Abstract
Purpose
To report a case of a cyclodialysis cleft that was successfully managed with gonioscopically guided transscleral cyclopexy using partial-thickness scleral flap.
Case summary
A 44-year-old man complaining of blurred vision in the left eye after blunt trauma was referred to our hospital. The intraocular pressure (IOP) was 4 mmHg and the visual acuity was counting finger. Gonioscopy examination revealed cyclodialysis cleft from 3 to 6 o'clock and fundus examination revealed macular folds. After the failure of conservative medical therapy and laser photocoagulation, gonioscopically guided transscleral cyclopexy using partial-thickness scleral flap was performed. Four months later, the IOP was 18 mmHg, the visual acuity was 0.8, and fundus examination showed the disappearance of the macular folds.
Figures and Tables
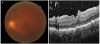 | Figure 1Preoperative fundus photography and optical coherence tomography. (A) Fundus photograph showing chorioretinal folds at macular area. (B) Optical coherence tomography showing wrinkling of the retina and the choroid. |
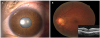
 | Figure 2Surgical procedures of transscleral cyclopexy using partial-thickness scleral flap. (A) A partial thickness scleral flap was created at the site of the cleft. (B) Cyclodialysis cleft was observed using Zeiss 4-mirror (Carl Zeis Meditec AG) gonioprism. (C) Cleft was closed with 10-0 nylon suture passing through the sclera and the detached ciliary body. (D) The cleft was closed completely with interrupted 10-0 nylon sutures. |
References
1. González-Martín-Moro J, Contreras-Martín I, Muñoz-Negrete FJ, et al. Cyclodialysis: an update. Int Ophthalmol. 2017; 37:441–457.


2. Ioannidis AS, Barton K. Cyclodialysis cleft: causes and repair. Curr Opin Ophthalmol. 2010; 21:150–154.


3. Kato T, Hayasaka S, Nagaki Y, Matsumoto M. Management of traumatic cyclodialysis cleft associated with ocular hypotony. Ophthalmic Surg Lasers. 1999; 30:469–472.


4. Küchle M, Naumann GO. Direct cyclopexy for traumatic cyclodialysis with persisting hypotony. Report in 29 consecutive patients. Ophthalmology. 1995; 102:322–333.

5. Chadha N, Lamba T, Belyea DA, Merchant KY. Indirect cyclopexy for treatment of a chronic traumatic cyclodialysis cleft with hypotony. Clin Ophthalmol. 2014; 8:591–594.



6. Feiler DL, Browne AW, Rachitskaya AV, et al. Indirect cyclopexy for repair of cyclodialysis clefts. Retina. 2018.

7. Rodrigues IA, Shah B, Goyal S, Lim KS. Gonioscopically guided nonpenetrating cyclodialysis cleft repair: a novel surgical technique. J Curr Glaucoma Pract. 2017; 11:31–34.



8. Kim CS, Ahn SI, Ahn BH. Treatment for persistent hypotony due to cyclodialysis. J Korean Ophthalmol Soc. 1998; 39:1505–1515.
9. Kim KH, Kim JW, Oh TH, Lee DH. Surgical repair of traumatic cyclodialysis with persistent hypotony. J Korean Ophthalmol Soc. 1997; 38:1294–1299.
10. Ahn K, Kee C. Clinical manifestations of cyclodialysis cleft and prognostic factors associated with direct cyclopexy. J Korean Ophthalmol Soc. 2003; 44:2328–2335.
11. Helbig H, Foerster MH. Management of hypotonous cyclodialysis with pars plana vitrectomy, gas tamponade, and cryotherapy. Ophthalmic Surg Lasers. 1996; 27:188–191.


12. Ishida Y, Minamoto A, Takamatsu M, et al. Pars plana vitrectomy for traumatic cyclodialysis with persistent hypotony. Eye (Lond). 2004; 18:952–954.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download