Abstract
Background
Anti-N-methyl-D-aspartate (anti-NMDA) receptor encephalitis was discovered less than 10 years ago. Its symptoms and characteristics are not well-defined yet. We experienced a case of anti-NMDA receptor encephalitis with phonemic paraphasia and acalculia that were not classical characteristics.
Case Report
A 44-year-old woman started to show dyslexia, phonemic paraphasia, and dyscalculia. These symptoms were gradually worsening for over 30 days. Various brain images were not helpful for primary diagnosis. Anti-NMDA receptor encephalitis was confirmed in two different laboratories. The patient started to recover with various immunosuppressive therapies.
The most common etiology of encephalitis is infection. However, immune-mediated etiologies of encephalitis are now increasingly recognized. Anti-N-methyl-D-aspartate (NMDA) receptor encephalitis was first identified in 2007 by Dalmau and Bataller.1 Its characteristics include impaired consciousness, psychosis, seizures, dyskinesia, autonomic instability, and other various symptoms.2 Among these symptoms, rapid progressive psychosis is the first symptom of the disease in most cases. We experienced a case of anti-NMDA receptor encephalitis with phonemic paraphasia and acalculia as first symptoms that were not classical characteristics.
A 44-year-old woman presented with dyslexia. She was unmarried without relevant medical or family history of epilepsy or stroke. She was a mathematical teacher in a school. She felt the first symptom during a class. She could not read the textbook fluently or perform even a simple calculation. The symptom was not severe at the first time. It did not significantly affect here everyday life. However, here symptoms showed gradual progression within 2 weeks. She started to have problem recognizing Korean letters. She had a hard time finding the right words for objects that she could recognize. In addition, she could not teach students anymore because she couldn't recall appropriate words during a conversation.
At 4 weeks after showing the first symptom, she presented to a nearest emergency department. Her initial vital signs were stable. The patient was alert. She showed good cooperation. She was able to follow the 3 step instruction. Her orientation was intact for time, place, and person. Her cranial nerve exam and motor sensory exams didn't have any deficit. However, she had impaired language function with fragmented fluency. She had difficulties in finding words. She could not perform any simple calculation appropriately. Her symptoms were dyslexia, phonemic paraphasia, and dyscalculia. These symptoms were thought as subacute, suggesting vascular stroke including Gerstmann syndrome or rapid progressive dementia such as Creutzfelt Jakob disease (CJD). Brain images were obtained to explore the etiology of her symptoms. Gradient echo MRI demonstrated no diffusion restriction lesions. In addition, brain magnetic resonance image (MRI) and angiography showed no parenchymal lesion or vessel abnormality. Cerebrospinal fluid (CSF) analysis failed to show any abnormal findings such as pleocytosis or protein level. Her initial Korean-Mini Mental State Examination (K-MMSE) score was 22. She was diagnosed as mild cognitive dysfunction. She was given oral antiplatelet agent and donepezil for 14-3-3 protein to differentiate CJD. After discharge, she showed depression, irritability, and night time visual hallucination. After 5 days, she couldn't make any conversation. She had abnormal phonation.
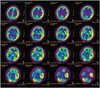
She was admitted to the Neurology Department at Korea University Anam Hospital. Her language function showed global aphasia. Follow up K-MMSE was uncheckable. Follow up brain MRI showed slightly high signal intensity on the left hippocampus (Fig. 1). Brain single-photon emission computed tomography (SPECT) (Tc-99m) showed relatively hyper-perfusion of the left temporal cortex than the right side (Fig. 2). Electroencephalogram showed continuous delta slow activity in the left hemisphere with delta brush pattern that could be seen in NMDA receptor encephalitis (Fig. 3). Repeated CSF analysis showed normal white blood cell count and protein levels. Although most studies could not define a specific diagnosis so far, the patient's clinical symptoms such as progressive psychosis, irritability, and bizzare arm movements suggested an anti-NMDA receptor encephalitis. Therefore, we sent her CSF samples to Seoul National University Hospital and Josep Dalmau Laboratory in Spain to test for autoimmune antibodies. Results were positive for NMDA receptor antibodies in both laboratories. We diagnosed her as anti-NMDA receptor encephalitis. We treated her with corticosteroids for 5 days, intravenous immunoglobulin for 5 days consecutively, and rituximab therapy for 3 cycles in a 30 day period with 1 more cycle after 6 months. She was also maintained with daily prednisolone at 15 mg. She was improved gradually after discharge. At 6 months later, she was able to come back to teach students with minor language difficulties that only she could feel. When anti-NMDA receptor antibodies were confirmed, she underwent additional tests to check for ovarian teratoma that is highly associated with anti-NMDA receptor antibodies. However, abdomen and pelvis CT, gynecologic sonography, and tumor marker tests through serum blood all failed to show any abnormal finding. Later, the patient provided more previous history with similar symptoms about 20 years ago. At that time, she suddenly showed violent behavior with reduced lingual expression. A psychiatrist suspected schizophrenia and gave her antipsychotics for 1 year. Her symptoms were resolved completely after that time without any deficit.
The characteristics of anti-NMDA receptor encephalitis are still not well-defined yet.234 Its first clinical symptoms could be so different that it is hard to differentiate appropriate diagnosis in neurology. It could be misdiagnosed as mild cognitive impairment, rapid progressive dementia, depression, or other psychologic disorders. A relatively small number of cases have reported that language dysfunction and calculation problem are first presenting symptoms.5 In this case, we found the following three atypical findings compared to typical anti-NMDA receptor encephalitis characteristics defined up to date. First, the patient showed dyslexia, phonemic paraphasia, and dyscalculia as first symptoms with progression. Considering these symptoms, we expected the lesion to be at the Broca's area that could develop motor aphasia. However, initial brain MRI showed no lesion. Follow up MRI after 4 weeks only showed suspicious signal change in the left hippocampal area. It is known that anti-NMDA receptor encephalitis may affect the brain asymmetrically. It may show structural lesions such as leptomeningeal enhancement and subcortical signal change.678 However, in this case, brain imaging was unhelpful, including brain CT. Electroencephalogram (EEG) and brain SPECT provided dysfunction in the left hemisphere. However, extreme delta brush pattern in EEG (Fig. 3B) could be a meaningful sign of anti-NMDA receptor encephalitis.910 Second, the patient never had any headache, fever, or viral-like illness throughout the clinical course, although these symptoms are classic features of encephalitis. According to some review articles, about 48–86% of anti-NMDA encephalitis patients have those symptoms weeks prior to acute presentation.211 In addition, CSF white blood cells and protein levels in anti-NMDA receptor encephalitis patients may not be reliable.12 Therefore, it is important to suspect anti-NMDA receptor encephalitis even when there is no classic characteristics of encephalitis. Third, the patient didn't have ovarian teratoma or other reproducing organ problem. The relationship between anti-NMDA receptor encephalitis and ovarian teratoma is well known. When teratoma is present, surgical treatment should be considered.213
In summary, anti-NMDA receptor encephalitis has been discovered for less than 10 years1 without well-defined characteristics.2 Therefore, many people with early cognitive and language dysfunction with subacute progression should be considered as anti-NMDA receptor encephalitis even though the classic symptoms of encephalitis are absent. Because anti-NMDA receptor encephalitis is treatable and reversible,2 we need to note its various possible symptoms so that appropriate treatment will not be delayed.
Figures and Tables
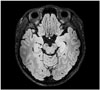 | Fig. 1MRI FLAIR image showing slightly high signal intensity on the left hippocampus (head to tail). FLAIR: fluid-attenuated inversion recovery, MRI: magnetic resonance image. |
References
1. Dalmau J, Bataller L. [Limbic encephalitis: the new cell membrane antigens and a proposal of clinical-immunological classification with therapeutic implications]. Neurologia. 2007; 22:526–537.

