Abstract
Background and Purpose
Although the 15-item Geriatric Depression Scale (GDS15) is a widely used depression screening questionnaire, the implications of the GDS15 in patients with Alzheimer's disease (AD) are questionable. We designed this study to explore the GDS15 factor structure and the relationships between these factors and cognitive-behavioral aspects.
Methods
The GDS15, cognitive function tests, and the Korean-Neuropsychiatry Inventory were administered to 310 patients with probable AD, who were not medicated before visiting the hospital. Three factors were identified by principal components analysis. A bivariate correlation analysis was conducted to determine the relationships between factors and neurocognitive and behavior symptoms.
Results
Factor 2 was correlated with the Korean Boston Naming Test, calculating ability, the go-no-go test, the Controlled Oral Word Association Test (COWAT), the Color Word Stroop Test (CWST; words and color), aggression, depression, and apathy. Factor 3 was correlated with calculating ability, the Seoul Verbal Learning Test, immediate recall, copy, and delayed recall on the Rey-Osterieth Complex Figure Test, contrasting on the COWAT, and words and delusion on the CWST. We identified three factors and revealed that the GDS15 may be comprised of a heterogeneous scale.
The Geriatric Depression Scale (GDS) is a widely used clinical and research depression screening tool since it was first developed over 30 years ago.1 This is the first specifically designed depression screening scale for elderly persons, as somatic and sexual complaints that are present on other depression scales have been removed. However, because the original GDS (GDS30) is relatively time-consuming, a shortened 15-item version (GDS15), which was extracted from the GDS30, has been developed.2 Sensitivity and specificity of the GDS15 has been assessed in a general elderly population,2 geriatric inpatients,3 primary care outpatients,4,5 and elderly patients6 and shows good discriminant validity, content validity, concurrent validity and internal consistency and reliability.
The GDS is a reliable screening tool for detecting depressive symptoms in elderly persons and patients with mild cognitive impairment. However, the usefulness of the GDS for patients with dementia, such as Alzheimer's disease (AD), is questionable.7,8 Thus, exploring the structure and clinical characteristics of the GDS15 items would be helpful to determine the utility of the GDS15 in patients with AD.
One approach to better understand the GDS15 and depressive symptomatology of patients with AD is to evaluate whether specific GDS15 items are associated with patients with AD. Rather than recognizing individual items separately, a number of associated items (factors) are identified and compared with these factors. This approach can provide insight into how the GDS15 items can be subgrouped (factors) and whether the GDS can be used as a uni-dimensional (i.e., a total score measuring depression)9 or multi-dimensional scale (i.e., grouping different subscales together into one total score).10,11 If the individual items of the GDS are heterogeneous in patients with AD, then they might be grouped similarly; thus, allowing delineation of more homogenous sub-groups and provide insight into depression in patients with AD. A factor analysis is the most widely used statistical method to extract correlated subsets of the GDS items, and a few factor analyses of the GDS309,10,11,12 and GDS1513,14,15,16,17 have been published.
The cognitive implications of depression in patients with AD have been studied extensively with inconsistent results. Previous studies provide evidence for a negative impact of depression on domains, including general cognition,18 full scale IQ,19 measures of dementia severity, working memory, processing speed,20 attention, motor functioning, and visuospatial perception and construction.21 Other investigators have found no cognitive differences between patients with AD with and without depressive symptoms.22,23
One of the confounding factors in this inconsistency is a psychoactive medication effect, particularly that of antidepressants. Depression is clearly influenced by antidepressants, but it can also be influenced by other psychoactive medications. Due to the long-standing Korean Confucian tradition of caring for patients with dementia by family members, a considerable portion of patients with mild to severe AD visit dementia clinics with no medication history. Therefore, we are able to recruit for drug-naïve patients with probable AD, which would overcome the psychoactive medication effects.
The aims of this study were to examine the factor structure of the GDS15 in patients with probable AD. A second aim was to identify the relationships between these factors and neuropsychological and behavioral aspects. Finally, we determined the structure and clinical meaning of the GDS15.
The initial 1324 patients with dementia were prospectively enrolled and screened from March 2003 to July 2013 at the Hyoja Geriatric Hospital. Among the 1324 patients, the study subjects included 310 patients with probable AD, who were not medicated before visiting the hospital. All study subjects met the National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer's Disease and Related Disorders Association criteria for probable AD.24 Patients who were taking psychoactive drugs, including antidepressants, antipsychotics, anticonvulsants, benzodiazepines, or cholinesterase inhibitors were excluded from this study.
