INTRODUCTION
MATERIALS AND METHODS
Patients
US Analysis
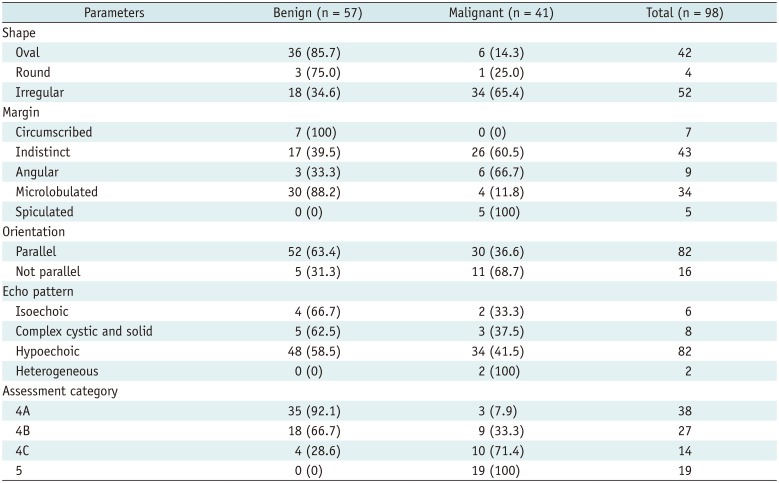
Table 1
Morphologic Characteristics and Assessment Category on B-Mode US
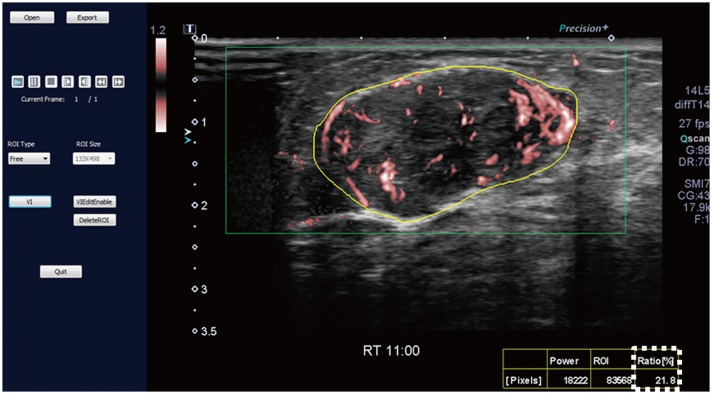 | Fig. 1SMI image and measurement of vascular index.SMI image is opened in dedicated software (VI test app, Canon Medical Systems Corp.) to measure vascular index. Setting yellow-free ROI along boundary of lesion causes vascular index (box outlined by dotted line) to be automatically calculated. Vascular index (%) indicates ratio between pixels for Doppler signal and those for total lesion. ROI = region of interest, SMI = Superb Microvascular Imaging
|
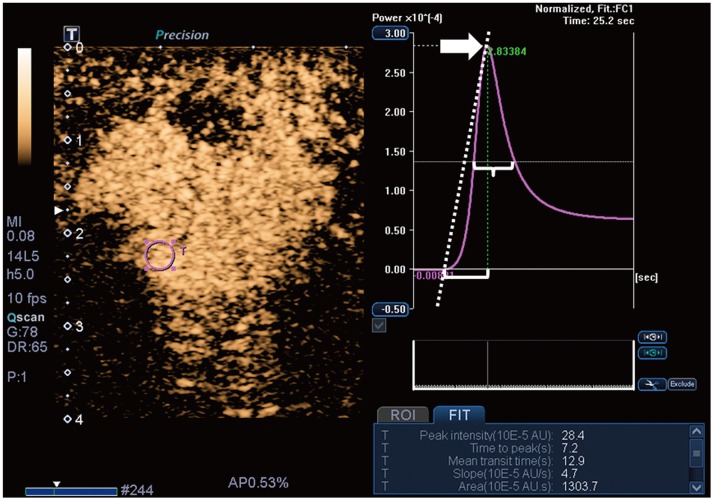 | Fig. 2CEUS image and time-intensity curve analysis.Time-intensity curve