INTRODUCTION
Anaphylaxis is a life-threatening condition caused by allergic reactions to various allergens including food and drug. In the past 10 years, there has been a significant increase in the incidence of anaphylaxis around the world. In Thailand, our previous study found that the incidence of anaphylaxis had increased from 9.16 per 100,000 admissions in 1999 to 55.45 per 100,000 admissions in 2004 [
1]. Common causes of anaphylaxis in the pediatric age group were drug (29.6%) and food (29.6%) allergies [
1]. This result corresponded to the findings of Manuyakorn et al. [
2]. For food-induced anaphylaxis, seafood was the most common allergen followed by wheat [
12]. The in-hospital mortality rate in Thailand is 0.19 deaths per 100,000 admissions [
1].
Standard treatment for anaphylaxis includes prompt administration of epinephrine when patients have anaphylactic reactions. However, the rate of carrying and using epinephrine in patients with a history of anaphylaxis is quite low in many studies. Pouessel et al. [
3] investigated the parental knowledge and readiness to use epinephrine auto-injector (EAI). They found that the rate of carrying epinephrine devices to be 60%–72% and only 60% had emergency kits at school. Carrillo et al. [
4], demonstrated that only 54% of patients with anaphylaxis symptoms used epinephrine devices before going to the hospital. A study conducted in Thailand reported that epinephrine was prescribed to only 40% of adult anaphylaxis patients and none used the epinephrine device during an anaphylactic event [
2]. However, there was limited data on the rate of carrying and injecting epinephrine in food-induced anaphylaxis in Thai children.
A 2013 study by Marrs and Lack [
5] reported the most common causes of underusing and carrying of epinephrine were lack of knowledge to use the medication, fear of using EAI, believing it was not necessary to carry epinephrine, lack of school readiness and bullying by other students. In Thailand, most patients who have a history of anaphylaxis are prescribed epinephrine in a prefilled syringe. A recent study found that it is easier to use and less costly than EAI [
6]. Therefore, the prefilled syringe may increase the likelihood that children will carry and use epinephrine.
The purpose of this study is to determine the rate of carrying epinephrine devices (both auto-injector and prefilled syringe) and factors influencing the decision to use and carry epinephrine devices in pediatric patients with a history of food-induced anaphylaxis to inform clinical management and improve quality of care in food-induced anaphylaxis patients.
RESULTS
Patient characteristics
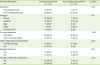
Ninety-nine subjects who met the inclusion criteria were enrolled. Twenty-one subjects (21.2%) were interviewed in person during a follow-up session and 78 were interviewed by telephone. Demographic data and patient illness information are summarized in
Tables 1 and
2. The current median age was 11 years old (range, 9 months to 18 years old). Fifty-eight of them (58.6%) were diagnosed with anaphylaxis before 1 year of age. Most of them were taken care by their mother (72.7%), and 48.5% of the primary caregivers completed bachelor degree. Epinephrine devices were given to all subjects. Eighty-nine of subjects were prescribed a prefilled syringe that was changed every 3 months.
Table 1
Demographic data of study population (N = 99)

|
Characteristic |
Carrying epinephrine (n = 84) |
Not carrying epinephrine (n = 15) |
p value |
|
Male sex |
44 (52.4) |
6 (40.0) |
0.37 |
|
Current age (median, 11 yr) |
|
|
0.64 |
|
0–5 yr |
16 (19.0) |
1 (6.7) |
|
6–12 yr |
41 (48.8) |
9 (60.0) |
|
13–18 yr |
27 (32.1) |
5 (33.3) |
|
Age at diagnosis (median, 3 yr) |
|
|
0.85 |
|
0–5 yr |
48 (57.1) |
10 (66.7) |
|
6–12 yr |
24 (28.6) |
4 (26.7) |
|
13–18 yr |
12 (14.3) |
1 (6.7) |
|
Family income |
|
|
0.49 |
|
<50,000 Baht |
48 (57.1) |
10 (66.7) |
|
≥50,000 Baht |
36 (42.9) |
5 (33.3) |

