Abstract
Purpose
To evaluate the efficacy of surgical treatment for a lamellar macular hole in highly myopic patients.
Methods
We retrospectively analyzed 31 eyes of 31 patients with a high myopia, who underwent 23-gauge vitrectomy and inner limiting membrane peeling after diagnosis of a lamellar macular hole. Thirty-two eyes of 32 patients with no high myopia were selected as the control group. The best-corrected visual acuity (BCVA) was checked and optical coherence tomography was used to evaluate structural changes in the lamellar macular hole before surgery, 6 months, 12 months, and 24 months after surgery.
Results
The high myopia group and the control group showed statistically significant differences between preoperative BCVA and central foveal thickness. The success of primary surgery was 96.77% in the high myopia group and 100% in the control group. At postoperative 24 months, the high myopia group showed significantly poorer BCVA, and a statistically significant difference in the central foveal thickness and the inner and outer diameters of the lamellar macular hole. In cases of foveoschisis or a very high degree of myopia of more than -8.0 diopters, there was no significant improvement in BCVA after surgery.
Conclusions
Surgical treatment of a lamellar macular hole associated with a high degree of myopia showed excellent surgical success, but was as statistically significant as surgical treatment of non-myopia eyes. Early surgical treatment can be considered for a lamellar macular hole associated with a high degree of myopia when preoperative visual acuity and macular architecture are preserved.
Figures and Tables
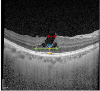 | Figure 1Preoperative parameters of spectral-domain optical coherence tomography. The red arrow indicates the inner diameter of the lamellar macular hole. The blue arrow indicates the outer diameter of the lamellar macular hole. The green arrow indicates the diameter of foveoschisis. The yellow arrow indicates the central foveal thickness. |
 | Figure 2The anatomical changes of the lamellar macular hole after surgery in a patient with high myopia (axial length = 30.57 mm, spherical equivalent = −16.63). (A) Preoperative fundus photograph and spectral-domain optical coherence tomography show the tigroid fundus and lamellar macular hole (LMH). (B) After 6 months postoperatively, LMH is well recovered to nearly regular foveal contour, and the measured central foveal thickness is 141 µm. (C) After 12 months postoperatively, recovered LMH is maintained, and the measured central foveal thickness is slightly decreased to 134 µm. (D) After 24 months postoperatively, the foveal contour remains stable, and the measured central foveal thickness is slightly decreased to 124 µm. |
 | Figure 3The anatomical changes of the lamellar macular hole after surgery in a patient with no high myopia (axial length = 23.67 mm, spherical equivalent = −0.50). (A) Preoperative fundus photograph and optical coherence tomography (OCT) show the lamellar macular hole (LMH) with epiretinal membrane (ERM). (B) After 6 months postoperatively, There is no apparent ERM both in fundus photograph and OCT, foveoschisis is resolved, and the foveal contour shows the appearance of pseudohole and the measured central foveal thickness is 204 µm. (C) After 12 months postoperatively, recovered LMH is maintained and the measured central foveal thickness is slightly decreased to 190 µm. (D) After 24 months postoperatively, the foveal contour remains stable, and the measured central foveal thickness is 214 µm. |
Table 2
The comparison of postoperative anatomical and functional changes of the lamellar macular hole with and without high myopia

Table 3
Associations of final visual acuity with demographic and clinical variables by multiple linear regression analyses in the high myopia group

Table 4
Differences of the demographic and clinical factors according to the presence of foveoschisis in the high myopia group

References
1. Gass JD. Lamellar macular hole: a complication of cystoid macular edema after cataract extraction: a clinicopathologic case report. Trans Am Ophthalmol Soc. 1975; 73:231–250.

2. Witkin AJ, Ko TH, Fujimoto JG, et al. Redefining lamellar holes and the vitreomacular interface: an ultrahigh-resolution optical coherence tomography study. Ophthalmology. 2006; 113:388–397.



3. Theodossiadis PG, Grigoropoulos VG, Emfietzoglou I, et al. Evolution of lamellar macular hole studied by optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2009; 247:13–20.


4. Spaide RF. Closure of an outer lamellar macular hole by vitrectomy: hypothesis for one mechanism of macular hole formation. Retina. 2000; 20:587–590.


5. Hirakawa M, Uemura A, Nakano T, Sakamoto T. Pars plana vitrectomy with gas tamponade for lamellar macular holes. Am J Ophthalmol. 2005; 140:1154–1155.


6. Kokame GT, Tokuhara KG. Surgical management of inner lamellar macular hole. Ophthalmic Surg Lasers Imaging. 2007; 38:61–63.


7. Garretson BR, Pollack JS, Ruby AJ, et al. Vitrectomy for a symptomatic lamellar macular hole. Ophthalmology. 2008; 115:884–886.


8. Lee SJ, Jang SY, Moon D, et al. Long-term surgical outcomes after vitrectomy for symptomatic lamellar macular holes. Retina. 2012; 32:1743–1748.


9. Rishi P, Kothari A. Lamellar macular hole: a new indication for vitrectomy with ilm peeling? Retin Cases Brief Rep. 2008; 2:272–273.


10. Michalewska Z, Michalewski J, Odrobina D, et al. Surgical treatment of lamellar macular holes. Graefes Arch Clin Exp Ophthalmol. 2010; 248:1395–1400.


11. Holland L, Chen JC, Lee LR. Anatomical and functional outcomes of pars plana vitrectomy for lamellar macular defects. Asia Pac J Ophthalmol (Phila). 2015; 4:134–139.


12. Sanisoglu H, Elbay A, Sevim S, et al. Surgical therapy versus observation for lamellar macular hole: a retrospective comparison study. Clin Ophthalmol. 2013; 7:1843–1848.


13. Panozzo G, Mercanti A. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol. 2004; 122:1455–1460.


14. Tanaka Y, Shimada N, Moriyama M, et al. Natural history of lamellar macular holes in highly myopic eyes. Am J Ophthalmol. 2011; 152:96–99.


15. Lin CW, Ho TC, Yang CM. The development and evolution of full thickness macular hole in highly myopic eyes. Eye (Lond). 2015; 29:388–396.



16. Lai TT, Chen SN, Yang CM. Epiretinal proliferation in lamellar macular holes and full-thickness macular holes: clinical and surgical findings. Graefes Arch Clin Exp Ophthalmol. 2016; 254:629–638.


17. Witkin AJ, Castro LC, Reichel E, et al. Anatomic and visual outcomes of vitrectomy for lamellar macular holes. Ophthalmic Surg Lasers Imaging. 2010; 41:418–424.


18. Gaucher D, Haouchine B, Tadayoni R, et al. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol. 2007; 143:455–462.


19. Alkabes M, Pichi F, Nucci P, et al. Anatomical and visual outcomes in high myopic macular hole (HM-MH) without retinal detachment: a review. Graefes Arch Clin Exp Ophthalmol. 2014; 252:191–199.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download