Abstract
Background and Purpose
This study was performed to newly develop the Way-Finding Ability Scale (WFAS) for middle-aged and older adults and validate its clinical utility.
Methods
The participants for verifying construct validity included 324 adults aged from 45 to 79 years, and 22 normal old adults without way-finding deficit (WFD), 41 amnestic mild cognitive impairment (aMCI), and 35 patients with Parkinson's disease (PD-MCI) for verifying discriminant validity. All participants were administered the newly constructed 28-item WFAS.
Results
Exploratory factor analysis of the WFAS revealed a four-factor solution (sense of direction and inattention, spatial learning and memory, strategic ability, and cardinal direction). This four-factor structure was confirmed by confirmatory factor analysis. The discriminant validity was examined by administering the WFAS to normal older adults and two patient groups (aMCI & PD-MCI). The results showed that the total scores of two patient groups were lower than that of normal older adults. The patients with WFD had significantly lower total scores than those without WFD. Interestingly, the total scores of patients without WFD were significantly lower than those of normal older adults suggesting that the cognitive functions associated with way-finding ability (WFA) were partially impaired in aMCI and PD-MCI patients without apparent WFD. The patients with WFD had consistently lower scores in every four-factor than those without WFD.
The increase in geriatric diseases in elderly population is a cause for concern. Among the geriatric diseases, dementia has received particular attention. Dementia refers to a state involving one or more cognitive impairments, such as attention, language ability, visuospatial function, and frontal/executive function, along with memory impairment, resulting in disability in daily life or work/social life.1 Way-finding deficit (WFD) is a common cognitive symptom in dementia.2345 WFD refers to the inability to find a way in a familiar or new environment. The person with WFD may wander around in a familiar place, may require a long time to learn a new way in a new neighborhood, or in severe cases, may lose the ability to return home. Such difficulties associated with way-finding ability (WFA) may increase the family burden if an accompanying guardian is required to prevent the disappearance or wandering of family members.
There are several instruments to evaluate WFA in clinical practice. However, there is no objective tool to directly measure WFA in patients with dementia in Korea. In other countries, tools using map reading or virtual reality have been developed for research or clinical purpose. However, these tools contain local geographical information and therefore, cannot be used in other areas including Korea. In addition, the road system in Korea does not present a straight-line format, such as streets or avenues. Moreover, the Korean elderly population has limited experience using maps. Therefore, it is a challenge to expect map reading skills among older adults in Korea. It is also difficult to implement the tools using virtual reality among older adults in Korea, who are not familiar with the digital environment. Therefore, clinicians should rely on patients' and caregivers' self-reports to evaluate WFA among older adults and patients with dementia. However, there are no appropriate scales that are validated and standardized for middle-aged and older adults in Korea.
The WFA is related to a variety of cognitive abilities, such as attention, visuospatial function, learning and memory, executive functions, decision-making, map-reading, and monitoring abilities.67891011 Hegarty et al.12 developed a sense-of-direction scale, evaluating the ability in various environmental-spatial tasks for college students. Kato and Takeuchi13 also developed a scale known as the Sense of Direction Questionnaire-Short Form to assess factors associated with the awareness of orientation and memory for general spatial behavior among college students. In Korea, Kwon and Lee6 developed the Wayfinding Ability Test, which examines diverse cognitive functions, such as spatial memory and learning, sense of direction, map usage, and visuospatial perception among college students. Hong and Lim.14 colleagues developed the Way-finding Effectiveness Scale consisting of complex way-finding goals, simple way-finding goals, analytical and global strategies for patients with dementia. Pai et al.15 developed a scale designated as the Questionnaire on Every Navigational Ability for assessing landmark agnosia, egocentric agnosia, inattention, and heading disorientation in patients with Alzheimer's disease dementia.