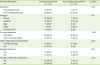
Table 2
Clinical course of food anaphylaxis (N = 99)
|
Illness information |
Carrying epinephrine (n = 84) |
Not carrying epinephrine (n = 15) |
p value |
|
Symptom |
|
|
0.45 |
|
Including syncope |
15 (17.9) |
1 (6.7) |
|
Not including syncope |
69 (82.1) |
14 (93.3) |
|
Allergen |
|
|
0.31 |
|
Wheat |
33 (39.3) |
7 (46.7) |
|
Seafood |
27 (32.1) |
6 (40.0) |
|
Egg |
5 (6.0) |
0 (0) |
|
Other |
5 (6.0) |
2 (13.3) |
|
Multiple food |
14 (16.7) |
0 (0) |
|
Current treatment |
|
|
1.00 |
|
Avoidance |
69 (82.1) |
13 (86.7) |
|
Oral immunotherapy |
15 (17.9) |
2 (13.3) |
|
Type of epinephrine prescribed |
|
|
0.35 |
|
Prefilled syringe |
74 (88.1) |
15 (100) |
|
EAI |
10 (11.9) |
0 (0) |
|
Regular follow-up |
|
|
0.21 |
|
Yes |
74 (88.1) |
11 (73.3) |
|
No |
10 (11.9) |
4 (26.7) |
|
Having a repeated anaphylaxis |
|
|
0.65 |
|
Yes |
34 (40.5) |
7 (46.7) |
|
No |
50 (59.5) |
8 (53.3) |

The most common cause of food-induced anaphylaxis was wheat (n = 52) followed by seafood (n = 37), egg (n = 15), peanut (n = 2), and insect (n = 3). Five subjects had been diagnosed with wheat-dependent, exercise-induced anaphylaxis. In the seafood anaphylaxis group, most subjects (17 subjects) were allergic to multiple seafood allergens, while 10 subjects were allergic only to shrimp.
All subjects had skin or mucosal symptoms accompanied by other systems involvement (86.9% had 2 systems and 13.1% had 3 systems). Cardiovascular symptoms were reported in 16% of subjects.
Rate of carrying epinephrine devices
Rate of carrying epinephrine devices was shown in
Fig. 1. The percentage of patients who always carry epinephrine was 57.5%, while 24.2% reported they carry it only to restaurants or traveling. Three percent said they only carried epinephrine to school and 16.1% indicated that they never carry epinephrine. There was no statistically significant difference between those with “wheat and non-wheat allergy” (
p = 0.62), “egg and non-egg allergy” (
p = 0.11) or “single allergen and multiple allergens” (
p = 0.12).
 | Fig. 1Rate of carrying epinephrine devices (N = 99).
|
Factors associated with carrying epinephrine devices
Among 42 subjects who did not always carry epinephrine, the most common reason that they decided not to carry the devices was parents' belief that they can avoid allergens (24 subjects). Interestingly, subjects who did not carry epinephrine devices due to this reason had a significantly lower rate of relapse compared to other explanations (p = 0.02).
Twenty-three percent of subjects reported that carrying epinephrine was not convenient. Among these, 52.2% experienced drug instability including color changing and drug evaporation before the expiration date, 26.1% experienced difficulty while recapping the needle, 8.7% experienced package collapsing, and 8.7% were afraid to carry epinephrine devices with them.
Parental knowledge was also assessed. Almost all subjects (99%) knew when to use epinephrine and all of them could recall the steps to use it correctly. However, most of the subjects still afraid to use epinephrine when it is needed. Most subjects suggested that a simulation practice session could help to boost parental confidence to use epinephrine.
There were 89 subjects who are in school-age. The school facilities for children with food allergy are shown in
Table 3. Almost all subjects (91%) informed school officer and teachers about their illness, while others decided not to report because parents thought their children were mature enough to take care of themselves. Half of subjects (50.6%) had an observer at school to help them avoid foods that could cause anaphylaxis. However, 51.7% of subjects had no emergency room or school nurse at their school. Only 3% experienced bullying at school and all of the bullying were from teachers. However, the availability of school emergency room or nurse did not affect their decision to carry epinephrine.
Table 3
School types and facilities (N = 89)

|
School type and facility |
Carrying to school (n = 55) |
Not carrying to school (n = 34) |
p value |
|
Subject educational status |
|
|
0.81 |
|
Kindergarten/elementary school |
32 (58.2) |
18 (52.9) |
|
High school |
21 (38.2) |
14 (41.2) |
|
Bachelor degree |
2 (3.6) |
2 (5.9) |
|
Type of school |
|
|
0.24 |
|
State school |
27 (49.1) |
21 (61.8) |
|
Private school/international school |
28 (50.9) |
13 (38.2) |
|
Having illness information at school |
|
|
1.00 |
|
Yes |
50 (90.9) |
31 (91.2) |
|
No |
5 (9.1) |
3 (8.8) |
|
Having special caution at school |
|
|
0.72 |
|
Yes |
27 (49.1) |
18 (52.9) |
|
No |
28 (50.9) |
16 (47.1) |
|
Having first aid room at school |
|
|
0.05 |
|
Yes |
31 (56.4) |
12 (35.3) |
|
No |
24 (43.6) |
22 (64.7) |
|
Experienced school bullying |
|
|
0.55 |
|
Yes |
1 (1.8) |
2 (5.9) |
|
No |
54 (98.2) |
32 (94.1) |