analysis of CEUS video clip was performed using built-in software. Setting ROI (pink circle) in area of strongest enhancement causes following quantitative parameters to be automatically calculated: peak intensity (arrow), time to peak (bracket), mean transit time (brace), slope (dotted diagonal line), and area under curve. AU = arbitrary units, CEUS = contrast-enhanced ultrasound
|
Histologic Analysis
Statistical Analysis
RESULTS
Histologic Diagnoses
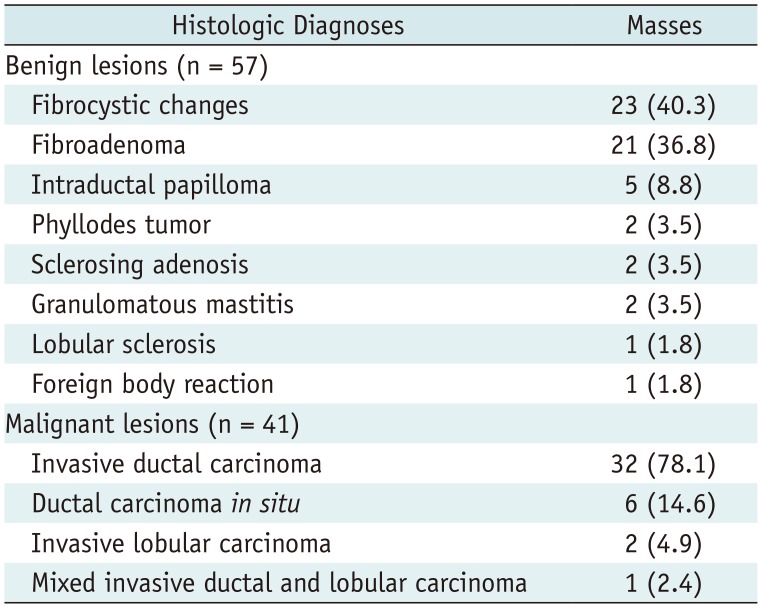
Table 2
Histologic Diagnoses
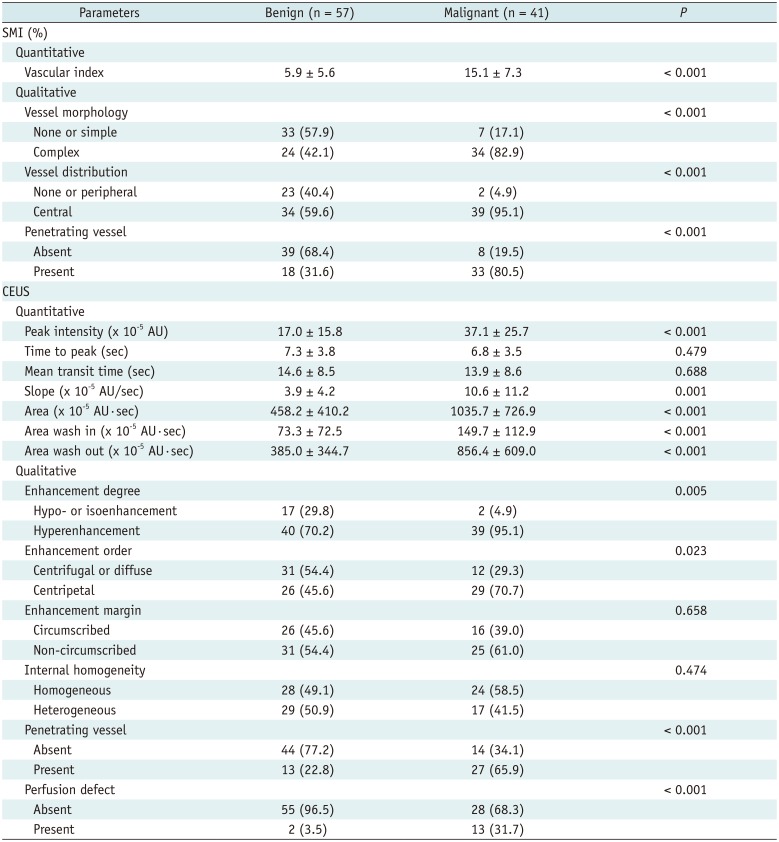
Comparison of SMI and CEUS Parameters between Benign and Malignant Masses
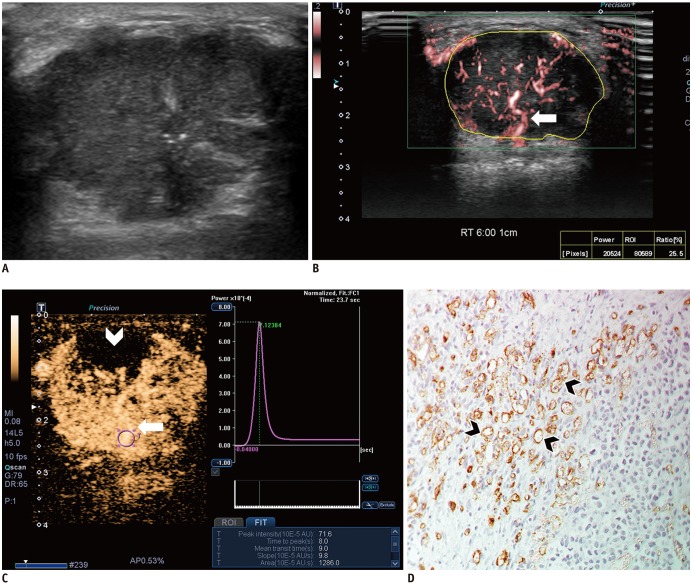 | Fig. 3Images from 44-year-old woman with invasive ductal carcinoma.
