2. Harrison MS, Goldenberg RL. Global burden of prematurity. Semin Fetal Neonatal Med. 2016; 21(2):74–79.


3. Magro Malosso ER, Saccone G, Simonetti B, Squillante M, Berghella V. US trends in abortion and preterm birth. J Matern Fetal Neonatal Med. 2018; 31(18):2463–2467.


4. Lee NH. International trends and implications for preterm birth. Health Soc Welf Forum. 2013; (200):116–127.
5. Kim YJ, Lee BE, Park HS, Kang JG, Kim JO, Ha EH. Risk factors for preterm birth in Korea: a multicenter prospective study. Gynecol Obstet Invest. 2005; 60(4):206–212.

6. Di Renzo GC, Giardina I, Rosati A, Clerici G, Torricelli M, Petraglia F, et al. Maternal risk factors for preterm birth: a country-based population analysis. Eur J Obstet Gynecol Reprod Biol. 2011; 159(2):342–346.


7. Boghossian NS, Yeung E, Albert PS, Mendola P, Laughon SK, Hinkle SN, et al. Changes in diabetes status between pregnancies and impact on subsequent newborn outcomes. Am J Obstet Gynecol. 2014; 210(5):431.e1–431.e14.

8. Premkumar A, Henry DE, Moghadassi M, Nakagawa S, Norton ME. The interaction between maternal race/ethnicity and chronic hypertension on preterm birth. Am J Obstet Gynecol. 2016; 215(6):787.e1–787.e8.
9. Abiodun OI, Jantan A, Omolara AE, Dada KV, Mohamed NA, Arshad H. State-of-the-art in artificial neural network applications: a survey. Heliyon (Lond). 2018; 4(11):e00938.

10. Song X, Mitnitski A, Cox J, Rockwood K. Comparison of machine learning techniques with classical statistical models in predicting health outcomes. Stud Health Technol Inform. 2004; 107(Pt 1):736–740.

11. Goodwin LK, Maher S. Data mining for preterm birth prediction. In : Proceedings of the 2000 ACM Symposium on Applied Computing; March 19-21, 2000; Villa Olmo, Italy. New York, NY: Association for Computing Machinery;p. 46–51.
12. Goodwin LK, Iannacchione MA, Hammond WE, Crockett P, Maher S, Schlitz K. Data mining methods find demographic predictors of preterm birth. Nurs Res. 2001; 50(6):340–345.


13. Goodwin LK, Iannacchione MA. Data mining methods for improving birth outcomes prediction. Outcomes Manag. 2002; 6(2):80–85.

15. Han J, Micheline K. Data Mining: Concepts and Techniques. 2nd ed. San Francisco, CA: Elsevier;2006.
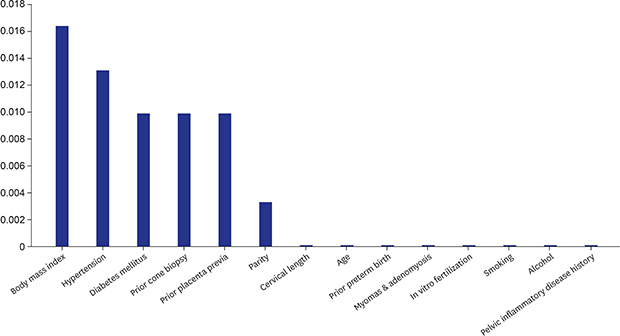
18. Shin D, Song WO. Prepregnancy body mass index is an independent risk factor for gestational hypertension, gestational diabetes, preterm labor, and small- and large-for-gestational-age infants. J Matern Fetal Neonatal Med. 2015; 28(14):1679–1686.


19. Sibai BM, Caritis SN, Hauth JC, MacPherson C, VanDorsten JP, Klebanoff M, et al. Preterm delivery in women with pregestational diabetes mellitus or chronic hypertension relative to women with uncomplicated pregnancies. The National institute of Child health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 2000; 183(6):1520–1524.

20. Hedderson MM, Ferrara A, Sacks DA. Gestational diabetes mellitus and lesser degrees of pregnancy hyperglycemia: association with increased risk of spontaneous preterm birth. Obstet Gynecol. 2003; 102(4):850–856.


21. Zhang J, Villar J, Sun W, Merialdi M, Abdel-Aleem H, Mathai M, et al. Blood pressure dynamics during pregnancy and spontaneous preterm birth. Am J Obstet Gynecol. 2007; 197(2):162.e1–162.e6.

22. O'Hara S, Zelesco M, Sun Z. Cervical length for predicting preterm birth and a comparison of ultrasonic measurement techniques. Australas J Ultrasound Med. 2013; 16(3):124–134.


23. McIntosh J, Feltovich H, Berghella V, Manuck T. Society for Maternal-Fetal Medicine (SMFM). The role of routine cervical length screening in selected high- and low-risk women for preterm birth prevention. Am J Obstet Gynecol. 2016; 215(3):B2–B7.

24. Berghella V, Pereira L, Gariepy A, Simonazzi G. Prior cone biopsy: prediction of preterm birth by cervical ultrasound. Am J Obstet Gynecol. 2004; 191(4):1393–1397.


25. Bevis KS, Biggio JR. Cervical conization and the risk of preterm delivery. Am J Obstet Gynecol. 2011; 205(1):19–27.


26. Pinborg A, Ortoft G, Loft A, Rasmussen SC, Ingerslev HJ. Cervical conization doubles the risk of preterm and very preterm birth in assisted reproductive technology twin pregnancies. Hum Reprod. 2015; 30(1):197–204.