All study subjects underwent a complete medical history, physical and neurological evaluations, comprehensive neuropsychological testing, routine laboratory tests, and brain magnetic resonance imaging or a computed tomography scan.
A structured interview and neuropsychological examination were performed with each subject. The Korean version of the Mini-Mental State Examination (K-MMSE)25 and the Clinical Dementia Rating Scale (CDR)26 were used to assess cognitive function. The Barthel index27 was used to assess activities of daily living (ADL).
Cognitive functions of all study subjects were evaluated with the Seoul Neuropsychological Screening Battery,28 which includes standardized and validated tests of diverse cognitive domains. Among them, the forward digit span, the Korean version of the Boston Naming Test, calculation, the Seoul Verbal Learning Test (SVLT) (three immediate recall trials of 12 items and 20-min delayed recall trial for the 12 items), the Rey-Osterrieth Complex Figure Test (RCFT) (copying, immediate, and 20-min delayed recall and recognition), the Controlled Oral Word Association Test (COWAT), which is test of semantic fluency and letter-phonemic fluency and contrasting program test, the go-no-go test, and the Color Word Stroop Test (CWST) were adopted for this study.
The GDS15 was administered by a trained neuropsychologist. A cutoff screening criterion of the Korean version of GDS15 for depression is 8 or more endorsed items.5 This would mean that a participant answered yes in the case of the 10 negative items and no in the case of the five positive items.
The Korean version of the Neuropsychiatry Inventory (K-NPI)29 was administered to assess the behavioral aspects of dementia. This scale addresses 12 specific behavioral and psychological symptoms and provides a numeric score for each domain that is the product of the frequency by severity sub-scores. The total K-NPI score was calculated by adding the 12 composite scores. Diagnosing depression based on the Neuropsychiatry Inventory (NPI) depression domain was classified as the NPI-D (>1 on the depression subscale).
After a complete description of the study was given to the patients and their caregivers, written informed consent was obtained from all patients or caregivers.
The study subject demographic data are described, and an estimate of internal consistency of the GDS15 as a function of dementia severity was made. A principal components analysis (PCA) was carried on the GDS15. Before the PCA analysis, two complementary methods, the Kaiser-Meyer-Olkin Measure of Sampling Adequacy and Bartlett's test of sphericity, were used to assess the appropriateness of a factor analysis. The objective of this preliminary phase was to assess whether items were reciprocally related to develop a factor model. Factors were extracted by using PCA with Spearman's correlation matrices, and varimax rotation was used for orthogonal rotation to achi-eve a simple structure. The rotation phase allows for the identification of factors summarizing sets of closely related variables and is more easily interpreted than those obtained in the extraction phase. Factors were selected if their eigenvalue was 1, and an item was included if its factor loading was 0.30. Factors were extracted initially by PCA for mathematical and empirical determination of the factors. Spearman's correlation analysis was conducted between the GDS15 items and cognitive functions, ADL, and behavioral symptoms to identify the characteristics of these GDS15 subgroups. Statistical analyses were performed with the SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). A p-value <0.05 was considered significant.
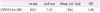
The study included 124 men (40.0%) and 186 women (60.0%) with a mean age of 74.6±7.5 years. The mean K-MMSE and CDR scores were 19.0±5.6 and 1.1±0.6 respectively, indicating that subjects with mild to moderate AD were mainly recruited (Table 1). More than half of the subjects had depression, according to self-rated criteria (GDS15) and caregiver-rated criteria (NPI-D), and 26.3% of the subjects had depression based on the GDS15 without evidence of depression on the NPI-D (Table 1).
Internal reliability was measured using Cronbach's alpha and is presented in Table 2 according to dementia severity. The internal consistency of the GDS15 was excellent across all three groups and did not decline with dementia severity (Table 2).
Test-retest reliability was evaluated with a 1 week interval using patients with AD not included in this study. Reliability was evaluated with the intraclass coefficient, and good reliability was demonstrated (Table 3).
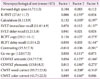
The prevalence of individual GDS15 items is summarized in Table 4. Item 8, "often feel helpless" was the most frequently endorsed item and item 11, "wonderful to be alive now (no)" was the least frequently endorsed item.
The PCA results and the factor loadings are shown in Table 4. All 15 items reached the factor loading criterion of ≥0.30, and three subgroups were identified using the 15 items. These three subgroups explained 52.25% of the total data variance.