A. B-mode image shows 29-mm, irregular, indistinct, hypoechoic mass with internal microcalcifications, which is assessed as BI-RADS category 4C. B. SMI image shows penetrating vessel (arrow) and branching vessels. Vascular index is 25.5%. C. CEUS image shows hyperenhancement of lesion with penetrating vessel (arrow) and perfusion defect (arrowhead). Time-intensity curve shows strong and fast enhancement: peak intensity, 71.6 × 10−5 AU; slope, 9.8 × 10−5 AU/sec; and area under curve, 1286 × 10−5 AU·sec. D. Microvessels (arrowheads) are assessed via immunohistochemical staining with CD34, and mass shows high MVD, 69.3 (× 200 magnification). BI-RADS = Breast Imaging Reporting and Data System, MVD = microvessel density
|
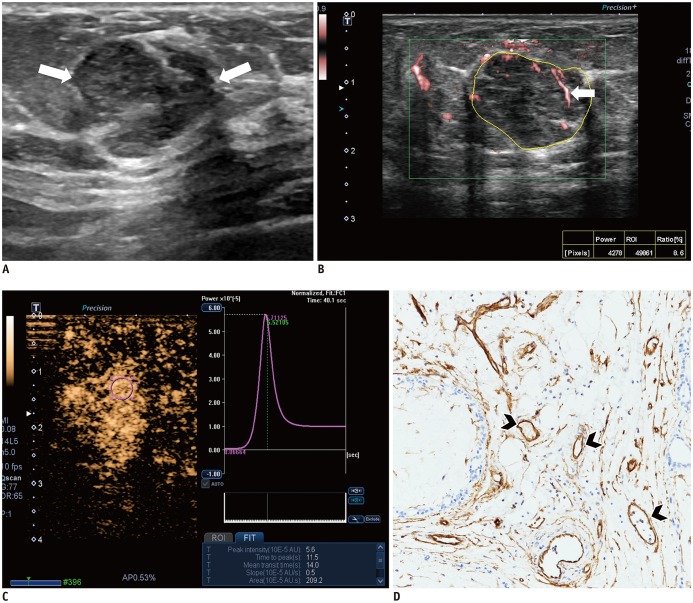 | Fig. 4Images from 54-year-old woman with fibroadenoma.
