INTRODUCTION
Following the widespread implementation of the rotavirus vaccine, the incidence of rotaviral enteritis has declined. However, enteritis with a bacterial etiology, such as that caused by
Salmonella,
Campylobacter, enteropathogenic
Escherichia coli, enterohemorrhagic
E. coli, is emerging as a major issue in clinical field.
1) Recently, the clinical application of polymerase chain reaction (PCR) has contributed to the precise molecular biological diagnosis of infectious agents, facilitating the investigation of detailed clinical presentations leading to therapeutic advancements, from an empirical to a pathogen-specific approach.
Campylobacter species are gram-negative, comma- or S-shaped rods that causes zoonotic infections. They can be transmitted via the fecal-oral route, by person-person contact, or by ingestion of undercooked contaminated poultry, meat, or milk.
Campylobacter enteritis was introduced as a new disease by Skirrow
2) in 1977, and various studies on
Campylobacter enteritis have been published worldwide for over 40 years.
Campylobacter infection is known to be a major cause of acute diarrhea. The most common clinical symptoms are fever, bloody diarrhea and colicky abdominal pain. Abdominal pain is continuous, and radiates to the right iliac fossa, mimicking acute appendicitis.
3) Most of these studies are confined to adults, and studies in children are limited.
Recent studies have shown a significant increase in the rate of
Campylobacter isolated from pediatric enteritis patients, compared with
E. coli or
Salmonella.
12) However, there have been limited studies that include patient cohort sizes larger than 100
Campylobacter enteritis in children in Korea. The present investigation was undertaken to describe the clinical and laboratory features of
Campylobacter enteritis diagnosed at the Nowon Eulji Medical Center (NEMC) over a period of 6 years.
DISCUSSION
This study aims to bring clinical and laboratory feature about
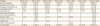
Campylobacter enteritis in children including patient cohort sizes larger than 100, first in Korea. We present result of our study of data totaling 123
Campylobacter enteritis cases retrospectively from 1,396 gastroenteritis patients. In this study, we aimed to identify the pathogen of enteritis by two flows. The first flow, EnterNet was only epidemiologic purpose, not intended for clinical care because the test results could be confirmed several weeks later. On the other hand, multiplex PCR, the second flow, was used to diagnose and treat the children immediately after receiving the stool specimen within one day. In the first flow, stool specimens were examined for both viral and bacterial etiology. Particularly during testing for bacterial pathogens, stool culture was performed first, followed by PCR in fecal specimens with positive results. Specimens with a negative final PCR despite a positive bacterial culture result were reported as negative. The prevalence of
Campylobacter enteritis was 4.3% in EnterNet (
Table 1). There was no comparable study of the proportion patients with
Campylobacter enteritis in enteritis, it is difficult to determine whether the prevalence of
Campylobacter enteritis was real. Because we stored stool samples at refrigerator temperature (4°C) and sent them only once a week to PHERI, we guess the sensitivity could be low. The male to female ratio of
Campylobacter enteritis in children has been reported around 6:4,
45) which is slightly different with the 5:5 ratio observed in the current study. According to previous study, two peaks in age distribution of
Campylobacter enteritis were observed: in children (aged 1 to 4 years) and in young adolescents (aged 15 to 24 years).
6) Interestingly, the second peak was not observed in
Shigella or
Salmonella enteritis and unique to
Campylobacter enteritis.
6) In the present study, it was difficult to identify the second peak because of age range difference from the previous study. And there was difference in culture by country and poultry consumption patterns. In this study, the highest incidence of
Campylobacter enteritis in school-aged children and young adolescents was observed only once, different with the two peaks of the previous study. This result was common with age distribution of bacterial enteritis, which was contrasted with the highest incidence of viral enteritis in children aged under 5 years.
In China,
Campylobacter enteritis peaks between late spring and summer and a lower second peak is observed in late autumn.
4) Previous studies
457) reported a disease peak between May and October, representing 95.0% of annually cases of
Campylobacter enteritis. In the current study, a comparable peak was observed between May and October, accounting for 79.7% of cases with
Campylobacter enteritis.
Campylobacter infection includes acute enteritis, sepsis, and extra-intestinal local infection.
Campylobacter spp. is well recognized major cause of acute enteritis.
8) After a latent period of 1 to 7 days,
Campylobacter spp. induces periumbilical pain, diarrhea, or mucous and bloody stools. Nausea is a common manifestation across all ages, whereas vomiting frequently occurs at a younger age.
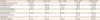
9) Surgical abdomen, such as appendicitis or intussusception, is characterized by a similar presentation. Clinical symptoms were comparable to those in previous studies. Diarrhea, fever, and abdominal pain were observed in a majority of the younger patients. Other symptoms included headache, vomiting, and macroscopic hematochezia.
WBC levels over 10,000/mm
3 were observed in 67 patients (57.3%), with 19 patients over 15,000/mm
3 (16.2%). And few of the patients (58 cases, 47.2%) the CRP levels were significantly elevated (over 1.2 mg/dL).