The first subgroup, factor 1 (resembling what was previously called "dysphoria"12,13,20) (29.98% of total variance) included eight items: "feel pretty worthless", "feel your life is empty", "often feel helpless", "often get bored", "feel your situation is hopeless", "prefer to stay at home", "afraid something bad will happen", and "most people better off". The second subgroup, factor 2 (resembling what was previously called "life satisfaction or apathy"12,13,20) (12.07% of total variance) was comprised of four items: "in good spirits most of the time (no)", "hopeful about the future (no)", "wonderful to be alive now (no)", and "basically satisfied with life (no)". The third subgroup, factor 3 (resembling what was previously called "cognitive impairment"13,20) (10.50% of total variance) included three items: "have more memory problems than most", "dropped many activities and interests", and "feel full of energy (no)".
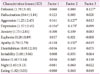
The correlation between the GDS15 factors and general cognitive and ADL functions are summarized in Table 5. In contrast to factors 1 and 3, factor 2 was not significantly correlated with GDS15. The Barthel index was significantly correlated with factor 1 and negatively correlated with factor 2. The MMSE was significantly correlated with factors 2 and 3.
Factor 2 was significantly correlated with the Korean Boston Naming Test (K-BNT), calculation, go-no-go, the COWAT (semantic and phonemic), and the CWST (word and color). Factor 3 was correlated with calculation, the SVLT (immediate recall), RCFT (copy delay recall, and contrasting), the COWAT (semantic and phonemic), and the CWST (word). Factor 1 was not correlated with any of the tested neurocognitive functions (Table 6).
Factor 2 was significantly correlated with aggression, depression, and apathy. Factor 3 was correlated with delusion. Factor 1 was correlated with the depression subdomains in the K-NPI (Table 7).
Depression in patients with AD has different clinical features than those occurring in younger non-demented patients. Due to these differences, depression in patients with AD has been considered an atypical syndrome of depression.11 How cognitive dysfunction is associated with depression is unclear in patients with AD, and there is no consensus. Due to this lack of consistent relationships between cognitive abnormalities and depression,30 depression is usually regarded as an epiphenomenon of AD and not secondary to cognitive impairment.31 Depression has also been associated with greater impairment in ADL, behavioral disturbances, such as aggression and wandering,32 and psychoses, such as delusions and hallucinations.33
The GDS is a widely used clinical and research instrument, but its clinical utility in patients with dementia is questionable. Items related to cognitive aspects in the GDS, which is a useful depression index in younger patients, usually accompany patients with AD. These cognitive impairment items can influence overall GDS scores according to dementia severity.
Several studies have reported the factor structure of the GDS and have extracted similar components. First, there is a consistent dysphoria or similar mood component.11,13 There is also frequently a component that suggests symptoms of apathy or symptoms related to apathy (e.g., diminished motivation or social withdrawal).13,16 Several studies have also reported components related to cognitive impairment and anxiety.10,11 However, the subjects of these studies were samples of cognitively intact or heterogeneously impaired subjects, whereas study subjects were homogenous with probable AD. Thus, these studies may not be appropriately applied to patients with probable AD.
We presented a three-factor PCA model that shows good overall fit using the GDS15. The reliability analyses support internal consistency of the GDS15 in patients with different severity levels of dementia, including those with severe cognitive impairment.
As in previous studies, the results of our factor analysis yielded three factors reflecting dysphoria,11,14 life satisfaction,13,16 and cognitive impairment.11 Factor 1 consisted of eight items that describe worthlessness, emptiness, helplessness, boredom, and hopelessness, as well as getting bored and fear that something bad is going to happen. All of these questions are positively stated items. Factor 2 consisted of four items considering lack of good spirits, not hopeful about the future, not wonderful to be alive, and a lack satisfaction with life. All of these items are comprised of negatively stated beliefs. Factor 3 was comprised of three items that describe memory problems, decreased activities, and lack of energy. A mix of positively and negatively stated items occurred in factor 3.
An analysis of item frequencies revealed that "helpless" was most the frequently endorsed item and that "wonderful to be alive now" was the least frequently endorsed item. In a previous factor analysis study on the GDS15,13 three dimensions were reported, such as general depressive affect (resembling our factor 1), life satisfaction (resembling our factor 2), and withdrawal (resembling our factor 3). In our study, the item "do you feel you have more problems with memory than most?" did not load highly on the cognitive impairment construct, but this item loaded highly on factor 3. The item "prefer to stay at home" is included in withdrawal symptoms, but this was included in factor 1 in our study. The item "dropped activity and interest" is included in withdrawal or apathy symptoms,11,17 but this item was a component of factor 3 in our study.
