Abstract
Purpose
To evaluate the clinical features of intravitreal bevacizumab injection in patients with macular hemorrhage (submacular or subinternal limiting membrane hemorrhage) secondary to a retinal arterial macroaneurysm.
Methods
We retrospectively reviewed the medical records of 17 eyes of 17 patients who underwent intravitreal bevacizumab injection with macular hemorrhage secondary to retinal arterial macroaneurysm. We evaluated the improvement of visual acuity and changes in central retinal thickness after intravitreal injections of bevacizumab. According to the final visual acuity, the characteristics of the good and poor visual prognoses groups were compared.
Results
The mean age of patients (17 eyes) who underwent intravitreal bevacizumab treatment for macular hemorrhage secondary to retinal arterial macroaneurysm was 78.47 ± 7.84 years. The mean follow-up period was 3.99 ± 2.99 months, and the mean number of injections of bevacizumab was 2.12 ± 1.36. There were significant improvements in visual acuity and central retinal thickness, and the duration from symptom onset to treatment was shorter in patients with good visual prognoses.
Figures and Tables
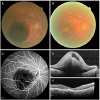 | Figure 1Images from the right eye of a 83-year-old woman with symptomatic retinal arterial macroaneurysm treated with intravitreal bevacizumab injections (patient 3). Initial visual acuity was hand motion. Duration from symptom onset to treatment was 10 days. (A, D) Fundus photograph and optical coherence tomography (OCT) obtained at the initial visit showing submacular and sub-inner limiting membrane hemorrhage with subretinal fluid secondary to the retinal arterial macroaneurysm. (C) Fluorescein angiography showing a focal hyperfluorescence attributable to macroaneurysm. (B, E) Fundus photograph and OCT 3 month after the 3 intravitreal bevacizumab injection showing resolution of the retinal hemorrhages, obliteration of the macroaneurysm, and flattened macular. Final best corrected visual acuity was 20/667 (Snellen). |
 | Figure 2Images from the left eye of a 88-year-old woman with symptomatic retinal arterial macroaneurysm treated with intravitreal bevacizumab injections (patient 11). Initial visual acuity was counting fingers. Duration from symptom onset to treatment was 3 days. (A, B) Fluorescein and indocyanine green angiography showing a focal hyperfluorescence attributable to macroaneurysm. (C, E) Fundus photograph and optical coherence tomography (OCT) obtained at the initial visit showing submacular and sub-inner limiting membrane hemorrhage secondary to the retinal arterial macroaneurysm. Initial visual acuty was counting fingers. (D, F) Fundus photograph and OCT 6 month after the 4 intravitreal bevacizumab injection showing resolution of the retinal hemorrhages, obliteration of the macroaneurysm, and flattened macular. Final best corrected visual acuity was 20/67 (Snellen). |
Table 1
Baseline characteristics of patient with the macular hemorrhage secondary to the retinal arterial macroaneurysm

Table 3
Comparison of two groups according to final best corrected visual acuity

Values are presented as mean ± standard deviation unless otherwise indicated. ‘Group A’ means good visual prognosis group. ‘Group B’means poor visual prognosis group.
M/F = male/female; RAM = retinal arterial macroaneurysm; BCVA = best corrected visual acuity; logMAR = the logarithm of the minimal angle of resolution; CRT = central retinal thickness.
*The significance of the difference was assessed by the Mann-Whitney U test; †The significance of the difference was assessed by the Fisher's exact test; ‡The significance of the difference was assessed by the linear by linear association.
References
1. Moosavi RA, Fong KC, Chopdar A. Retinal artery macroaneurysms: clinical and fluorescein angiographic features in 34 patients. Eye (Lond). 2006; 20:1011–1020.


2. Pitkänen L, Tommila P, Kaarniranta K, et al. Retinal arterial macroaneurysms. Acta Ophthalmol. 2014; 92:101–104.


3. Lavin MJ, Marsh RJ, Peart S, Rehman A. Retinal arterial macroaneurysms: a retrospective study of 40 patients. Br J Ophthalmol. 1987; 71:817–825.



4. Kim DH, Yu HG. Clinical results of vitrectomy in macular hemorrhage from a ruptured retinal artery macroaneurysm. J Korean Ophthalmol Soc. 2010; 51:961–966.

5. Moon SJ, Kim SW, Kim HS, et al. Intravitreal bevacizumab for macular edema secondary to ruptured retinal arterial macroaneurysm. J Korean Ophthalmol Soc. 2012; 53:522–527.

6. Ohno-Matsui K, Hayano M, Futagami S, et al. Spontaneous involution of a large retinal arterial macroaneurysm. Acta Ophthalmol Scand. 2000; 78:114–117.


7. Xu L, Wang Y, Jonas JB. Frequency of retinal macroaneurysms in adult Chinese: the Beijing Eye Study. Br J Ophthalmol. 2007; 91:840–841.



8. Brown DM, Sobol WM, Folk JC, Weingeist TA. Retinal arteriolar macroaneurysms: long-term visual outcome. Br J Ophthalmol. 1994; 78:534–538.



9. Tsujikawa A, Sakamoto A, Ota M, et al. Retinal structural changes associated with retinal arterial macroaneurysm examined with optical coherence tomography. Retina. 2009; 29:782–792.


10. Pichi F, Morara M, Torrazza C, et al. Intravitreal bevacizumab for macular complications from retinal arterial macroaneurysms. Am J Ophthalmol. 2013; 155:287–294.e1.


11. Battaglia Parodi M, Iacono P, Pierro L, et al. Subthreshold laser treatment versus threshold laser treatment for symptomatic retinal arterial macroaneurysm. Invest Ophthalmol Vis Sci. 2012; 53:1783–1786.


12. Parodi MB, Iacono P, Ravalico G, Bandello F. Subthreshold laser treatment for retinal arterial macroaneurysm. Br J Ophthalmol. 2011; 95:534–538.


13. Cho HJ, Rhee TK, Kim HS, et al. Intravitreal bevacizumab for symptomatic retinal arterial macroaneurysm. Am J Ophthalmol. 2013; 155:898–904.


14. Mansour AM, Foster RE, Gallego-Pinazo R, et al. Intravitreal anti-vascular endothelial growth factor injections for exudative retinal arterial macroaneurysms. Retina. 2018; 03. 02. DOI: 10.1097/IAE.0000000000002131. [Epub ahead of print].

15. Chanana B, Azad RV. Intravitreal bevacizumab for macular edema secondary to retinal macroaneurysm. Eye (Lond). 2009; 23:493–494.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download