Abstract
Tibialis anterior muscle herniation is the most common type of skeletal muscle herniation of the lower legs. The treatment of muscle herniation relies on the patient's symptoms. For patients with chronic large fascial defects, fascial grafting with synthetic mesh can be considered. In this case of a patient who was exposed to excessive strain on his lower legs during a military training program, the use of a secure repair technique with synthetic mesh was required. This paper presents a case of tibialis anterior muscle herniation that was treated successfully with a monofilament knitted polypropylene mesh covered by the tibialis anterior fascia. The advantages of this technique include early rehabilitation and an early return to work. No significant difference in the clinical results compared to other methods were observed and there were no complications. The military training program appeared to have aggravated the patient's symptoms of tibialis anterior muscle herniation. On the other hand, larger scale study will be needed to determine if this program actually affects the clinical outcomes.
Traumatic symptomatic herniation of the tibialis anterior muscle requires surgical treatment.1) Previously, several authors reported repairing fascial defects using mesh placed over the fascia to reduce the strain between the tibialis anterior muscle and the mesh.23) Here we present a case of tibialis anterior muscle herniation that was successfully treated with synthetic mesh that was beneath the fascia. Believing that the military training program likely worsened the symptoms of tibialis anterior muscle herniation, we designed the present study to investigate the correlation between the military training program and muscle herniation.
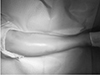
A 19-year-old male military recruit visited our outpatient clinic in Armed Forces Daejeon Hospital with vague pain and a palpable mass in the anterolateral aspect of the right lower leg. Four months prior, he suffered blunt trauma to the same area induced by a sharp metal fitness equipment. At that time, because the pain was feeble and there was no visible wound, he did not visit the hospital. However, as the military training program progressed, the palpable mass and vague pain developed and the size of the mass increased considerably. The mass also increased in size upon prolonged standing, squatting, or walking uphill. A physical examination revealed that the mass was located in the right lower leg along the lateral border in the middle of the tibia at 10 cm from the tibial tuberosity. The mass was prominent when the ankle joint was dorsiflexed (Fig. 1).
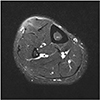
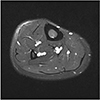
Based on history and clinical findings, we suspected that the mass was a tibialis anterior muscle herniation; magnetic resonance imaging (MRI) findings confirmed our suspicions. The MRI scans revealed a 3×5 cm oval-shaped focal herniation of the tibialis anterior muscle overlying a fascial defect. The margin of the fascial defect was thickened, and the muscle belly protruded through it (Fig. 2).
We attempted conservative treatments including lifestyle modification, compression stockings, and oral medications for a 1-month period. After conservative treatment failure, we provided surgical treatment. During surgery, we used a longitudinal skin incision overlying the mass to reveal a 3×5 cm fascial defect. The tibialis anterior muscle was bulging out through the fascial defect (Fig. 3).
Direct closure was not sufficient to repair the fascial defect because the margin was hypertrophied and it was difficult to approximate the margin without tension. Therefore, we applied fascial grafting using synthetic mesh placed under the fascia. We chose to cover the fascial defect with a monofilament knitted polypropylene mesh (Bard® mesh; C. R. Bard Inc., Warwick, RI, USA) (Fig. 4). The mesh was prepared to match the shape of the fascial defect (Fig. 5). Using an Army Navy retractor and Freer elevator, the protruded muscle belly was reduced. The mesh was placed under the fascia and the anterior margin of the fascia was initially repaired with a Prolene 4-0 monofilament. The posterior margin of the fascia was retracted with Allis tissue forceps to reduce the gap in the margin. The posterior margin was then repaired (Fig. 6). After a meticulous and secure repair was completed, friction and irritation between the mesh, suture knots, and the muscle were checked for during passive ankle movement.
After the surgery, we applied a short leg splint with the ankle in plantar flexion. Since a tight repair was performed, early rehabilitation was started. One week after surgery, we removed the splint and weight bearing was started. We recommended that the patient use compression stockings. Two weeks after surgery, full weight bearing was started. One month after surgery, the patient returned to work. At the 2-month follow-up, the patient returned to his normal sports activities. At the 6-month follow-up, there were no complications including irritation or cosmetic problems.
Skeletal muscle herniations are classified as constitutional or traumatic.45) Constitutional herniations are caused by chronic stress on the fascia of the underlying muscle, while traumatic defects are classified as those caused by direct or indirect trauma. In the present case, the blunt trauma to the right lower leg caused by a sharp metal fitness instrument may have contributed to the weakening of the fascia overlying the tibialis anterior muscle that led to the symptomatic muscle herniation later on.
Most cases to date have been described in athletes and young adults experiencing excessive strain on the lower legs.67) Due to being tight and superficial, the anterior tibial compartment is most commonly affected by muscle herniation. Therefore, here we investigated whether the military training program and excessive strain on the lower legs were correlated. We found that the military training program could have worsened the symptoms of tibialis anterior muscle herniation. These results confirm those of a previous study8) in which the primary strength of military-related physical activities was shown to be derived more from the lower extremities than from the upper extremities. The weight-based training program is used to strengthen the lower extremities, while the calisthenics program trains the leg and hip muscles. Furthermore, working as a sentry who maintains a standing position for a long time can be a factor of the acquired excessive strain on the lower legs.
Since treatment relies mainly on patient symptoms, asymptomatic muscle herniation requires no specific treatment. Symptomatic muscle herniation has various treatments ranging from conservative management to surgical procedures including direct repair, fasciotomy, and fascial grafting using an autologous graft or synthetic mesh. For patients with chronic and large fascial defects, fascial grafting with an autologous graft or synthetic mesh can be considered. Fascial grafting using an autologous graft such as a tensor fascia lata9) or periosteal graft10) can be useful. There are several advantages to this, such as a lack of skin irritation and low cost. However, this procedure requires careful postoperative observation for compartment syndrome and donor site morbidity. Considering the patient's concern about the cosmetic result of the surgery and secondary damage that would occur at the donor site, an autologous graft was not considered.
In this case, the patient was exposed to excessive strain on the lower legs during the military training program and his work as a sentry. This meant that he maintained a long-term standing position of more than 4 hours a day. He wanted to achieve early recovery and an early return to work. Therefore, secure surgical repair with synthetic mesh was required. Some authors previously suggested that the mesh should be fixed above rather than under because it allows the underlying muscle to slide without any friction by the mesh or suture materials.23) However, the fascial defect margin was hypertrophied and thickened in this case, and we were concerned that the bulky margin could interrupt the tight repair and cause skin irritation. Thus, we decided to fix the mesh beneath the fascia. After fixation, we checked the grafting site during passive ankle movement. There was no irritation around the mesh or suture materials and the underlying muscle was sliding without any interruption. There were no abnormal findings on the immediate postoperative and 3-month follow-up MRI scans (Fig. 7). Since a tight repair was performed, early rehabilitation was started and an early return to work enabled. To the best of our knowledge, this is the first case report to focus on South Korean military recruits. Although only one case was described in this report and the follow-up period was short, fascial grafting using synthetic mesh provided satisfactory outcomes without serious complications and could be an alternative option to conventional surgical treatments.
In conclusion, tibialis anterior muscle herniations should be considered a rare differential diagnosis whenever patients present with persistent vague leg pain after a military training program. Furthermore, in cases of chronic and large fascial defects, fascial grafting using synthetic mesh under the fascia can be a good option for managing tibialis anterior muscle herniation, as this simple procedure can provide good functional outcomes without complications.
Figures and Tables
References
1. Miniaci A, Rorabeck CH. Tibialis anterior muscle hernia: a rationale for treatment. Can J Surg. 1987; 30:79–80.