Another AD study that used the GDS30 reported four factors. All items included in factor 2 of our study belong to the apathy factor. Most items in factor 1 of our study were consistent with dysphoric factors, except items 3 (apathy factor) and 9 (social withdrawal factor). Only the memory problem items in factor 3 of our study were consistent with cognitive impairment factors. The item "dropped activity" (factor 3 in our study) is included as an apathy factor and the item "prefer to stay home" (cognitive impairment item in our study) is included as a social withdrawal factor.18 These discrepancies may be due to differences in study subject characteristics, e.g., community study or hospital study, and non-demented or patients with AD.
The correlations between these factors and cognitive functions, ADL, and the neuropsychiatric symptom domains were analyzed to identify the clinical characteristics of these factors. Interestingly, factor 1 was not correlated with any other general, specific cognitive function and was only correlated with the depression subdomain of the K-NPI. However, this factor was correlated with the Barthel index, which was rather puzzling. Considering that this factor was not correlated with a cognition index (K-MMSE or CDR), factor 1 may have mild dementia severity. This hypothesis should be explored.
Factor 2 was significantly correlated with the K-MMSE, the Barthel index, the K-BNT, calculation, go-no-go test, the COWAT (semantic and phonemic), the CWST (word and color), and the aggression, depression, and apathy tests. Factor 3 was correlated with the K-MMSE, the CDR, calculation, the SVLT (immediate recall), the RCFT (copy, delay recall, and contrasting), the COWAT (semantic and phonemic), the CWST (word), and delusions. These findings suggest that factors 2 and 3 are more or less related to diverse cognitive functions and behavioral symptoms, whereas factor 1 was not associated with any cognitive aspects. Thus, our results may favor the cognitive bias hypothesis of depression.
The depression subdomain of the K-NPI was correlated with factors 1 and 2. Apathy in the K-NPI was only correlated with factor 2. These findings suggest that depression, as measured by the K-NPI, usually reflects life satisfaction (or apathy?) and cognitive aspects, but not subjective-rated dysphoric aspects. This discrepancy between the GDS15 and the K-NPI was suggested previously.34
Another possibility that cannot be overlooked relates to the valence of the factor 2 items, which can be related to the construct of the items or that the structure of the questionnaire influenced the results, considering that the items for this factor were all negatively associated. For example, "do you feel happy most of the time?" and the negatively stated item "don't you feel happy most of the time?" may affect the underlying factor structure of the items. Patients should hold their responses to a go stimulus but respond to a no-go stimulus, if they are responding appropriately. This response inhibition is a condition sine qua non for human executive function, and diverse cognitive functions, including response inhibition, should be mobilized.35 The go-no-go test can assess these functions. Thus, the correlations between factor 2 and the negatively stated items may be associated with the structure of this questionnaire.
Our results show that some questionnaire items are more likely to be associated with general and specific cognitive functions. As a result, these items can be non-affective factors, even though they are found in depression scales, such as the GDS. However, we should be cautious when interpreting the clinical implications of these factors, particularly between factors 2 and 3. Further studies are needed to elucidate the somewhat different neuropsychological impairment profiles suggested for involvement of different neural substrates.
In contrast to previous studies that only determined the GDS structure, we revealed not only the structure, but the cognitive-behavioral characteristics of these factors. By associating the factors with other cognitive and behavioral aspects, we gained insight in to GDS structure for patients with AD. However, whether depression influenced cognitive function or vice versa remains uncertain because of the study design and statistical methods.
Our study had several limitations. First, sample size was relatively small. Second, we included mainly patients with mild AD; thus, this study was biased for mild cases (mean CDR score, 1.1). Third, the statistical methods (correlation) and study design (retrospective study) cannot be used to determine cause-effect relationships and only suggest correlations among factors. Thus, we cannot define the flow relationship among these variables. Fourth, correlation testing is used to confirm the relationship between two variables. Although the result is significant with a p-value <0.05, the correlation coefficients of some variables that measure the strength and direction of the relationship between two variables was low in our study. Thus, although these variables were related, the strength (not the relationship itself) may have been low. The statistical results should be considered cautiously. Finally, this was a hospital-based study and may not represent the actual community.
In summary, our results show that the GDS15 was comprised of three different structures, and these factors were related to cognitive and behavioral symptoms. These findings suggest multi-dimensional characteristics of the GDS in patients with AD. Therefore, a screening tool for depression should be applied cautiously.
Figures and Tables
References
1. Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983; 17:37–49.

2. Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS) recent evidence and development of a shorter version. Clinical Gerontologist. 1986; 1:165–173.

3. Shah AK, Phongsathorn V, Bielawska C, Katona C. Screening for depression among geriatric inpatients with short versions of the Geriatric Depression Scale. Int J Geriatr Psychiatry. 1996; 11:915–918.

4. D'Ath P, Katona P, Mullan E, Evans S, Katona C. Screening, detection and management of depression in elderly primary care attenders. I: The acceptability and performance of the 15 item Geriatric Depression Scale (GDS15) and the development of short versions. Fam Pract. 1994; 11:260–266.

5. Bae JN, Cho MJ. Development of the Korean version of the Geriatric Depression Scale and its short form among elderly psychiatric patients. J Psychosom Res. 2004; 57:297–305.

6. Pomeroy IM, Clark CR, Philp I. The effectiveness of very short scales for depression screening in elderly medical patients. Int J Geriatr Psychiatry. 2001; 16:321–326.

7. Montorio I, Izal M. The Geriatric Depression Scale: a review of its development and utility. Int Psychogeriatr. 1996; 8:103–112.

8. Debruyne H, Van Buggenhout M, Le Bastard N, Aries M, Audenaert K, De Deyn PP, et al. Is the geriatric depression scale a reliable screening tool for depressive symptoms in elderly patients with cognitive impairment? Int J Geriatr Psychiatry. 2009; 24:556–562.

9. Parmelee PA, Lawton MP, Katz IR. Psychometric properties of the Geriatric Depression Scale among the institutionalized aged. Psychol Assess. 1989; 1:331–338.

10. Adams KB, Matto HC, Sanders S. Confirmatory factor analysis of the geriatric depression scale. Gerontologist. 2004; 44:818–826.

11. Adams KB. Depressive symptoms, depletion, or developmental change? Withdrawal, apathy, and lack of vigor in the Geriatric Depression Scale. Gerontologist. 2001; 41:768–777.

