1. Rowe PJ. WHO manual for the standardized investigation, diagnosis and management of the infertile male. 5th ed. Cambridge: Cambridge University Press;2000. p. 1–5.
2. Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, et al. European Association of Urology guidelines on male infertility: the 2012 update. Eur Urol. 2012; 62:324–332. PMID:
22591628.

3. Garg H, Kumar R. Empirical drug therapy for idiopathic male infertility: what is the new evidence? Urology. 2015; 86:1065–1075. PMID:
26255035.

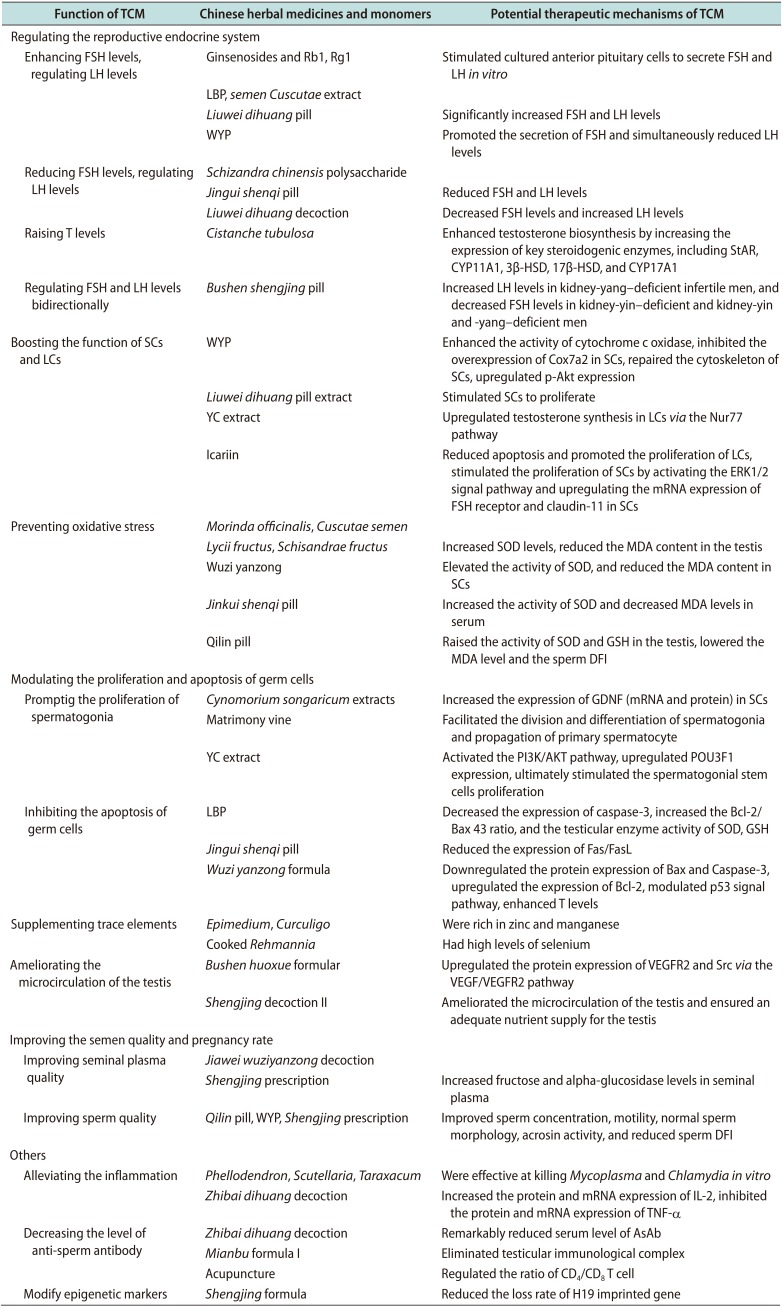
4. Cen YH, Zhao FL, Fan R, He GZ. Research progress in the reproductive-related kidney deficiency and kidney tonifying Chinese medicine mechanism. Med Recapitulate. 2014; 20:2226–2228.
5. Qian FL, Zeng FH, Feng WQ. Effects of Chinese herbal preparation for invigorating kidney on function of hypothalamicpituitary-gonad axis in rats. Chin J Sports Med. 2005; 24:571–575.
6. Luo Q, Li Z, Huang X, Yan J, Zhang S, Cai YZ. Lycium barbarum polysaccharides: protective effects against heat-induced damage of rat testes and H2O2-induced DNA damage in mouse testicular cells and beneficial effect on sexual behavior and reproductive function of hemicastrated rats. Life Sci. 2006; 79:613–621. PMID:
16563441.