Those scales for WFA were developed for limited targets such as college students and patients with dementia. Further, the cognitive abilities measured by each of the scales were different. Therefore, it is necessary to develop a new scale that evaluates the comprehensive cognitive abilities required for WFA in middle-aged and older adults including patients with dementia. The new scale will be designed to elucidate the decline of WFA with normal aging. It will also provide important information highlighting the differences between the decline decline in WFA during normal aging and WFD in patients with dementia.
The purposes of this study were to develop a self-report questionnaire, the Way-Finding Ability Scale (WFAS) for middle-aged and older adults and to evaluate the clinical usefulness of WFAS by examining the ability of the newly developed WFAS to distinguish not only the presence but also the degree of WFD in the normal elderly population and in patients with mild cognitive impairment (MCI) with or without WFD.
A total of 324 (157 males, 167 females) aged between 45 and 79 years (middle-aged and older adults) who were residents in Seoul, Incheon, or Gyeonggi province, participated in the study. All the subjects meeting the health screening criteria proposed by Christensen et al.16 had no history of neurological or psychiatric illnesses affecting cognitive functions (Table 1).
The participants included 22 normal old adults without WFD, 41 patients with amnestic mild cognitive impairment (aMCI), and 35 patients with Parkinson's disease (PD). The normal older adults reporting no cognitive complaints met the health screening criteria proposed by Christensen et al.,16 without a history of neurological or psychiatric illnesses affecting cognitive functions. They showed a normal range of performance in the Korean-Mini Mental State Examination (K-MMSE), 171819 in which the total score was above the 16 percentile, and in the Korean-Instrumental Activities of Daily Living (K-IADL),20 in which the score was lower than 0.43.
Patients with aMCI and PD were selected from those who visited the Department of Neurology at Hallym University Sacred Heart Hospital. The aMCI met Petersen's criteria for MCI,21 showing memory impairment with one or more deficits in other cognitive domains in the comprehensive neuropsychological test, while the activities of daily living were maintained within the normal range. Patients with PD were diagnosed with probable PD based on the UK brain bank standard22 and showed ≤3 on the Hoehn & Yahr staging scale.23 They had MCIs met Petersen's criteria for MCI (PD-MCI) with <0.43 on the K-IADL. The Clinical Dementia Rating (CDR)242526 scores of all patients were 0.5.
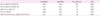
All participants for verifying discriminant validity were divided into two subgroups, with and without WFD, based on the WFD screening questionnaire developed by the Clinical Research Center for Dementia (CRCD).27 All the normal older adults reported the absence of WFD. In the aMCI group, 22 reported the absence of WFD (aMCI-N), while 19 reported WFD (aMCI-W). In the PD-MCI group, 20 patients reported the absence of WFD (PD-N) and 15 reported WFD (PD-W) (Table 2).
The Health Screening Questionnaire16 was administered to normal middle-aged and older adults for construct validity. The K-MMSE and K-IADL as well as the Health Screening Questionnaire were used to screen the normal elderly Koreans for discriminant validity. All the patients were subjected to the Seoul Neuropsychological Screening Battery, 2nd edition (SNSB-II)19 including measures of attention, language, visuospatial, memory, and frontal/executive functions as well as the K-MMSE, K-IADL, and CDR.
The following four questions developed by CRCD27 were used: 1) Have you ever been unable to find the right direction or the way when you traveled to your destination or return home? 2) Have you ever lost your way to an unfamiliar place (one or two visits last year)? 3) Have you ever been lost in your neighborhood community? Have you ever lost your building or your unit number in your apartment complex? and 4) Have you ever lost the way to the bathroom in your house? If one responded “ye”s to one or more of these questions, a case of WFD was classified.