12. Sheikh JI, Yesavage JA, Brooks JO 3rd, Friedman L, Gratzinger P, Hill RD, et al. Proposed factor structure of the Geriatric Depression Scale. Int Psychogeriatr. 1991; 3:23–28.

13. Mitchell J, Mathews HF, Yesavage JA. A multidimensional examination of depression among the elderly. Research on Aging. 1993; 15:198–219.

14. Friedman B, Heisel MJ, Delavan RL. Psychometric properties of the 15-item geriatric depression scale in functionally impaired, cognitively intact, community-dwelling elderly primary care patients. J Am Geriatr Soc. 2005; 53:1570–1576.
15. Incalzi RA, Cesari M, Pedone C, Carbonin PU. Construct validity of the 15-item geriatric depression scale in older medical inpatients. J Geriatr Psychiatry Neurol. 2003; 16:23–28.
16. Brown PJ, Woods CM, Storandt M. Model stability of the 15-item Geriatric Depression Scale across cognitive impairment and severe depression. Psychol Aging. 2007; 22:372–379.

17. Havins WN, Massman PJ, Doody R. Factor structure of the Geriatric Depression Scale and relationships with cognition and function in Alzheimer's disease. Dement Geriatr Cogn Disord. 2012; 34:360–372.

18. Rovner BW, Broadhead J, Spencer M, Carson K, Folstein MF. Depression and Alzheimer's disease. Am J Psychiatry. 1989; 146:350–353.
19. Breen AR, Larson EB, Reifler BV, Vitaliano PP, Lawrence GL. Cognitive performance and functional competence in coexisting dementia and depression. J Am Geriatr Soc. 1984; 32:132–137.
20. Rubin EH, Kinscherf DA, Grant EA, Storandt M. The influence of major depression on clinical and psychometric assessment of senile dementia of the Alzheimer type. Am J Psychiatry. 1991; 148:1164–1171.
21. Wefel JS, Hoyt BD, Massma PJ. Neuropsychological functioning in depressed versus nondepressed participants with Alzheimer's disease. Clin Neuropsychol. 1999; 13:249–257.
22. Fahlander K, Berger AK, Bäckman L, Wahlin A. Depression does not aggravate the episodic memory deficits associated with Alzheimer's disease. Neuropsychology. 1999; 13:532–538.

23. Lopez OL, Boller F, Becker JT, Miller M, Reynolds CF 3rd. Alzheimer's disease and depression: neuropsychological impairment and progression of the illness. Am J Psychiatry. 1990; 147:855–860.

24. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984; 34:939–944.

25. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997; 15:300–308.

26. Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982; 140:566–572.

27. Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J. 1965; 14:61–65.

28. Kang Y, Na D. Seoul Neuropsychological Screening Battery (SNSB). Incheon: Human Brain Research & Consulting;2003.

29. Choi SH, Na DL, Kwon HM, Yoon SJ, Jeong JH, Ha CK. The Korean version of the neuropsychiatric inventory: a scoring tool for neuropsychiatric disturbance in dementia patients. J Korean Med Sci. 2000; 15:609–615.

30. Lyketsos CG, Steinberg M, Tschanz JT, Norton MC, Steffens DC, Breitner JC. Mental and behavioral disturbances in dementia: findings from the Cache County Study on Memory in Aging. Am J Psychiatry. 2000; 157:708–714.

31. Payne JL, Lyketsos CG, Steele C, Baker L, Galik E, Kopunek S, et al. Relationship of cognitive and functional impairment to depressive features in Alzheimer's disease and other dementias. J Neuropsychiatry Clin Neurosci. 1998; 10:440–447.

32. Schneider LS, Tariot PN, Lyketsos CG, Dagerman KS, Davis KL, Davis S, et al. National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE): Alzheimer disease trial methodology. Am J Geriatr Psychiatry. 2001; 9:346–360.

33. Zubenko GS, Zubenko WN, McPherson S, Spoor E, Marin DB, Farlow MR, et al. A collaborative study of the emergence and clinical features of the major depressive syndrome of Alzheimer's disease. Am J Psychiatry. 2003; 160:857–866.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download