Abstract
Background
Neuromyelitis optica (NMO) is characterized by optic neuritis and longitudinally extensive transverse myelitis. Generally, the brain had been considered healthy in NMO patients, though recent studies have demonstrated that T2-weighted abnormalities may be observed in various brain regions. Logically, NMO brain lesions are localized at sites of high aquaporin-4 expression.
Case Report
A 68-year-old right-handed man with dysuria, weakness in the bilateral upper and lower limbs, and decreased sensation of the lower extremities, was diagnosed with neuromyelitis optica. The patient was gradually speaking less, was showing reduced interest in hobbies, and had undergone changes in character and behavior. An examination was performed using the Seoul Neuropsychological Screening Battery (SNSB), which revealed that the profile of frontal lobe dysfunctions was prominent as compared with other cognitive domains. The patient was treated with prednisolone and azathioprine for about 1 year without recurrence, and showed prognostic improvement according to further SNSB testing.
Neuromyelitis optica (NMO) is an inflammatory disease of the central nervous system mainly characterized by optic neuritis and extensive myelitis where the optic nerve and spinal cord have an inflammatory disease of the central nervous system caused by an autoimmune mechanism.
Its clinical symptoms are similar to multiple sclerosis (MS), which has made it difficult to distinguish between them and has caused confusion in their diagnosis. However, autoantibodies to the water channels protein aquaporin-4 (AQP4) of the central nervous system was found since 2004, the pathogenesis of NMO and many facts about the clinical characteristics had been known.1
The typical characteristics of cognitive functional disorders that were exhibited in patients with MS through the previous study, include deterioration of concentration and information processing speed, decreased memories and frontal lobe dysfunctions and decreased flexibility of thinking.2 The authors report a case that had shown improvement of frontal lobe dysfunctions in NMO after treatment.
A 68-year-old right-handed man with an educational background of a high school diploma had visited the hospital due to weakness in the bilateral upper limbs and lower limbs, decreased sensation of lower extremities and dysuria occurred 5 days ago as main complaints. Due to decreased vision of the left eye, which had occurred seven years ago, and decreased vision of the right eye occurring 2 months before visiting the hospital, he was diagnosed as optic neuritis and received a steroid treatment from other hospital. He had discontinued the medication and was under prognostic observation. The vision in both of his eyes at the time of visiting the hospital were decreased but still he was able to distinguish shapes or colors of all objects.
His consciousness was clear, and eye movements, facial symmetry and sensory functions were normal other than the existing sight disorder. The muscular strength of extremities showed MRC grade III in the right upper limb, grade IV in the left upper limb, and grade IV in both lower limbs. When conducting the sensory test, there were slightly degraded pain senses, vibration senses, tactile senses and location senses below T4 skin fragments. He showed a positive response to Lhermitte's sign where the patient has sensations of electrical current flowing through his bilateral arms when suddenly flexing his head forward. The deep tendon reflexes of extremities were all normal, and both sides showed negative responses to the Babinski reflex. As abdominal distention was observed, 1000 cc of urine was drained after insertion of a urinary catheter.
During the spinal magnetic resonance imaging (spine MRI), a high intensity signal of T2 was shown from C1-T8 spine (Fig. 1) and the findings from the brain MRI were normal. The number of cells, the chemical values and IgG index were normal in the cerebrospinal fluid tests, whereas the oligoclonal band was negative also.
The visual evoked potential test showed poor waveforms from both sides, whereas the left posterior tibial nerve sensory evoked a potential test among the somatosensory evoked potential test showing an abnormality reasonable for central nerve conduction disorder, and the auditory evoked potential test results were normal. Basic blood tests, urinalysis, vasculitis test and thyroid function tests were all normal and from the autoimmune antibody test, it showed positive response to the AQP4 antibody.
As the guardian commented that the patient is gradually speaking less, has a reduction of interest in hobby activities, and has character and behavioral changes such as being unable to control his appetite and becoming furious to insignificant matter, we conducted the Seoul Neuropsychological Screening Battery for additional evaluation.3 The patient's education level was graduation from high school; his score on the Korean Version of the Mini-Mental State Examination was 22 points whereas the clinical dementia rating was 1 point (Table 1). In the case of this patient, the profile of frontal lobe dysfunctions was prominent compared to other cognitive domains.