2. Barry H, Byrne S, Barrett E, Murphy KC, Cotter DR. Anti-N-methyl-d-aspartate receptor encephalitis: review of clinical presentation, diagnosis and treatment. BJPsych Bull. 2015; 39:19–23.

3. Wang W, Li JM, Hu FY, Wang R, Hong Z, He L, et al. Anti-NMDA receptor encephalitis: clinical characteristics, predictors of outcome and the knowledge gap in southwest China. Eur J Neurol. 2015; 11. 12. DOI: 10.1111/ene.12911. [Epub].

4. Pollak TA, McCormack R, Peakman M, Nicholson TR, David AS. Prevalence of anti-N-methyl-D-aspartate (NMDA) receptor [corrected] antibodies in patients with schizophrenia and related psychoses: a systematic review and meta-analysis. Psychol Med. 2014; 44:2475–2487.

5. Deiva K, Pera MC, Maurey H, Chrétien P, Archambaud F, Bouilleret V, et al. Sudden and isolated Broca's aphasia: a new clinical phenotype of anti NMDA receptor antibodies encephalitis in children. Eur J Paediatr Neurol. 2014; 18:790–792.

6. Reid DK, Clardy SL. Neurological picture. Anti-NMDA-receptor encephalitis: unusual presentation of an uncommon condition. J Neurol Neurosurg Psychiatry. 2013; 84:69–70.

7. Hacohen Y, Absoud M, Hemingway C, Jacobson L, Lin JP, Pike M, et al. NMDA receptor antibodies associated with distinct white matter syndromes. Neurol Neuroimmunol Neuroinflamm. 2014; 1:e2.

8. Finke C, Kopp UA, Pajkert A, Behrens JR, Leypoldt F, Wuerfel JT, et al. Structural Hippocampal Damage Following Anti-N-Methyl-DAspartate Receptor Encephalitis. Biol Psychiatry. 2015; 02. 26. pii:S0006-3223(15)00149-3.

9. Schmitt SE, Pargeon K, Frechette ES, Hirsch LJ, Dalmau J, Friedman D. Extreme delta brush: a unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology. 2012; 79:1094–1100.

10. VanHaerents S, Stillman A, Inoa V, Searls DE, Herman ST. Early and persistent 'extreme delta brush' in a patient with anti-NMDA receptor encephalitis. Epilepsy Behav Case Rep. 2014; 2:67–70.

11. Iizuka T. [Clinical features and pathogenesis of anti-NMDA receptor encephalitis]. Rinsho Shinkeigaku. 2008; 48:920–922.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download