A. B-mode image shows 16-mm, irregular, indistinct, hypoechoic mass, which is assessed as BI-RADS category 4B (arrows). B. SMI image shows dot-like or linear vessels (arrow). Vascular index is 8.6%. C. CEUS image shows hyperenhancement of lesion without penetrating vessel or perfusion defect. Time-intensity curve shows slow and weak enhancement: peak intensity, 5.6 × 10−5 AU; slope, 0.5 × 10−5 AU/sec; and area under curve, 209.2 × 10−5 AU·sec. D. Microvessels (arrowheads) are assessed via immunohistochemical staining with CD34, and mass shows low MVD, 15.0 (× 200 magnification).
|
Table 3
Comparison of SMI and CEUS Parameters between Benign and Malignant Masses
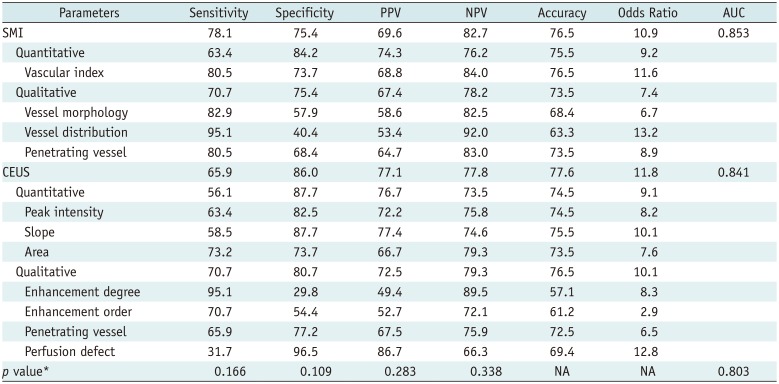
Diagnostic Performance of SMI and CEUS
Table 4
Diagnostic Performance of SMI and CEUS in Distinguishing Malignant from Benign Masses
Effect of the Vascular Parameters of SMI and CEUS on Downgrading BI-RADS Category 4A Masses
Table 5
Effect of Downgrading BI-RADS Category 4A Masses on Basis of Benign Vascular Parameters of SMI and CEUS
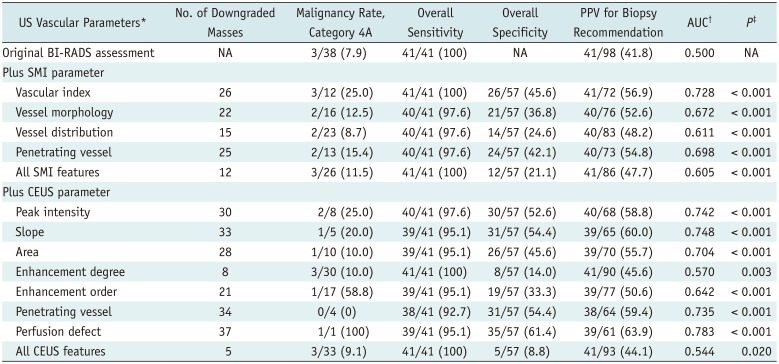
Data are expressed as numbers (%). *Following benign vascular features were used in downgrading mass assessed as BI-RADS category 4A (n = 38) to category 3: vascular index < 8.9, none or simple vessel morphology, none or peripheral vessel distribution, absence of penetrating vessel on SMI, and peak intensity < 27.0, slope < 7.1, area < 583.4, hypo- or isoenhancement, centrifugal or diffuse enhancement, absence of penetrating vessel or perfusion defect on CEUS, †For evaluation of AUC, category 3 masses were considered ‘test negative’ and category 4A or higher masses were considered ‘test positive’, ‡p value was that to null hypothesis that there is no change in AUC with addition of vascular parameter (pairwise comparison of ROC curve).
