Abstract
Background
Alzheimer's disease (AD) is a representative neurodegenerative disorder associated with memory disturbance. Recent research has shown that risk factors for cerebrovascular disorders are also causes of dementia. Of these risk factors, hyperhomocysteinemia is well known to be positively correlated with all types of dementias including AD. But it is not clear if there is a difference in the concentration of homocysteine according to subtypes of memory impairment of AD. We performed this study to explore the relationship between homocysteine and memory.
Methods
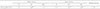
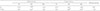
A total of 54 patients (male: 15 patients) to the dementia clinic at our hospital were recruited for this study. All subjects underwent neuropsychological tests including detailed memory function tests and brain magnetic resonance images. The plasma homocysteine level was measured routinely in all patients.
Results
Verbal and visual memories in AD were significantly associated with the concentration of plasma homocysteine. The plasma homocysteine level was significantly correlated with delayed recalls of verbal and visual memories and recognition of visual memory. However, there was no relationship between plasma homocysteine and working memory.
Figures and Tables
References
2. Oulhaj A, Refsum H, Beaumont H, Williams J, King E, Jacoby R, et al. Homocysteine as a predictor of cognitive decline in Alzheimer's disease. Int J Geriatr Psychiatry. 2010; 25:82–90.

3. Seshadri S. Elevated plasma homocysteine levels: Risk factor or risk marker for the development of dementia and Alzheimer's disease? J Alzheimers Dis. 2006; 9:393–398.

4. Honig LS, Tang MX, Albert S, Costa R, Luchsinger J, Manly J, et al. Stroke and the risk of Alzheimer disease. Arch Neurol. 2003; 60:1707–1712.

5. Lehmann M, Gottfries CG, Regland B. Identification of cognitive impairment in the elderly: Homocysteine is an early marker. Dement Geriatr Cogn Disord. 1999; 10:12–20.

7. Quadri P, Fragiacomo C, Pezzati R, Zanda E, Forloni G, Tettamanti M, et al. Homocysteine, folate, and vitamin B-12 in mild cognitive impairment, Alzheimer disease, and vascular dementia. Am J Clin Nutr. 2004; 80:114–122.

8. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: Report of the NINCDS-ADRDA work group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984; 34:939–944.

9. Kang Y, Na DL, Hahn S. A validitiy study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997; 15:300–308.

10. Choi SH, Lee BH, Hahm DS, Jeong JH, Yoon SJ. Estimating the validity of the Korean version of Expanded Clinical Dementia Rating (CDR) scale. J Korean Neurol Assoc. 2001; 19:585–591.

11. Martignoni E, Tassorelli C, Nappi G, Zangaglia R, Pacchetti C, Blandini F. Homocysteine and Parkinson's disease: a dangerous liaison? J Neurol Sci. 2007; 257:31–37.

12. Ho PI, Collins SC, Dhitavat S, Ortiz D, Ashline D, Rogers E, et al. Homocysteine potentiates beta-amyloid neurotoxicity: role of oxidative stress. J Neurochem. 2001; 78:249–253.

13. Fuso A, Nicolia V, Cavallaro RA, Ricceri L, D'Anselmi F, Coluccia P, et al. B-vitamin deprivation induces hyperhomocysteinemia and brain s-adenosylhomocysteine, depletes brain s-adenosylmethionine, and enhances ps1 and bace expression and amyloid-beta deposition in mice. Mol Cell Neurosci. 2008; 37:731–746.

14. Pacheco-Quinto J, Rodriguez de Turco EB, DeRosa S, Howard A, Cruz-Sanchez F, Sambamurti K, et al. Hyperhomocysteinemic Alzheimer's mouse model of amyloidosis shows increased brain amyloid beta peptide levels. Neurobiol Dis. 2006; 22:651–656.

15. Sontag E, Nunbhakdi-Craig V, Sontag JM, Diaz-Arrastia R, Ogris E, Dayal S, et al. Protein phosphatase 2a methyltransferase links homocysteine metabolism with tau and amyloid precursor protein regulation. J Neurosci. 2007; 27:2751–2759.

16. Zhuo JM, Wang H, Pratico D. Is hyperhomocysteinemia an Alzheimer's disease (AD) risk factor, an AD marker, or neither? Trends Pharmacol Sci. 2011; 32:562–571.

17. Blasko I, Grubeck-Loebenstein B. Role of the immune system in the pathogenesis, prevention and treatment of Alzheimer's disease. Drugs Aging. 2003; 20:101–113.
18. Karabag T, Kaya A, Temizhan A, Koc F, Yavuz S, Cam S. The influence of homocysteine levels on endothelial function and their relation with microvascular complications in T2DM patients without macrovascular disease. Acta Diabetol. 2007; 44:69–75.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download