Abstract
Background
Several studies have shown that the presence of cerebrovascular lesions may play an important role for determining the severity of the clinical symptoms of dementia. But no study to date has explored the clinical effect of cerebrovascular disease in Parkinson's disease with dementia (PDD), although cerebrovascular disease is common causes of dementia in elderly population. Therefore we conducted this study to evaluate the relationship between silent cerebrovascular lesions and cognitive decline in PDD.
Methods
Only 27 patients with PDD were chosen; 17 patients had PDD with silent cerebral ischemic lesions (PDDI) and 10 patients had PDD without silent cerebral ischemic lesions (pure PDD). These subjects received the global cognitive function testing and were all evaluated with detailed neuropsychological tests including attention, memory, language, and also the visuospatial and frontal function.
Results
There were no significant differences between pure PDD and PDDI group on general cognitive functions tests. Regard to mean time duration of suffering from Parkinson motor symptoms and motor function scale, pure PDD group showed more long duration than PDDI group but there was no significant difference between two groups. Furthermore, there were not any significant differences between the two groups on detailed neuropsychological tests.
Conclusions
We concluded that silent cerebrovascular lesions do not contribute to neuropsychological severity of PDD, although vascular disease is a common cause of cognitive impairment in the elderly. Thus the results of the present study suggest that factors other than cerebrovascular disease contribute to severity of PDD.
Although most of patients with idiopathic Parkinson's disease (PD) have circumscribed cognitive impairment, only a proportion of them develop dementia [1]. The etiology of dementia in PD remains unknown yet. Cortical changes, including concomitant Alzheimer disease (AD) pathology, Lewy bodies, and frontal atrophy, may be involved in PD with dementia (PDD) [2, 3]. Subcortical pathologies, which may contribute to dementia in PD, include atrophy of the cholinergic nucleus basalis of Meynert, striatonigral degeneration, and involvement of the dopaminergic ventral tegmental area and other monoaminergic nuclei [3].
Cerebrovascular lesions are common in older persons and they are generally considered to be among the most common causes of dementia. Recently several studies have shown that the presence of cerebrovascular lesions may play an important role for determining the presence and severity of the clinical symptoms of AD, for lowering the threshold of the AD pathology that's required for the clinical expression of dementia [4, 5]. And cerebrovascular pathologies frequently coexist with AD and this combination may show synergistic effects on patients' cognitive decline, yet the results of the epidemiologic and clinico-pathologic studies on the relation between cerebrovascular disease and AD have been controversial [6]. In regard to PDD, no study to date has explored the clinical effect of cerebrovascular disease in patients with PDD, although cerebrovascular disease is most common causes of dementia as well as common disease in elderly population. Therefore we conducted this study to evaluate the clinical relationship between silent cerebral ischemic lesions and cognitive decline in patient with PDD.
The study was approved by the local ethics committee and each patient gave written informed consent for participation. We prospectively included all consecutive PD patients with complaints of memory disturbance, who presented to dementia clinic and the movement disorder clinic of Catholic Medical Center between May, 2007 and June, 2008. All consecutive patients underwent the brain magnetic resonance imaging (MRI) to evaluate brain lesions. And experienced radiologist and neurologist, who blinded to the neuropsychological findings and clinical features of all subjects, assessed all brain MRIs in consensus with regard to the presence of silent ischemic lesions.
Fifty-six subjects participated in this study and were performed general neuropsychological tests to exclude PD patients without dementia. Of 56 PD patients, 29 patients didn't have any history or symptoms of memory impairment, any other cognitive dysfunctions assessed by a dementia screening questionnaire and general dementia scale. Therefore only 27 PD patients with dementia features were chosen; 17 patients had PDD with silent cerebral ischemic lesions (PDDI) and 10 patients had PDD without silent cerebral ischemic lesions (pure PDD). And we evaluated motor function of each group by Hoehn and Yhar stage (H-Y stage). All of the subjects were also assessed by experienced neurologists at the dementia and memory clinic. The evaluation procedures other than brain MRI consisted of a detailed medical history, physical and neurological examinations, neuropsychological assessments and laboratory tests. The history of medical and neurological problems was obtained from the patient and their family members or from their other caregivers.
All the PD patients were diagnosed according to the United Kingdom Parkinson's Disease Society Brain Bank Clinical Diagnosis Criteria for Parkinson's Disease [7]. For all the PDD patients, the criteria for diagnosis of probable PDD by Emre et al. [8] were fulfilled and the onset of Parkinson disease preceded the development of dementia by at least 12 months. The pure PDD patients never had focal neurological signs and symptoms of cerebral disease. We also excluded those patients who were displaying markedly fluctuating cognition with pronounced variations in attention and alertness, and recurrent vivid hallucinations, those patients taking medications (e.g. anticholinergic agents) that have been reported to influence cognition and memory, those patients who had any signs of atypical parkinsonism and those patients who fulfilled the DSM-IV criteria for delirium or amnesic disorders and depressive disorders [9, 10]. Apart from the above mentioned exclusion criteria, we excluded patients with secondary causes of parkinsonism that would, in judgment of the investigators, interfere with the safe conduct of the study.
We defined silent cerebral ischemic lesions as evidence on the brain MRI of one or more ischemic lesions, without a history of a stroke or transient ischemic attack and neurological symptoms. If a prior stroke or transient ischemic attack did correspond with a lesion, we excluded the patients with these lesions from this study. All of the PDDI had few small ischemic white matter lesions with the exception of the sites of strategic infarction dementia. The lesions included in this study were defined as the size of the deep white matter and periventricular white matter lesions (extending cap or irregular halo) that were less than 10 mm, and the lacunar lesions had less than 5 lesion sites, but we excluded lesions involving medial and lateral cholinergic pathway and diffusely confluent hyperintensities (>25 mm, irregular shape) of white matter in this study [11-13]. These criteria were mainly based on brain imaging criteria for subcortical vascular dementia by Erkinjuntti et al. [11].
We also assessed stroke risk factors, such as hypertension, cigarette smoking, hypercholesterolemia, diabetes mellitus and heart diseases, by evaluating the patients' medical histories and laboratory findings to examine association of these factors between PDD and PDDI group.