7. Li X, Liu S, Ma X, Xu J. A study of the effect of ginsenosides on the secretion of gonadotropins. J Norman Bethune Univ Med Sci. 1988; 14:293–295.
8. Nan YY, Wang ZR, Lu ZF, Liu ML, Ma L, Li R, et al. Expression of P450arom CYP19 gonadal hormone levels and influence of the number of spermium in the testis of infertile rats with kidney-yang deficiency after treated by extractive of Cuscuta. J Liaoning Univ Tradit Chin Med. 2012; 14:20–25.
9. Ye Z, Chen D, Zhong J, Zhang Y, Zhang W, Wang G, et al. Effect of Jiawei Wuzi Yanzong decoction on sperm quality and hormone level. World Chin Med. 2013; 8:626–629.
10. Xie J, Wang J, Chen M, Liu H. Influence of Guilingji capsules on spermatogenesis and sexual hormones in oligospermatism rats. J Guangzhou Univ Tradit Chin Med. 2011; 28:621–623.
11. Zhang Y, Shen N, Qi L, Chen W, Dong Z, Zhao DH. Efficacy of Schizandra chinesis polysaccharide on cyclophosphamide induced dyszoospermia of rats and its effects on reproductive hormones. Chin J Integr Tradit West Med. 2013; 33:361–364.
12. Ma L, Jia M, Nan YY, Liu ML, Wang ZR, Ma J. Effects of Jingui Shenqi pills on sperm quality and contents of hormones in adenine-induced infertility rats. J Shandong Univ Tradit Chin Med. 2011; 35:431–433.
13. Ling Q, Ao Z, Xu Z, Xu Z, Yin G, Tao W. Effect of Liuweidihuang decoction on reproductive system of male rat. Chin Tradit Pat Med. 2004; 26:561–564.
14. Jiang Z, Wang J, Li X, Zhang X. Echinacoside and Cistanche tubulosa (Schenk) R. wight ameliorate bisphenol A-induced testicular and sperm damage in rats through gonad axis regulated steroidogenic enzymes. J Ethnopharmacol. 2016; 193:321–328. PMID:
27422164.

15. Yue GP, Chen Q, Dai N. Eighty-seven cases of male infertility treated by bushen shengjing pill in clinical observation and evaluation on its curative effect. Chin J Integr Tradit West Med. 1996; 16:463–466.
16. Rebourcet D, Darbey A, Monteiro A, Soffientini U, Tsai YT, Handel I, et al. Sertoli cell number defines and predicts germ and leydig cell population sizes in the adult mouse testis. Endocrinology. 2017; 158:2955–2969. PMID:
28911170.