The preliminary items were collected from the existing scales of previous studies.612131415 One of the investigators (SJK) selected 55 preliminary items appropriate for middle-aged and older adults and that assessed various cognitive functions required for WFA such as sense of direction, memory, and executive function. Two clinical psychologists, a professor of clinical neuropsychology (YK) and a licensed clinical psychologist, selected the final 28 items after evaluation of the appropriateness of the 55 items. Among the selected items, the items in Korean were used as indicated on the existing scale. The items in English, however, were first translated by the researchers and back-translated by a native speaker to confirm the accuracy of translation (Table 3). Each item was scored on a 5-point Likert scale (1: strongly disagree, 2: disagree, 3: neutral, 4: agree, and 5: strongly agree). Some of the items were reverse-coded. The total score ranged from 28 to 140, with the higher values indicating better performance.
ANOVA and Chi-square tests were used to detect group differences for demographic variables such as age, education, and sex. To confirm the reliability of the WFAS, Cronbach's α and intra-class correlation (ICC) were calculated. Exploratory and confirmatory factor analyses were performed to evaluate construct validity. We performed a multivariate analysis of covariance (MANCOVA) controlling for age on the WFAS total and subscale scores. In addition, we conducted post-hoc contrast analyses for multiple comparisons to analyze group differences. To confirm the sensitivity and specificity of the WFAS, the receiver operating characteristic (ROC) curve was analyzed. All p-values were two-tailed, and statistical significance was accepted at p<0.05. SPSS version 19.0 (IBM Corp., Armonk, NY, USA) and AMOS version 20.0 (IBM Corp.) were used for data analysis.
Internal consistency and test-retest reliability analyses were conducted to evaluate the reliability of the WFAS. The Cronbach's α was 0.92 for the overall scale, and 0.59–0.90 for the four factors (0.89 for sense of direction and inattention, 0.90 for spatial memory and learning, 0.59 for strategic ability, and 0.75 for cardinal direction). To confirm the test-retest reliability, 30 middle-aged and older adults, who were randomly selected from the total normal participants, were retested at intervals of 5 to 6 weeks. The test-retest reliability (ICC) of the WFAS total score was r=0.78 (p<0.001) and that of the factors was 0.77–0.90 (p<0.001) (0.90 for sense of direction and inattention, 0.77 for spatial memory and learning, 0.88 for strategic ability, and 0.80 for cardinal direction).
First, Kaiser-Meyer-Olkin (KMO) index for sampling adequacy28 and Bartlett's Test of Spericity29 were inspected to determine whether the data (n=324) for construct validity were appropriate for factor analysis. The KMO value was 0.93 and the sphericity was significant at p<0.001. Therefore, it was confirmed that this data was appropriate for factor analysis, and exploratory factor analysis was performed initially. Principal axis factoring with oblique rotation was used as the factor extraction method. The number of factors was determined by examining the cumulative percentage of variance, the scree plot, and the eigenvalues. As a result, the following four factors were extracted: 1) sense of direction and inattention, 2) spatial learning and memory, 3) strategic ability, and 4) cardinal direction. These four factors explained 53.98% of the total variance (35.16, 7.76, 6.63, and 4.43%, respectively) (Table 4). Moderate-to-strong correlations between factors were found between “sense of direction and inattention” and “spatial learning and memory” (r=0.74), “spatial learning and memory” and “cardinal direction” (r=0.67), and “sense of direction and inattention” and “cardinal direction” (r=0.63). A moderate correlation was found between “sense of direction and inattention” and “strategic ability” (r=0.44). Relatively weak correlations were found between “spatial learning and memory” and “strategic ability” (r=0.25) and “strategic ability” and “cardinal direction” (r=0.32).
A confirmatory factor analysis was performed using AMOS to confirm whether the factor structure model obtained using exploratory factor analysis was appropriate. The results confirmed the model obtained by exploratory factor analysis [χ2(344)=700.10, p<0.001, GFI=0.87, TLI=0.90, CFI=0.91, RMSEA=0.06 (0.0–0.06)]. In order to re-verify the validity of the 4-factor structure extracted from 324 normal middle-aged and older adults, the confirmatory factor analysis was conducted again using 98 normal (n=22) and clinical groups (aMCI & PD=76). The result re-confirmed that the model obtained by exploratory factor analysis was valid [χ2(344)=544.96, p<0.001, GFI=0.73, TLI=0.85, CFI=0.87, RMSEA=0.07 (0.06–0.09)].