The patients' general cognitive state and their severity of dementia were evaluated by means of the MMSE, CDR and sum of the box of CDR (SOB) [14-16]. Several cognitive domains were assessed by conducting a detailed neuropsychological battery of tests. This consisted of an attention test (forward digit span, backward digit span and letter cancellation), a language and related function test (spontaneous speech, comprehension, repetition, Boston Naming test, readings, writing, calculation, finger naming, right-left orientation, body part identification and praxis), a visuospatial function test (drawing interlocking pentagon and Rey complex figure copy test), a verbal memory test (registration and recall of 3-words, Seoul Verbal Learning Test (SVLT): immediate recall, delayed recall and recognition), and a frontal executive function test (contrasting program, go-no-go test, fist-edge-palm, alternating hand movement, alternating square and triangle, Luria loop, the Controlled Oral Word Association test: animal, supermarket and letters, and Color Word Stroop Test: word reading and color reading) [16-18].
The statistical analysis was performed with the SPSS software version 17.0 package and with using Mann-Whitney test for comparison of the variables' mean between the PDD and PD groups. Analyses between pure PDD and PDDI were also used Mann-Whitney test. Fisher's exact tests were used for comparison of the categorical variables between each group. And multiple linear regression analysis was performed to analyze affection of factors except for ischemic cerebral lesion on cognitive decline. Values are expressed as means with SD. Statistical significance was assumed for p values <0.05.
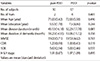
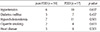
The number of subjects, the mean age, length of education, disease duration, MMSE, CDR score associated with SOB score and H-Y stage for pure PDD and PDDI group are presented in Table 1. These findings showed that there were no significant differences between pure PDD and PDDI group on general cognitive functions tests (MMSE, CDR score associated with SOB). Regard to mean time duration of suffering from Parkinson motor symptoms, pure PDD group showed more long duration than PDDI group but there was no significant difference between two groups (43.1±16.18 vs 32.2±17.78 months, respectively). Furthermore, each group was similar for their motor function scale assessed by H-Y stage (1.91±0.87 in pure PDD vs 1.97±1.09 in PDDI). The results of detailed neuropsychological tests for each group are summarized in Table 2 and Table 3. There were no significant differences between the pure PDD and PDDI groups for the most of cortical function domains, including language and related function tests, attention, apraxia test and memory function tests. Furthermore, there were not any significant differences between the two groups for all frontal executive function, which have frequently demonstrated impairment in patients with PDD. Even visuospatial function test, which is one domain out of cognitive domains that characterized in patients with PDD, also showed no significant differences between the two groups.
With regard to association of risk factors for ischemic lesions including hypertension, diabetes mellitus, cholesterol, cigarette smoking and heart disease, there was no significant association between pure PDD and PDDI (Table 4).
Multiple linear regression analysis showed that MMSE and CDR scores, which indicate the severity of cognitive decline, were not associated with age (respectively, p value=0.180 & 0.305), education (p value=0.708 & 0.673), duration of disease (p value=0.589 & 0.938) and duration of dementia (p value=0.699 & 0.592), significantly.
In the present pilot study, we investigated the characteristics of the cognitive profiles of patients with pure PDD and PDDI. And we attempted to clarify the influence of silent cerebral ischemic lesions on cognition on patients with PDD by using comprehensive neuropsychological tests. However, although previous studies suggested significant association between AD and cerebrovascular lesions [4, 19], we cannot find out sharp neuropsychological differences between patients with pure PDD and PDDI.
Generally, it is known that cerebrovascular disease is second most common cause of dementia and it has also has been suggested that AD may be primarily a vascular disorder [20, 21]. Previous study also reported that AD with cerebrovascular disease showed more severe cognitive decline than AD without cerebrovascular disease, indicating cerebrovascular disease contributes to the severity of cognitive decline [19]. Moreover, Ronchi et al. suggested that stroke is a strong risk factor for dementia and the hypothesis that a stroke event may near the beginning of dementia by about 10 years, possibly accelerating the progression from cognitive impairment/no dementia to dementia [22]. The Framingham study also demonstrated that stroke increased the risk of dementia 2.6 times in subjects aged up to 80 years, and 2.4 times in subjects who had completed high school [23]. However, few studies have examined the role of cerebrovascular risk factors for dementia in PD. A study by Salganik et al. [24] showed correlation between hypertension and dementia in a convenience sample of PD patients. But the authors found out no definite correlation between cerebrovascular disease or cardiovascular disease and dementia in these subjects [24]. Furthermore, recent large cohort study by Haugarvoll et al. [25] concluded that cerebrovascular risk factors do not contribute to dementia in patients with PD. In recent clinicopathological study on 97 PD brain donors, Papapetropoulos et al. [26] also reported that there was no association between ischemic cerebrovascular disease and specific phenotypic characteristics of PD including dementia. There are several potential factors contributed to PDD, such as advanced age, depression, presence of speech and axial involvement et al. [27]. Although the relative contribution of each of these factors is not known, previous several studies suggest that cortical Lewy bodies is the most important cause of PDD [25, 28, 29]. In accordance with above-mentioned several previous studies, we might also conclude that cerebral ischemic lesions do not contribute to neuropsychological severity of PDD in the current study, although vascular disease is a common cause of cognitive impairment and dementia in the elderly [25]. Thus this finding could also suggest that factors other than cerebrovascular disease contribute to severity of PDD. Furthermore this conclusion is consistent with the finding that cerebrovascular disease is rare in patients with dementia with Lewy bodies [30].
This study had several limitations. First, this study was not large-scale longitudinal study and second, this study was the use of PDD diagnostic criteria that have not yet been validated. And differentiating between PDD and dementia with Lewy bodies on the basis of clinical criteria is difficult. Additionally, we cannot be certain about the accuracy of our clinical diagnosis because of the lack of the neuropathologic confirmation, because the patients were still alive. The major strength of this study is that comprehensive neuropsychological tests for dementia features and neurological examination for parkinsonian features were performed on all of the PDD patients by experts in each clinic.
In conclusion, the result of the present study suggested that silent cerebral ischemic lesions were not contributed to neuropsychological severity of PDD, indicating that the PD-related degenerative brain changes are the main causes of dementia in PD. We could also think that PDD is less influenced by a reduction of the cognitive reserve induced by cerebrovascular lesions without cholinergic pathway involvement than AD and vascular dementia. However, to clarify this assumption, clinicopathologic studies and studies using magnetic resonance imaging, involving large cohort of PD patients, are needed to further explore the relative contribution of vascular and neurodegnenrative factors on PDD.
Figures and Tables
Table 2
Neuropsychological test results in the pure PDD and PDDI groups