10) Moreover, in 45 patients (36.6%), the CRP level was above 3.5 mg/dL,
10) which represents screening points for bacterial infections. Kim et al.
1) reported that CRP levels were higher in patients infected with
Salmonella spp. or
Campylobacter spp. than in those infected with
S. aureus or pathogenic
E. coli. Marked rise of CRP in
Campylobacter infection was observed in the current study, and is consistent with the findings of previous reports.
1)
In the majority of patients, imaging findings were diffuse edematous wall thickening of the colon and reactive mesenteric lymph nodes, indicative of enterocolitis. Yoon
11) found that enteritis caused by
Campylobacter spp. and
Salmonella spp. involved edematous changes in the terminal ilium and proximal colon, which may include involvement of the whole colonic wall. Furthermore, according to the previous study,
11) ultrasound findings include hypoechoic luminal wall thickening and increased Doppler blood flow to mucosa due to inflammation, which may be associated with large hypertrophic mesenteric lymph nodes. This finding is consistent with the results of abdominal enhanced CT and abdominal sonography in this study.
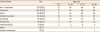
The first line therapy of
Campylobacter enteritis is IV hydration and conservative management. Consistently with the previous research, this study showed that the early initiation of a 3-day-regimen of azithromycin could improve prognosis.
1213) So, azithromycin use can be considered in pediatric patients with severe suspected
Campylobacter enteritis. In this study, IV ceftriaxone was often prescribed as the antibiotic of choice in pediatric patients with high CRP levels because of the possibility of
Salmonella-induced sepsis. However, Kim et al.
1) reported that there were 22 cases (12%) of
Salmonella infection of 183 diagnosed cases of bacterial enteritis, but no cases of
Salmonella-induced sepsis were reported. Furthermore, the present study showed that the use of azithromycin was significantly associated with hospitalization within 3 days (
P<0.05). Therefore, azithromycin can be considered as the first choice of antibiotics in pediatric patients with enteritis, with clinically severe symptoms and high CRP levels, in order to cover the possibility of infection with bacterial pathogen, such as
Campylobacter spp. and
Salmonella spp.
Recurrent infection was suspected in one patient. The first episode manifested as a 3-week history of continuous diarrhea and the patient was treated with azithromycin. The patient complained of on-going abdominal pain following the completion of the antibiotic regimen, although the pain subsequently decreased. Two months later, the patient was diagnosed with recurrent
Campylobacter enteritis again, although with milder symptoms. Azithromycin was administered, which led to the resolution of symptoms with no complications. The incubation period of Campylobacterium is between 2 and 7 weeks in the feces of patients with
Campylobacter enteritis in the absence of antibiotic administration. In this case, antibiotics were administered during the first infection. Second,
Campylobacter was positive in stool culture and on PCR analysis after 9 weeks. In developing countries, recurrent infection has been reported in children, but it is rarely found in adults, who are considered to have been immunized through repeated infection.
14) The recurrent infections in the 11-year-old boy in this study were also consistent with the findings of previous studies.
Food-borne infection, particularly due to undercooked meat, unpasteurized milk, and poultry, is the leading cause of
Campylobacter enteritis.
151617) Once infected, the host can contribute to the propagation of the pathogen for weeks to months. Furthermore, as neonates are vulnerable to all kinds of direct contact with infected sources, such as pets, meat products, or even diapers from daycare centers, careful history taking is crucial.
18) Breast feeding is recommended in infants' owing to its protective effects.
19) The 9-month-old patient in this study was fed with formula and delivered weaning food available in market.
The current study was a single institution study, and the study population does not represent the general Korean pediatric patients. However, the significance of this study lies in the fact that we analyzed more than 100 pediatric patients with Campylobacter and observed their clinical progress with accumulated data for 6 years. The complication and recurrence rates may be lower than those observed because of the follow-up losses, which frequently occur in retrospective studies. We reported several complications following Campylobacter infection and prospective cohort study may also be warranted in the future.
Selection bias could have affected the result as NEMC is the secondary hospital with an emergency department, which means that patients with more severe enteritis attend the hospital. So, treatment by using antibiotics had to be considered frequently in current study, allowing for the severity of the laboratory findings and symptoms such as fever, abdominal pain. Furthermore, it is not a standard practice to consider PCR routinely or in patients with milder symptoms.
Campylobacter spp. is a major cause of bacterial enteritis in pediatric patients. It commonly occurs in summer, and most often affects young adolescents. Clinical symptoms are of relatively severe and includes high fever, diarrhea, headache, and severe abdominal pain, with bloody stool. A thorough understanding of the clinical presentation of Campylobacter enteritis and early suspicion in pediatric patients may minimize unnecessary CT scanning and enable the appropriate initiation of an azithromycin regimen, potentially shortening the duration of symptoms and lowering the rate of complications. As the number of patients diagnosed with Campylobacter enteritis increases, future approaches are suggested to include a stool culture and antibiotic susceptibility testing of Campylobacter spp. that can help identify the infection source and to perform a prospective randomized controlled study that can compare antibiotic administration effects.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download