17. Yang A, Liu B, Zhang S, Xie C, Li L, Zhou Q, et al. Mechanism of Wuziyanzong Pills in improvement of function of Sertoli cells in rats with insufficiency of kidney essence. J Beijing Univ Tradit Chin Med. 2010; 33:378–380. 384
18. Zhang SQ, Liu BX, Wang X, Li LQ, Zhang XP, Zhang T, et al. Effect of Wuziyanzong Pill medicated serum on secretion of rat sertoli cells in vitro. Chin J Tradit Chin Med Pharm. 2013; 28:631–634.
19. Xu YP, Liu BX, Zhang XP, Yang CW, Wang CH. A Chinese herbal formula, Wuzi Yanzong pill, improves spermatogenesis by modulating the secretory function of Sertoli cells. Chin J Integr Med. 2014; 20:194–199. PMID:
24615212.
20. Ke M, Liu B, Wang C, Pei X. Study on the effects of Wuzi Yanzong pill on semen quality and its related mechanism. Chin J Androl. 2016; 30:30–33.
21. Hu S, Li Y, Cao Y, Jian G, Guo J. Influence and mechanism of Wuzi Yanzong Wan on proliferation of Sertoli cells in infant rats. J Beijing Univ Tradit Chin Med. 2017; 40:917–922.
22. Wang QZ, Wang DF, Liu HL, Feng DJ, Wang HH, Guo ZB. Effects of extracts from Liuwei dihuang Pill on the proliferation of mouse Sertoli cells. Lishizhen Med Mat Medica Res. 2013; 24:1363–1365.
23. Gu Y, Zhang X, Sun D, Zhao H, Cai B, Gao C, et al. The stimulative effect of Yangjing capsule on testosterone synthesis through Nur77 pathway in Leydig cells. Evid Based Complement Alternat Med. 2015; 2015:408686. PMID:
26413123.

24. Xu Y, Wu B, Jiang Y. Effect of icariin on the proliferation, apoptosis and testosterone synthesis of immature rat Leydig cells. Mod J Integr Tradit Chin West Med. 2013; 22:2864–2866.
25. Nan Y, Zhang X, Yang G, Xie J, Lu Z, Wang W, et al. Icariin stimulates the proliferation of rat Sertoli cells in an ERK1/2-dependent manner in vitro. Andrologia. 2014; 46:9–16. PMID:
23134192.
26. Chen M, Hao J, Yang Q, Li G. Effects of icariin on reproductive functions in male rats. Molecules. 2014; 19:9502–9514. PMID:
24995929.

27. Wu ZQ, Chen DL, Lin FH, Lin L, Shuai O, Wang JY, et al. Effect of bajijiasu isolated from Morinda officinalis F. C. how on sexual function in male mice and its antioxidant protection of human sperm. J Ethnopharmacol. 2015; 164:283–292. PMID:
25686781.

28. Yang X, Ding CF, Zhang YH, Yan ZZ, Du J. Extract from Cuscuta chinensis against the structure of human sperm membrane and the oxidative injury of function. Chin Pharm J. 2006; 41:515–518.
29. Shi GJ, Zheng J, Wu J, Qiao HQ, Chang Q, Niu Y, et al. Beneficial effects of Lycium barbarum polysaccharide on spermatogenesis by improving antioxidant activity and inhibiting apoptosis in streptozotocin-induced diabetic male mice. Food Funct. 2017; 8:1215–1226. PMID:
28225103.

30. Yu HY, Chen ZY, Sun B, Liu J, Meng FY, Liu Y, et al. Lignans from the fruit of Schisandra glaucescens with antioxidant and neuroprotective properties. J Nat Prod. 2014; 77:1311–1320. PMID:
24927000.

31. Yin JL, Xu Y, Wu B. Wuziyanzong compound relieves oxidative stress injury and inhibits the apoptosis of Sertoli cells. Natl J Androl. 2013; 19:257–261.
32. Li WL, Dai Y, Xu D, Ji YB. Effects of different polar fractions from Jinkuishenqiwan on testosterone and oxidative stress in rats with kidney-yang deficiency induced by hydrocortisone. Chin J New Drugs. 2007; 16:1944–1946.
33. Zhou SH, Wen ZW, Liang AJ, Zhang ST. Experimental research on therapeutic efficacy of traditional chinese medicine Shengjing Capsule extracts in treating spermatogenesis impairment induced by oxidative stress. Med Sci Monit. 2016; 22:50–56. PMID:
26730959.

34. Weng Z, Zhou S, Liang A, Li L, Li TL, Zhang S. Effects of traditional Chinese medicine on spermatogenesis damage of rats caused by cigarette smoke exposure. Chin J Androl. 2016; 33:11–17.
35. Meng X, Lindahl M, Hyvönen ME, Parvinen M, de Rooij DG, Hess MW, et al. Regulation of cell fate decision of undifferentiated spermatogonia by GDNF. Science. 2000; 287:1489–1493. PMID:
10688798.