values are expressed as mean(standard deviation).
BNT, Korean-Boston Naming test; SVLT, Seoul Verbal Learning Test; COWAT, controlled oral word association test; pure PDD, Parkinson's disease dementia without silent cerebral ischemic lesions; PDDI, Parkinson's disease with concomitant silent cerebral ischemic lesions.
References
1. Mayeux R, Denaro J, Hemenegildo N, Marder K, Tang MX, Cote LJ, et al. A population-based investigation of Parkinson's disease with and without dementia. Relationship to age and gender. Arch Neurol. 1992; 49:492–497.
2. Jellinger KA. Prevalence of Alzheimer lesions in Parkinson's disease. Mov Disord. 2003; 18:1207–1208.
3. Aarsland D, Andersen K, Larsen JP, Lolk A, Nielsen H, Kragh-Sørensen P. Risk of dementia in Parkinson's disease: a community-based, prospective study. Neurology. 2001; 56:730–736.
4. Vermeer SE, Prins ND, den Heijer T, Hofman A, Koudstaal PJ, Breteler MM. Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med. 2003; 348:1215–1222.
5. Lee JH, Olichney JM, Hansen LA, Hofstetter CR, Thal LJ. Small concomitant vascular lesions do not influence rates of cognitive decline in patients with Alzheimer disease. Arch Neurol. 2000; 57:1474–1479.
6. Jellinger KA, Mitter-Ferstl E. The impact of cerebrovascular lesions in Alzheimer disease--a comparative autopsy study. J Neurol. 2003; 250:1050–1055.
7. Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992; 55:181–184.

8. Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, et al. Clinical diagnostic criteria for dementia associated with Parkinson's disease. Mov Disord. 2007; 22:1689–1707.

9. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. ed 4. Washington: American Psychiatric Association;1994. p. 143–147.
10. McKeith IG, Dickson DW, Lowe J, Emre M, O'Brien JT, Feldman H, et al. Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology. 2005; 65:1863–1872.
11. Erkinjuntti T, Inzitari D, Pantoni L, Wallin A, Scheltens P, Rockwood K, et al. Research criteria for subcortical vascular dementia in clinical trials. J Neural Transm Suppl. 2000; 59:23–30.

12. Roman GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC, Garcia JH, et al. Vascular dementia: diagnostic criteria for research studies. Report of the NINDSAIREN International Workshop. Neurology. 1993; 43:250–260.

13. Selden NR, Gitelman DR, Salamon-Murayama N, Parrish TB, Mesulam MM. Trajectories of cholinergic pathways within the cerebral hemispheres of the human brain. Brain. 1998; 121:2249–2257.

14. Kang Y, Na DL, Hahn SH. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997; 15:300–308.

15. Choi SH, Na DL, Lee BH, Hahm DS, Jeong JH, Yoon SJ, et al. Estimating the validity of the Korean version of expanded clinical dementia rating (CDR) scale. J Korean Neurol Assoc. 2001; 19:585–591.
16. Kang YW. Samsung neuropsychological screening battery. In : Kang YW, editor. Current Research in Dementia. Seoul: The Korean Dementia Association;1998. p. 99–107.
17. Kim H, Na DL. Korean-Boston Naming Test. Seoul: Hakji Co;1997.
18. Kim H, Kim EY, Na DL. Naming deficits in patients with dementia of the Alzheimer type: error analysis of the Korean version of the Boston Naming Test. J Korean Neurol Assoc. 1997; 15:1012–1021.
19. Song IU, Kim JS, Kim YI, Eah KY, Lee KS. Clinical significance of silent cerebral infarctions in patients with Alzheimer disease. Cogn Behav Neurol. 2007; 20:93–98.

20. O'Brien JT, Erkinjuntti T, Reisberg B, Roman G, Sawada T, Pantoni L, et al. Vascular cognitive impairment. Lancet Neurol. 2003; 2:89–98.

21. Honig LS, Kukull W, Mayeux R. Atherosclerosis and AD: analysis of data from the US National Alzheimer's Coordinating Center. Neurology. 2005; 64:494–500.

22. De Ronchi D, Palmer K, Pioggiosi P, Atti AR, Berardi D, Ferrari B, et al. The combined effect of age, education, and stroke on dementia and cognitive impairment no dementia in the elderly. Dement Geriatr Cogn Disord. 2007; 24:266–273.

23. Ivan CS, Seshadri S, Beiser A, Au R, Kase CS, Kelly-Hayes M, et al. Dementia after stroke: the Framingham Study. Stroke. 2004; 35:1264–1268.

24. Salganik I, Korczyn A. Risk factors for dementia in Parkinson's disease. Adv Neurol. 1990; 53:343–347.

25. Haugarvoll K, Aarsland D, Wentzel-Larsen T, Larsen JP. The influence of cerebrovascular risk factors on incident dementia in patients with Parkinson's disease. Acta Neurol Scand. 2005; 112:386–390.

26. Papapetropoulos S, Gonzalez J, Mash DC. The effect of ischemic cerebrovascular disease on the clinical characteristics of Parkinson's disease. A post-mortem study. Eur J Neurol. 2006; 13:96–97.

27. Emre M. Dementia associated with Parkinson's disease. Lancet Neurol. 2003; 2:229–237.
28. Hurtig HI, Trojanowski JQ, Galvin J, Ewbank D, Schmidt ML, Lee VM, et al. Alpha-synuclein cortical Lewy bodies correlate with dementia in Parkinson's disease. Neurology. 2000; 54:1916–1921.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download