A MANCOVA controlled for age was conducted to compare the normal elderly and dementia patients with or without WFD, such as Normal, aMCI-N, aMCI-W, PD-N, and PD-W (Table 5). First, there were significant differences among groups in the total score of WFAS (F=40.12, p<0.001). The normal elderly group showed the highest total score, followed by aMCI-N and PD-N. The aMCI-W and PD-W, who reported WFD, showed the lowest total scores. There were no significant differences in total scores between aMCI-N and PD-N or between aMCI-W and PD-W.
The factor scores of “sense of direction and inattention” and “cardinal direction” were the highest in the normal and aMCI-N groups, and were sequentially lowered in PD-N, aMCI-W, and PD-W. The score of “spatial learning and memory” was the highest in the normal group, and declined sequentially in PD-N, aMCI-N, PD-W, and aMCI-W. The normal elderly group showed significantly higher “strategic ability” score than the aMCI, while the aMCI showed significantly higher score than the PD. Among the patient groups of aMCI and PD, there were no significant differences between the groups with and without WFD in “strategic disability.”
ROC curve analyses were performed to examine the sensitivity and specificity of the WFAS (Table 6). The WFAS had moderate accuracy30 (AUC=0.80, p<0.001; sensitivity 0.68, specificity 0.91, cut-off score 102) in differentiating the normal from the patient groups without WFD (NC vs. aMCI-N & PD-N). The WFAS total score, however, was found to be highly accurate in differentiating between normal and patient groups with WFD (NC vs. aMCI-W & PD-W, AUC=0.96, p<0.001; sensitivity 0.91, specificity 0.91, cut-off score 82), between aMCI-N and aMCI-W (AUC=0.98, p<0.001), between PD-N and PD-W (AUC=0.97, p<0.001), and between patient groups without WFD (aMCI-N & PD-N) and those with WFD (aMCI-W & PD-W) (AUC=0.96, p<0.001).
In this study, we developed a self-report questionnaire for the evaluation of WFA. It was confirmed that this scale reliably and adequately assessed the degrees of WFD in patients with and without WFD.
The exploratory factor analysis was conducted to examine the construct validity of WFAS. Four sub-factors were extracted, which accounted for 53.98% of the total variance. Most items of the first factor “sense of direction and inattention.” were similar to the items involving the “inattention” factor (3rd factor) in the scale developed by Pai et al.15 for patients with Alzheimer's disease. They were also partly similar to the items in the “sense of direction” factor (2nd factor) of the Kwon and Lee's scale6 developed for college students. The items in the second factor, “spatial learning and memory,” were similar to those of the first factor (spatial memory and learning) in the Kwon and Lee's scale.6 The third factor, “strategic ability,” was similar to the “analytical strategy” factor (3rd factor) in the Hong and Lim's scale14 developed for patients with dementia.
The last factor consisting of 3 items was designated as “cardinal direction.” These items were extracted as the second factor (sense of direction) with a large explained variance in the Kwon and Lee's scale,6 which was developed for college students. However, they were extracted as the fourth factor with relatively small explained variance in the WFAS. In addition, the “map usage” factor in the Kwon and Lee' scale6 was not an independent factor in the WFAS. These results suggest that middle-aged and older adults in Korea do not use map or cardinal direction as much as the college students to find their way. They suggest that the WFD in the middle-aged and older adults varied from that of college students and the effect of different cognitive impairments varied with the age cohort. Therefore, it is necessary to develop novel way-finding ability scales tailored to middle-aged and older adults compared with the scales for younger adults (college students). This four-factor structure revealed in exploratory factor analysis was confirmed in confirmatory factor analyses.
In order to examine the discriminant validity of the WFAS, we compared the WFAS total scores of normal older adults, aMCI, and PD patients with or without WFD. We found that patients with WFD (aMCI-W and PD-W) had the lowest score, followed by patients without WFD (aMCI-N and PD-N), and the score was the highest in normal older adults. This result suggested that the total WFAS score can be used to diagnose WFD. It was interesting that patients without WFD (aMCI-N and PD-N) showed a significantly lower WFAS total score compared with normal older adults. This finding suggests that the cognitive functions related to WFA were partially impaired in aMCI and PD-MCI patients without apparent WFD. Therefore, WFAS can be used to determine the degree of WFA as well as predict or prevent WFD even in cases without WFD complaints.