36. Yang WM, Kim HY, Park SY, Kim HM, Chang MS, Park SK. Cynomorium songaricum induces spermatogenesis with glial cell-derived neurotrophic factor (GDNF) enhancement in rat testes. J Ethnopharmacol. 2010; 128:693–696. PMID:
20219665.

37. Jin B, Cai B, Sun D, Zhang X, Cui Y, Deng W, et al. Yangjing capsule extract promotes proliferation of GC-1 spg cells via up-regulated POU3F1 pathway. Biosci Trends. 2017; 11:95–104. PMID:
28154340.
38. Xu W, Luo Z, Jin J, Wang Q, Jiang Y, Han B, et al. Establishment of cyclophosphamide-induced oligopermia mouse model and the curative effect of matrimony vine. Chin J Androl. 2015; 29:3–7.
39. Zhu Q, Xiao L, Yang J, Hou L, Zhang D. Effects of Jinguishenqi bolus on apoptosis of kidney-yang deficiency model of testicular cells from the Fas/FasL pathway. Lishizhen Med Materia Medica Res. 2017; 28:272–276.
40. Huang WF, Zhang CC, Liu J, Song LX, Peng B, Zhao HX. Protective effect of Wuzi Yanzong prescription on apoptosis in germ cells of mice induced by cyclophosphamide. Zhong Yao Cai. 2016; 39:1143–1147. PMID:
30133214.
41. Ma N, Zhao HX, Chen Q, Han GF, Liu ZC, Yuan D, et al. Protective effect of Wuzi Yanzong recipe on testicular DNA damage and apoptosis in natural ageing rats. Zhongguo Zhong Yao Za Zhi. 2018; 43:1675–1681. PMID:
29751716.
42. Zhang C, Wang Y, Xu K, Wang Z, Hou Y. Effect of different nourishing formulas on spermatogenic cell apoptosis of aging mice. Chin J Exp Tradit Med Formulae. 2018; 4:148–153.
43. Bray TM, Bettger WJ. The physiological role of zinc as an antioxidant. Free Radic Biol Med. 1990; 8:281–291. PMID:
2187766.

44. Sharif R, Thomas P, Zalewski P, Fenech M. The role of zinc in genomic stability. Mutat Res. 2012; 733:111–121. PMID:
21939673.

45. Flohé L. Selenium in mammalian spermiogenesis. Biol Chem. 2007; 388:987–995. PMID:
17937612.

46. Lapointe S, Ahmad I, Buhr MM, Sirard MA. Modulation of postthaw motility, survival, calcium uptake, and fertility of bovine sperm by magnesium and manganese. J Dairy Sci. 1996; 79:2163–2169. PMID:
9029354.

47. Zhao J, Dong X, Hu X, Long Z, Wang L, Liu Q, et al. Zinc levels in seminal plasma and their correlation with male infertility: a systematic review and meta-analysis. Sci Rep. 2016; 6:22386. PMID:
26932683.

48. Scott R, MacPherson A, Yates RW, Hussain B, Dixon J. The effect of oral selenium supplementation on human sperm motility. Br J Urol. 1998; 82:76–80. PMID:
9698665.