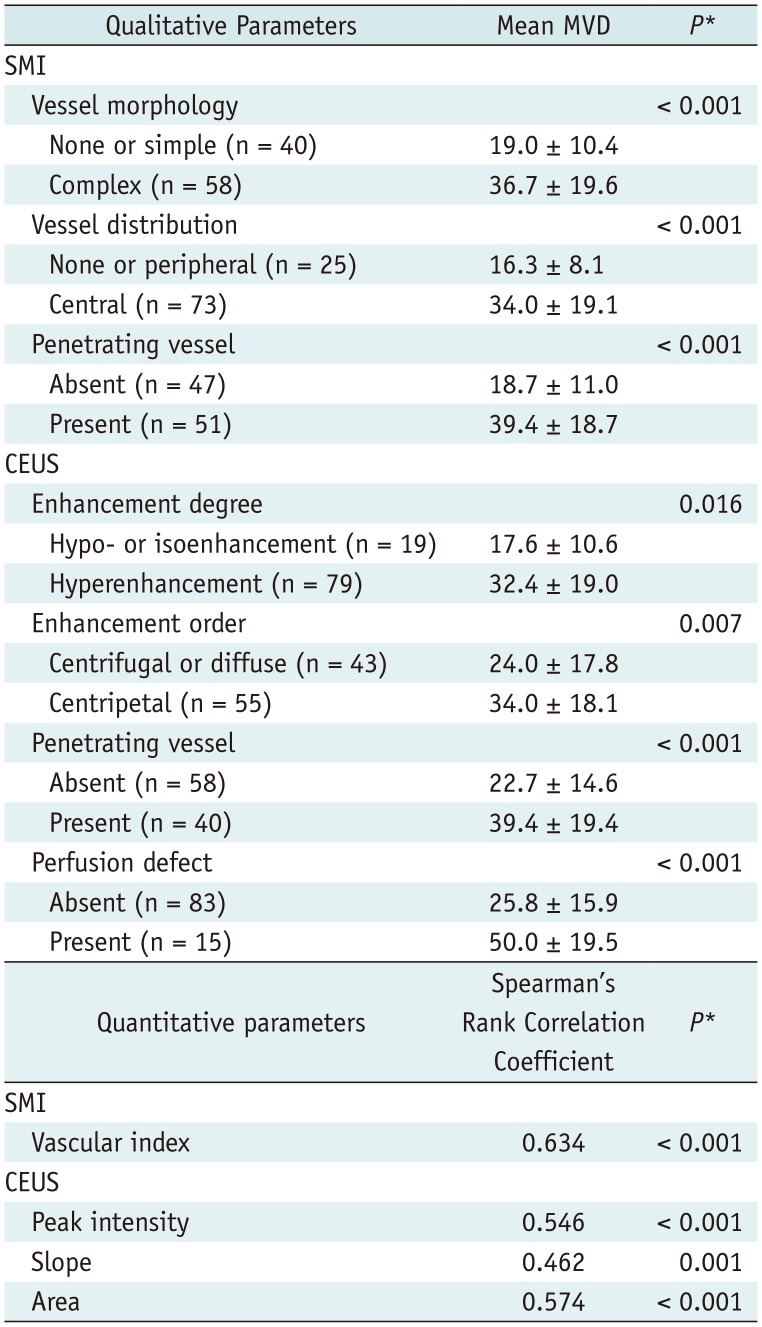
Association between US Vascular Parameters and MVD
Table 6
Association between US Vascular Parameters and MVD
| Quantitative parameters | Spearman's Rank Correlation Coefficient | P* |
|---|---|---|
| SMI | ||
| Vascular index | 0.634 | < 0.001 |
| CEUS | ||
| Peak intensity | 0.546 | < 0.001 |
| Slope | 0.462 | 0.001 |
| Area | 0.574 | < 0.001 |
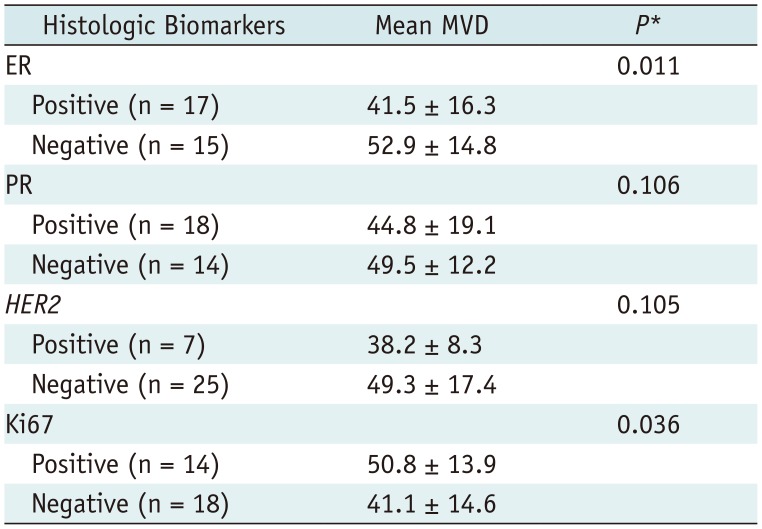
Table 7
Correlation of MVD with Histologic Biomarkers in 32 Invasive Ductal Carcinomas




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download