The variation in scores among factors associated with WFAS was also analyzed. The scores obtained for the following three factors, “sense of direction and inattention,” “spatial learning and memory,” and “cardinal direction,” in patients with WFD (aMCI-W and PD-W) were significantly lower than in those without WFD (aMCI-N and PD-N). This finding suggested that the three factors can be effectively used to differentiate WFD. However, there was no difference in “strategic ability” between patients with and without WFD. Instead, the PD group showed significantly lower scores than the aMCI group, regardless of WFD. The items included in the “strategic ability” factor included questions related to the use of memory strategy in relation to way-finding. Therefore, they included items that evaluated frontal/executive functions. The result was attributed to greater frontal/executive dysfunction in patients with PD than in those with aMCI with same degree of dementia severity (CDR score of 0.5). Therefore, we conclude that compared with previous studies1415 reporting that the strategic use such as landmarks was critical for WFA, it does not effectively discriminate WFD in patients with aMCI and PD-MCI.
The factor scores including “sense of direction and inattention,” “strategic ability,” and “cardinal direction” were higher in those with aMCI-N compared with PD-N, and in patients with aMCI-W compared with PD-W, respectively. The factor score of “spatial learning and memory” was lower in aMCI-N compared with PD-N, and in aMCI-W compared with PD-W, respectively. The factors of “sense of direction and inattention,” “strategic ability,” and “cardinal direction” comprised several items that assessed visuospatial dysfunction or frontal/executive dysfunction starting from the early stage of disease in many patients with PD. On the other hand, “spatial learning and memory” factor consisted of items related to learning and memory impairments that played a major role in patients with aMCI. Stern et al.31 reported that at similar stages of dementia, PD patients with dementia presented worse visuospatial dysfunction compared with AD patients with dementia. However, Huber et al.32 found that the AD patients presented worse memory impairment compared with PD dementia patients. Our results were consistent with these findings, suggesting that the items and factors of WFAS were appropriate for the evaluation of diverse cognitive functions relating to the WFD.
The results of ROC curve analysis confirmed that the WFAS total score represented a robust rate of discrimination. The discriminant accuracy (AUC=0.96) was very high between normal older adults and patients with WFD (aMCI-W, PD-W). The accuracy of discrimination between patients with and without WFD in aMCI (aMCI-N vs. aMCI-W) and PD (PD-N vs. PD-W) groups was also very high at 0.98 and 0.97, respectively. Interestingly, even the discriminant accuracy between normal older adults and patients without WFD [NC vs. (aMCI-N & PD-N)] was moderate (0.80). As mentioned previously, these results suggest that the aMCI and PD patients without apparent WFD may have minor cognitive impairments based on WFAS. Therefore, the WFAS scale can be used for detection and early intervention of WFD as well as predicting WFD based on the degree of WFA deterioration.
The newly developed WFAS was verified for reliability and validity in the present study. By contrasting to the existing scales, which were targeted only at young adults (especially university students) or patients with dementia (mainly Alzheimer's disease dementia), the WFAS extended the scope of application to middle-aged and older adults. In addition to the aMCI known as the prodromal stage of Alzheimer's disease dementia, it was also applied for PD to confirm the ability of WFAS for WFD diagnosis in various patient groups. In summary, it can be concluded that the WFAS can be used to not only distinguish normal older adults and MCI patient groups effectively but also significantly differentiate between patients with WFD and those without WFD within the MCI population.
The WFAS is a self-report questionnaire. Therefore, the present study obtained clinical data only from patients with MCI, and not dementia for collecting reliable data. Whether the WFAS can be answered by caregivers of dementia patients should be considered in further studies. Although the WFAS, which consists of 28 questions, provides rich and reliable information related to WFD, it is a long and tedious tool for clinical use. It is expected that a shorter version of the WFAS will be developed in a future study.
Figures and Tables
Table 2
Demographics of normal older adults and clinical groups for verification of discriminant validity