We found no relationship between the rate of carrying epinephrine devices and the sex or age of subjects, income and educational status of parents, type of current treatment, presenting symptoms, and type of allergens. The reported fear and inconvenience of carrying epinephrine devices also did not significantly influence the decision to carry them. Subjects who missed their follow-up session did not have lower rate of carrying epinephrine because they received epinephrine from a nearby hospital. Subjects who had repeated episode did not have significantly lower rate of carrying epinephrine (p = 0.65).
Rate of repeated anaphylaxis
The rate of repeated anaphylaxis during the previous 5 years and the cause of repeated was reviewed (
Table 4). No repeated episode was observed in 58.5% of subjects and 37.4% repeated 1–3 times. The most common cause of repeated anaphylaxis was accidental exposure to an offending allergen (78%), followed by intentionally eating the food because they expected only mild symptoms (17.1%). There was no relation between the age of subjects and the rate of repeated anaphylaxis.
Table 4
Rate of relapsing, cause of relapsing, and treatment of repeated anaphylaxis (N = 41)

|
Variable |
Carrying epinephrine (n = 34) |
Not carrying epinephrine (n = 7) |
p value |
|
Rate of relapsing during past 5 years |
|
|
0.16 |
|
1–3 |
32 (94.1) |
5 (71.4) |
|
>3 |
2 (5.8) |
2 (28.5) |
|
Cause of relapsing (n = 41) |
|
|
1.00 |
|
Contamination |
26 (76.5) |
6 (85.7) |
|
Others |
8 (23.5) |
1 (14.3) |
|
|
Intentionally eat in large amount |
6 |
1 |
|
|
Intentionally eat in small amount |
1 |
0 |
|
|
Forced to eat by others |
1 |
0 |
|
Treatment of relapsing episode (n = 41) |
|
|
0.01 |
|
Using epinephrine |
20 (58.8) |
0 (0) |
|
|
Epinephrine alone |
10 |
0 |
|
|
Epinephrine + hospital visit |
9 |
0 |
|
|
Epinephrine + other medicine |
1 |
0 |
|
Not using epinephrine |
14 (41.2) |
7 (100) |
|
|
Hospital visit |
6 |
3 |
|
|
Using other medicine |
2 |
2 |
|
|
Using other med + hospital visit |
6 |
2 |
|
Reason for not using epinephrine (n = 14) |
|
|
0.44 |
|
Afraid to use epinephrine |
4/14 (28.6) |
2/7 (28.6) |
|
Live near hospital |
6/14 (42.8) |
1/7 (14.3) |
|
Other |
4/14 (28.6) |
4/7 (57.1) |

