Abstract
Purpose
When there is a mass in the superior temporal orbit area, a lacrimal gland tumor should be suspected. We report a rare case of orbital lymphatic malformation that was histologically diagnosed in a patient with typical clinical features of the lacrimal gland.
Case summary
A 55-year-old female with no underlying disease and no ophthalmic history visited our clinic with a right upper eyelid edema associated with an enlarged painless eyelid mass 1 month prior to her visit. The patient stated that she discovered the mass 1 year previously.The palpebral lobe of the lacrimal gland protruded slightly with congestion of the surrounding conjunctiva. Enhanced computed tomography showed a 3 cm well-defined heterogeneous mass in the right lacrimal gland area and several well-defined round calcifications within the mass. Orbital tissue or bone involvement was not observed. The pleomorphic adenoma of the lacrimal gland was the most clinically suspicious, so complete resection of the mass was performed using lateral orbitotomy. Histopathologically, lymphangioma (lymphatic malformation) originating from the lacrimal gland was diagnosed.
Figures and Tables
Figure 1
Clinical photograph. (A) Moderate firm, palpable mass with eyelid swelling (black arrow) is seen at right upper eyelid. (B) Prominent palpebral lobe of lacrimal gland with mild conjunctival injection (white arrow) is seen.
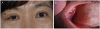
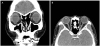
Figure 2
Preoperative enhanced computed tomography images of coronal view (A) and axial view (B). A 3 cm well-defined heterogeneous mass at right lacrimal gland area, and several well-marginated round calcifications within mass.
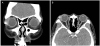
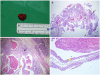
Figure 3
Gross findings and pathologic findings of the excised mass. (A) Gross findings of the excised mass measuring approximately 2.0 × 1.5 cm in diameter. (B–D) Pathologic findings. Microscopic examination of the removed tumor showed multiple dilated cystic spaces (red arrows) lined with thin-walled endothelium (yellow star) with myxoid degeneration. Note that normal lacrimal glandular cells (black arrows) are observed in the mass (B: Hematoxylin and eosin stain [H&E stain], ×10, C: H&E stain, ×40, D: H&E stain, ×100).
References
1. von Holstein SL, Rasmussen PK, Heegaard S. Tumors of the lacrimal gland. Semin Diagn Pathol. 2016; 33:156–163.


2. Andreasen S, Esmaeli B, Holstein SL, et al. An update on tumors of the lacrimal gland. Asia Pac J Ophthalmol (Phila). 2017; 6:159–172.


3. Bagheri A, Amoohashemi N, Salour H, Yazdani S. Lacrimal gland lymphangioma: report of a case and review of literature. Orbit. 2012; 31:197–199.


4. Harris GJ, Sakol PJ, Bonavolontà G, De Conciliis C. An analysis of thirty cases of orbital lymphangioma. Pathophysiologic considerations and management recommendations. Ophthalmology. 1990; 97:1583–1592.

5. Rootman J, Heran MK, Graeb DA. Vascular malformations of the orbit: classification and the role of imaging in diagnosis and treatment strategies*. Ophthalmic Plast Reconstr Surg. 2014; 30:91–104.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download