*p<0.001.
aMCI: amnestic mild cognitive impairment, aMCI-N: aMCI-no way-finding deficit, aMCI-W: aMCI-way-finding deficit, K-MMSE: Korean-Mini Mental State Examination, NC: normal control, PD-MCI: Parkinson's disease-mild cognitive impairment, PD-N: PD-no way-finding deficit, PD-W: PD-way-finding deficit.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). Washington, DC: American Psychiatric Association;1994.
2. Iachini I, Iavarone A, Senese VP, Ruotolo F, Ruggiero G. Visuospatial memory in healthy elderly, AD and MCI: a review. Curr Aging Sci. 2009; 2:43–59.

3. Benke T, Karner E, Petermichl S, Prantner V, Kemmler G. Neuropsychological deficits associated with route learning in Alzheimer disease, MCI, and normal aging. Alzheimer Dis Assoc Disord. 2014; 28:162–167.

4. Allison SL, Fagan AM, Morris JC, Head D. Spatial navigation in preclinical Alzheimer's disease. J Alzheimers Dis. 2016; 52:77–90.

5. Davis R, Weisbeck C. Creating a supportive environment using cues for wayfinding in dementia. J Gerontol Nurs. 2016; 42:36–44.

6. Kwon H, Lee J. A study of development and validation of the Way-finding Ability Test (WAT). Korean J Psychol. 2005; 24:1–10.
7. Berthoz A, Viaud-Delmon I. Multisensory integration in spatial orientation. Current Opinion in Neurobiology. 1999; 9:708–712.

8. Nadolne MJ, Stringer AY. Ecologic validity in neuropsychological assessment: prediction of wayfinding. J Int Neuropsychol Soc. 2001; 7:675–682.

9. Corbetta M, Kincade JM, Shulman GL. Neural systems for visual orienting and their relationships to spatial working memory. J Cogn Neurosci. 2002; 14:508–523.

10. Burgess N. Spatial memory: how egocentric and allocentric combine. Trends Cogn Sci. 2006; 10:551–557.

11. Lepsien J, Nobre AC. Cognitive control of attention in the human brain: insights from orienting attention to mental representations. Brain Res. 2006; 1105:20–31.

12. Hegarty M, Richardson AE, Montello DR, Lovelace K, Subbiah I. Development of a self-report measure of environmental spatial ability. Intelligence. 2002; 30:425–447.

13. Kato Y, Takeuchi Y. Individual differences in wayfinding strategies. J Environ Psychol. 2003; 23:171–188.

14. Hong GRS, Lim Y. Reliability and validity of the Korean version of the way-finding effectiveness scale for persons with dementia. J Clin Nurs. 2009; 18:1625–1631.

15. Pai MC, Lee CC, Yang YC, Lee YT, Chen KC, Lin SH, et al. Development of a questionnaire on everyday navigational ability to assess topographical disorientation in Alzheimer's disease. Am J Alzheimers Dis Other Demen. 2012; 27:65–72.

16. Christensen KJ, Multhaup KS, Nordstrom S, Voss K. A cognitive battery for dementia: development and measurement characteristics. J Consult Clin Psychol. 1991; 3:168–174.

17. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12:189–198.
18. Kang Y. A normative study of the Korean-Mini Mental State Examination (K-MMSE) in the elderly. Korean J Psychol. 2006; 25:1–12.
19. Kang Y, Jahng S, Na DL. Seoul Neuropsychological Screening Battery, 2nd ed. (SNSB-II). Seoul: Human Brain Research & Consulting Co.;2012.
20. Kang SJ, Choi SH, Lee BH, Kwon JC, Na DL, Han SH. Korean Dementia Research Group. The reliability and validity of the Korean Instrumental Activities of Daily Living (K-IADL). J Korean Neurol Assoc. 2002; 20:8–14.
21. Petersen RC. Clinical practice. Mild cognitive impairment. N Engl J Med. 2011; 364:2227–2234.
22. Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992; 55:181–184.

23. Hoehn MM, Yahr MD. Parkinsonism: onset, progression, and mortality. Neurology. 1967; 17:427–442.

25. Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993; 43:2412–2414.
26. Choi SH, Na DL, Lee BH, Hahm DS, Jeong JH, Yoon SJ, et al. Estimating the validity of the Korean version of expanded Clinical Dementia Rating (CDR) scale. J Korean Neurol Assoc. 2001; 19:585–591.
27. Moon SY, Park DH, Lee SM, Kim SY. Clinical significance of topographical disorientation in mild cognitive impairment. Dement Neurocogn Disord. 2009; 8:84–87.
29. Tobias S, Carlson JE. Brief report: Bartlett's test of sphericity and chance findings in factor analysis. Multivariate Behav Res. 1969; 4:375–377.

30. Greiner M, Pfeiffer D, Smith RD. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev Vet Med. 2000; 45(1-2):23–41.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download