Self-injected epinephrine was used in 20 out of 41 subjects (48.8%) who had repeated anaphylaxis. The rest of them decided to use other medications or go to a hospital. The epinephrine formulation did not affect the decision to use. All subjects who used epinephrine reported a rapid improvement of symptoms. Among the 21 subjects who did not use self-injected epinephrine, the most common reasons were did not carry epinephrine (33.3%), followed by lived near a hospital and decided to go there instead (33.3%), and afraid to inject by themselves (28.5%). Sixty-five percent of patients admitted that they fear using epinephrine. Fear of using epinephrine was the only variable that influenced the frequency of using the medication (p = 0.001).
Since parental concern about allergen contamination in food could affect the rate of relapse, we asked how often they read food labels and how strict were they about avoiding allergens. We found that 82 parents (82.8%) read food labels regularly while 9 parents (9.1%) read sometimes, and 8 parents (8.1%) did not read at all. Among those parents who did not read food labels regularly, 9 out of 17 (52.9%) believed they could avoid allergens while 5 out of 17 (29.4%) thought their child's symptoms had already subsided, 2 subjects (11.8%) were exercise-induced anaphylaxis. Thirteen subjects (13.1%) decided not to avoid allergens after reading the food label. The most common reason to not avoid allergens was that they no longer had severe symptoms and their condition was food-dependent, exercise-induced anaphylaxis.
DISCUSSION
Our study found that 57% of children with a history of food-induced anaphylaxis carried an epinephrine device. This proportion rose to 84.7% when including subjects who carried epinephrine in some occasions.
Previous studies in Thailand showed the rate of epinephrine device prescription was only 44%–70% [
12], but the rate of carrying epinephrine devices was not well demonstrated. The lower rate of epinephrine device prescription might be because those studies not specific to anaphylaxis from food, which is more difficult to avoid compared to drugs or venom. The type of allergic food may influence the decision to carry epinephrine. Our study showed that the most allergenic food is wheat, which is contained in a wide variety of food. In contrast, the most common allergenic food in the previous study was seafood, which is easier to avoid [
2].
Few studies investigated the rate of carrying epinephrine devices specifically in children with a history of food-induced anaphylaxis. One recent study in Dutch adolescents with food allergy found that 52 (94.5%) were prescribed the epinephrine device [
8]. Among these patients, 35 (67.3%) reported that they always carried the EAI, while 17 (32.7%) carried the EAI only under specific circumstances. Another study from Italy found that among 65 children with a history of anaphylaxis (65% caused by food), only 10 patients had been prescribed the EAI [
9]. All patients in our study were prescribed epinephrine devices. This is because our study was performed in a tertiary care hospital where all children with a history of anaphylaxis are referred to the allergy clinic.
We found that patients typically carry the epinephrine device when traveling or eating at a restaurant, similar to the report by Pouessel et al [
3]. In that study, the rate of carrying epinephrine was 66% to the restaurant, 53% during leisure activities, and 53% during school trips. Interestingly, Pouessel et al [
3] reported that the rate of carrying epinephrine to school was 72%, compared to 60.5% in our study.
Factors that might influence the frequency of carrying epinephrine include female sex, frequent repeat, higher education, and higher income [
10]. However, these factors had no significant effect in our study. This could be explained by the different socioeconomic level. The higher educational status in the previous study means the master degree (which had only 14% in our study), whereas our study referred to the education higher than the bachelor degree (48.5% of all subjects).
The age of patients might also influence the decision to carry an epinephrine device. Our study found that almost all patients younger than 5 years old carried epinephrine. However, the overall rate in our study is similar to the study in adolescent [
8].
Although wheat is usually hidden in many kinds of food and difficult to avoid, we found that the rate of carrying epinephrine was not statistically different between patients who were allergic to wheat and those who were allergic to other foods. Therefore, the cause of the food allergy may not influence the decision to carry the devices.
In a study from Marrs and Lack [
5], the likelihood of carrying EAI was found to be inversely proportional to the time period since the allergy was diagnosed. The severity of symptoms also affected rate of carrying epinephrine in adolescents. In our study, both factors did not affect our primary outcome. Furthermore, the fear of being viewed as different from other adolescents [
11] did was not an important factor in our study. This might be as a result of different style of raising children between Thailand and Western country. In Thailand, most children were still under supervision of their parents until at least 18 years old, while, in western countries, they tend to be living more independently.
In our study, 23 subjects (23%) believed the device was not appropriate, but this reason also did not affect the decision to carry devices. The physical features of epinephrine devices have been reported to affect the rate of carrying epinephrine devices [
11]. Most patients in our study used the epinephrine devices in the form of a prefilled syringe instead of the EAI. So some patients might be afraid about the appearance of the needles or some of them worried about the leakage and how to store the medicine.
Parental knowledge about how to use the devices was also assessed. Studies by Blyth and Sundrum [
12] and Gold and Sainsbury [
13], reported that only 24% of subjects knew how to use epinephrine devices, while other studies reported that patients had never been taught how to use epinephrine [
141516]. Another study showed that the demonstration was repeated at each medical follow-up visit for only 19% of families and 10% had never seen a demonstration at all [
3]. This could explain why reason parents did not use epinephrine in other studies was lack of knowledge about “when” and “how” to use devices [
121718]. In our study, 98 parents (99%) could explain the indication to use epinephrine devices correctly and all of them could recall the steps of using epinephrine correctly.
Previous studies have reported the rate of using EAI during an anaphylactic episode to be only 8%–25% [
815]. The most common reasons were that other medication was used or the patient did not think the episode was severe enough to require epinephrine. In contrast, 58.8% of our patients who were carrying epinephrine devices used them during anaphylactic episodes. The reason for not using epinephrine was their lack of confidence and afraid of using devices. Therefore, the knowledge about the indication and how to use the device is essential to improve the rate of self-epinephrine injection.
The most common cause of relapse was the accidental ingestion of allergenic foods. To prevent this, healthcare workers must emphasize allergen avoidance by urging parents and children to read nutritional labels and always to be aware of everything their child eats. School facilities are also crucial for anaphylaxis management, especially in young children. According to Ercan et al. [
18], among 237 teachers from both public and private schools, only 59 teachers (25%) knew all the symptoms requiring epinephrine injection. In a study by Gold and Sainsbury [
13], although 91 children (97%) inform the school of their allergy, only 27children (40%) had devices and nursing staff at school. In our study, only 60.5% of patients carried epinephrine to school, and only 48.3% of patients had access to a first aid room at school. Anaphylaxis education for teachers is needed in Thailand.
The limitation of our study is that we recruited only subjects who continued to follow-up at the allergy clinic or who could be contacted by phone. Therefore, the rate of carrying epinephrine devices in this group might be higher than reported in other studies.
There is a need for better education about the importance of habitually carrying epinephrine and to teach parents and their children to know when and how to use epinephrine devices. Larger studies including subjects who do not carry epinephrine should be done to identify factors that influence the decision not to carry and use epinephrine to prevent anaphylaxis.







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download