2. Siliprandi L, Martini G, Chiarelli A, Mazzoleni F. Surgical repair of an anterior tibialis muscle hernia with Mersilene mesh. Plast Reconstr Surg. 1993; 91:154–157.


3. Marques A, Brenda E, Amarante MT. Bilateral multiple muscle hernias of the leg repaired with Marlex mesh. Br J Plast Surg. 1994; 47:444–446.


4. Nguyen JT, Nguyen JL, Wheatley MJ, Nguyen TA. Muscle hernias of the leg: a case report and comprehensive review of the literature. Can J Plast Surg. 2013; 21:243–247.



5. Ihde H. On muscular hernia of the leg. Acta Chir Scand. 1929; 65:97–120.
6. Kim M, Hong SP, Hwang SM, Park H, Ahn SK. Tibialis anterior muscle herniation developed after trauma. Int J Dermatol. 2008; 47:845–847.


7. Rho NK, Kim WS, Kim YJ, Yoo KH, Kim BJ, Kim MN. The use of dynamic ultrasonography for the confirmation of lower leg muscle herniation. Ann Dermatol. 2008; 20:190–192.



8. Harman EA, Gutekunst DJ, Frykman PN, et al. Effects of two different eight-week training programs on military physical performance. J Strength Cond Res. 2008; 22:524–534.


9. Simon HE, Sacchet HA. Muscle hernias of the leg: review of literature and report of twelve cases. Am J Surg. 1945; 67:87–97.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download