The patient was diagnosed as NMO and treated with methylprednisolone 1g via IV administration once daily for 5 days. After the treatment, the muscle power of the bilateral upper limbs was observed as MRC grade IV, and the muscle power of his lower limbs was the same as measured at the time of admission. Since the patient had no large scale change in the conditions, he is under prognostic observation as being treated with prednisolone and azathioprine from the out-patient department currently without recurrence for about 1 year. After 1 year of time lapse, we conducted the Neuropsychological Screening Battery (NSB) again for cognitive function evaluation, and frontal lobe functions showing an improving trend but there were no large changes in other domains compared to the conditions before NSB (Table 1).
NMO is a disease that shows clinical findings differentiated from MS and can measure auto-antibodies associated with the disease onset mechanism. Currently, MS occurs as sensitized T-lymphocytes passing through the Blood-Brain Barrier whereas NMO is considered to be an inflammation that occurs through an auto-antibody. In the past, it has been known that NMO did not invade into the brain, and even if any brain lesions were found from MRI images, they were known as asymptomatic. But according to a recent study, brain lesions are found in ≥70% of patients with anti-AQP4 positive antibodies and associated symptoms are expressed in a substantial number of patients.4 In addition, as a case is being identified in whom the brain lesion is expressed as the initial symptom before the optic neuritis and myelitis are displayed, the clinical spectrum of NMO is gradually widening.
Notwithstanding there is a debate on whether anti-AQP4 antibody is just a simple disease specific indicator or if it plays an important role in etiology, but currently it is accepted that anti-AQP4 antibody binds to AQP4 in the central nervous system and through activation of complementary body and immuno-reaction, it plays the role of etiology of NMO, according to the results of several studies. Therefore, in case of NMO that causes the functional damage of the central nervous system, it can be seen as it is natural to have occurrence of dysfunction in cognitive function acting in integrated manner of several sites.
From the previous study, the patients with MS showed the most abnormalities in the information processing speed, memory and execution function and in the patients with NMO, it is known that they showed cognitive dysfunctions with similar frequency.56 In addition, a study result was presented that suggests the decreased cognitive function in NMO is associated with the volumetric reduction of the brain white matters.7
In MS, the immunomodulatory medication and the immunosuppressive medications were reported as effective for treatment of cognitive dysfunctions,5 thereby it is likely to presume that they may present the similar effectiveness after treatment in NMO as well. From the initial NSB actually performed in this patient, frontal lobe dysfunctions were observed notably among cognitive functions and the patient showed prognostic improvement in the NSB performed again after using the medication for treatment of NMO.
This study aimed to differentiate a diagnosis of NMO from MS and other auto-immune diseases invading the central nervous system at an early stage. And in addition to the studies in respect to the mechanism that can improve cognitive functions after medication treatment based on accurate diagnosis in the future, further studies are considered as necessary for the most effective medication regimen in improving cognitive functions through systematic treatment using even more diversified immune-related agents.
Figures and Tables
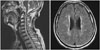 | Fig. 1Sagittal T2-weighted image of spine shows diffuse enlargement of cervical and thoracic spinal cord and continuous high signal intensity in the central gray matter from C1 level. Axial fluid-attenuated inversion recovery image of brain shows high signal intensity lesions in the cerebral periventricular and deep white matter. |
Acknowledgements
This study was supported by a VHS Medical Center Research Grant, Republic of Korea (grant number: VHSMC 15012).
References
1. Lee S, Kim BJ. Diagnosis and treatment of neuromyelitis optica. J Neurocrit Care. 2011; 4:Suppl 1. S38–S41.
2. Lee CN, Park KW. Cognitive impairment in multiple sclerosis. J Mult Scler. 2013; 4:29–35.
3. Ahn HJ, Chin J, Park A, Lee BH, Suh MK, Seo SW, et al. Seoul Neuropsychological Screening Battery-dementia version (SNSB-D): a useful tool for assessing and monitoring cognitive impairments in dementia patients. J Korean Med Sci. 2010; 25:1071–1076.

4. Pittock SJ, Lennon VA, Krecke K, Wingerchuk DM, Lucchinetti CF, Weinshenker BG. Brain abnormalities in neuromyelitis optica. Arch Neurol. 2006; 63:390–396.

5. Blanc F, Zéphir H, Lebrun C, Labauge P, Castelnovo G, Fleury M, et al. Cognitive functions in neuromyelitis optica. Arch Neurol. 2008; 65:84–88.

6. Saji E, Toyoshima Y, Yanagawa K, Nishizawa M, Kawachi I. Neuropsychiatric presentation of neuromyelitis optica spectrum disorders. Neurol. 2010; 74:A169.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download