49. Yu NC, Guan JH. Study on trace elements in 8 kidney-tonifying Chinese medicines and their clinical efficacy. ShiZhen J Tradit Chin Med Res. 1997; 8:33–34.
50. Lin S, Zhao L, Dong S, An D. Determination of selenium in ten kinds of traditional Chinese medicine by fluorescence spectrophotometry. J China Pharm Univ. 1989; 20:46–47.
51. Zhou SH, Xie JX. The application of treating male diseases from the perspective of blood stasis. J New Chin Med. 2007; 39:97–98.
52. Dong W, Jin B, Sun D, Cai B, Deng W, Cui Y, et al. Bushenhuoxue prescription facilitates testicular microcirculation in dyszoospermia mice via activating VEGF/VEGFR2 pathway. Chin J Androl. 2018; 32:30–35.
53. Guo J, Wang F, Zhang Q, Geng Q, Yu GJ, Zhao JY, et al. Treatment of oligospermia/asthenozoospermia patients by three different Chinese medical principles: a randomized control clinical study. Chin J Integr Tradit West Med. 2013; 33:1170–1173.
54. Chen D, Zhong J, Chen S, Zhang Y, Zhang W, Wang G, et al. Effect of supplemented Wuzi Yanzong decoction on the quality of sperm and secretion of seminal fructose. J Tradit Chin Med. 2013; 54:401–404.
55. Sun ZG, Lian F, Jiang KP, Zhang JW, Ma FM, Zhang N, et al. Shengjing prescription improves semen parameters of oligoasthenozoospermia patients: efficacy and mechanism. Natl J Androl. 2012; 18:764–767.
56. Shang XJ, Guo J, Chen L, Deng CH, Sun XZ, Geng Q, et al. Qilin pills for oligoasthenospermia: a multi-centered clinical trial. Natl J Androl. 2011; 17:1139–1142.
57. Au C, Yeung W, Xu F. Meta-analysis on TCM diagnosis and treatment of oligoasthenospermia. Chin Arch Tradit Chin Med. 2015; 33:2268–2273.
58. Zhou JF, Li Q, Zhang QH, Lin RW, Chen ZQ, Xiang ST. Kidney-tonifying Chinese medicine for male infertility: a systematic review of randomized controlled trials. Natl J Androl. 2015; 21:833–840.
59. Jerng UM, Jo JY, Lee S, Lee JM, Kwon O. The effectiveness and safety of acupuncture for poor semen quality in infertile males: a systematic review and meta-analysis. Asian J Androl. 2014; 16:884–891. PMID:
25038176.

60. Purvis K, Christiansen E. Infection in the male reproductive tract. impact, diagnosis and treatment in relation to male infertility. Int J Androl. 1993; 16:1–13.

61. Lu F, He Q, Zhang B, Liu Z, Li L. Effects of Zhibai Dihuang decoction on expression of IL-2, TNF-α in the testis of rats infected by ureaplasma urealyticum. China J Tradit Chin Med Pharm. 2011; 26:448–450.
62. Upadhyaya M, Hibbard BM, Walker SM. Antisperm antibodies and male infertility. Br J Urol. 1984; 56:531–536. PMID:
6534457.

63. Mahony MC, Alexander NJ. Sites of antisperm antibody action. Hum Reprod. 1991; 6:1426–1430. PMID:
1770139.
64. Li X, Yu X, Liu J, Liao X, Miao Y. An Experimental Study of the effect of Zhibai Dihuang Decoction on immunological infertility. Tradit Chin Drug Res Clin Pharmacol. 1997; 8:83–85.
65. Wang W, Huang Z, Tang M, Li X, Chen Y, Chan M, et al. A histological and immunohistochemical study on MianBu I & II treating immunological infertility of male mice. Chin J Histochem Cytochem. 2001; 10:81–85.
66. Lun X. Effects of acutherapy on T lymphocyte subgroup classification in male immuno-infertility. J Beijing Univ TCM. 2004; 27:90–92.
67. Rajender S, Avery K, Agarwal A. Epigenetics, spermatogenesis and male infertility. Mutat Res. 2011; 727:62–71. PMID:
21540125.

68. Boissonnas CC, Abdalaoui HE, Haelewyn V, Fauque P, Dupont JM, Gut I, et al. Specific epigenetic alterations of IGF2-H19 locus in spermatozoa from infertile men. Eur J Hum Genet. 2010; 18:73–80. PMID:
19584898.

69. Lian F, Sun J, Guo L, Sun Z, Wu H. Effects of Shengjing Formula on the expression of H19 imprinted gene in infertile patients caused by oligoasthenospermia with kidney deficiency syndrome. J Tradit Chin Med. 2014; 55:1113–1116.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download