:15–22.



11. Stubbs B, Vancampfort D, De Hert M, Mitchell AJ. The prevalence and predictors of type two diabetes mellitus in people with schizophrenia: a systematic review and comparative meta-analysis. Acta Psychiatr Scand. 2015; 132:144–157.


12. Vancampfort D, Sweers K, Probst M, Maurissen K, Knapen J, Minguet P, et al. Association of the metabolic syndrome with physical activity performance in patients with schizophrenia. Diabetes Metab. 2011; 37:318–323.


13. Nasrallah HA, Meyer JM, Goff DC, McEvoy JP, Davis SM, Stroup TS, Lieberman JA. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophr Res. 2006; 86:15–22.


14. Becker T, Hux J. Risk of acute complications of diabetes among people with schizophrenia in Ontario. Canada. Diabetes Care. 2011; 34:398–402.



15. Eaton WW, Byrne M, Ewald H, Mors O, Chen CY, Agerbo E, et al. Association of schizophrenia and autoimmune diseases: linkage of Danish national registers. Am J Psychiatry. 2006; 163:521–528.


16. Juvonen H, Reunanen A, Haukka J, Muhonen M, Suvisaari J, Arajärvi R, et al. Incidence of schizophrenia in a nationwide cohort of patients with type 1 diabetes mellitus. Arch Gen Psychiatry. 2007; 64:894–899.


17. Benros ME, Nielsen PR, Nordentoft M, Eaton WW, Dalton SO, Mortensen PB. Autoimmune diseases and severe infections as risk factors for schizophrenia: a 30-year population-based register study. Am J Psychiatry. 2011; 168:1303–1310.


18. Chen SJ, Chao YL, Chen CY, Chang CM, Wu EC, Wu CS, et al. prevalence of autoimmune diseases in in-patients with schizophrenia: nationwide population-based study. Br J Psychiatry. 2012; 200:374–380.


19. Goueslard K, Petit JM, Cottenet J, Chauvet-Gelinier JC, Jollant F, Quantin C. Increased Risk of Rehospitalization for Acute Diabetes Complications and Suicide Attempts in Patients With Type 1 Diabetes and Comorbid Schizophrenia. Diabetes Care. 2018; 41:2316–2321.


20. Kim LY, Jin SK, Kim Y, Kim SR, Kim SY, Tchoe BH, et al. Developing the inpatient sample for the National Health Insurance claims data. Health Policy Manag. 2013; 23:152–161.

21. Jun JA, Son SJ, Lee NH, Choi JH. Prevalence of Multimorbidity and Transitional Patterns of Chronic Diseases among Korean Adults. Seoul: Korea Institute for Health and Social Affairs;2014.
22. Kim CH, Lee MR, Yoo WS. Common combinations of chronic diseases in multimorbidity and their effect on healthcare cost in Korea. Korean J Health Econ Policy. 2014; 20:81–102.
23. Guo S, Fraser MC. Propensity Score Analysis: Statistical Methods and Applications CA. SAGE Publications Inc;2010.
24. Parsons LS. Performing a 1:N case-control match on propensity score. In : Proceedings of the 29th Annual SAS Users Group International Conference; Montreal, Canada: SAS Institute;2004.
25. Hallford P, St Clair D, Halley L, Mustard C, Wei J. A study of type-1 diabetes associated autoantibodies in schizophrenia. Schizophr Res. 2016; 176:186–190.

26. Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006; 29:725–731.


27. Harman JS, Edlund MJ, Fortney JC, Kallas H. The influence of comorbid chronic medical conditions on the adequacy of depression care for older Americans. J Am Geriatr Soc. 2005; 53:2178–2183.


28. Yoon J, Zulman D, Scott JY, Maciejewski ML. Costs associated with multimorbidity among VA patients. Med Care. 2014; 52:Suppl 3. S31–S36.

29. Mental Health Taskforce. The five year forward view for mental health. [Internet]. Mental Health Taskforce;2016. cited 2018 Nov 30. Available from: https://www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final.pdf.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download