Abstract
Until recently, there is considerable mess regarding the nature of anxiety in dementia. However, anxiety is common in this population affecting from 8% to 71% of prevalence, and resulted in poor outcome and quality of life, even after controlling for depression. Because a presentation of anxiety in the context of dementia can be different from typical early-onset anxiety disorder, it is not easy one to identify and quantify anxiety reliably. Moreover, differentiating anxiety from the depression and/or dementia itself also can be formidable task. Anxiety gradually decreases at the severe stages of dementia and this symptom may be more common in vascular dementia than in Alzheimer's disease. Due to the lack of large randomized clinical trials, optimal treatment and the true degree of efficacy of treatment is not clear yet in this population. However, these treatments can reduce adverse impact of anxiety on patients and caregivers. This article provides a brief review for the diagnosis, evaluation and treatment of anxiety in dementia.
Go to : 
For the past years, dementia is growing health problem. A serious and common complications of dementia is occurrence of neuropsychiatric and behavioral problems. Among them, anxiety symptoms in this population have received little attention.1 Anxiety, however, is common symptoms in patients with dementia with prevalence estimates ranging from 8% to 71% for anxiety symptoms and from 5% to 21% for anxiety disorders.23 This is also associated with poor quality of life, behavior problems, impairment of activities of daily living, sleep disturbances and poorer cognitive functions, independent of co-presence of depression. Anxiety in dementia is also predictor for future nursing home placement, suggesting that it is a serious caregiver's burdens.4
In this paper, we intergrate more recent studies for anxiety in dementia. First, we address how we detect anxiety and what is the best way to define anxiety in context of dementia. Second, we discuss the instruments that have been used to screen and assess anxiety in dementia. Though, not fully validated these tools, we recommend the certain assessment tools. Third, we examine the clinical characteristics and empirical treatment of anxiety in dementia. Finally, we discuss existing limitations and recommendations for future research.
Though, generalized anxiety disorder (GAD) is the common neuropsychiartric symptoms in dementia, the well-designed studies of prevalence and incidence of anxiety have been relatively sparse, due to the case selection difficulties and the overlapping symptomatology associated with dementia. In community setting, prevalence is 2–7%, and a prevalence is around 10% in primary care setting in elderly population.5 However, in patients with dementia, the rate of anxiety rises to between 38% and 72%.6 Although anxiety symptoms and disorders are more common in women within the elderly without dementia, sex differences is not found in most studies in anxious patients with dementia.6
Many studies have searched for factors influencing the presentation of anxiety in dementia. No relationship has been found with age, gender6 or education.7 Compared with White or African Americans, higher rates of anxiety in dementia have been found among Hispanics and Asians.8 Anxiety is more common in vascular,6 frontotemporal and Parkinson's dementias9 than in Alzheimer's disease (AD).
Anxiety was seldom the main reason for referral to the dementia clinic. Changes in the elderly persons' behavior and cognitive functions were two of the main reasons for referrals. To make the diagnosis of anxiety in patients with dementia, a multidisciplinary comprehensive assessment may be needed. This is necessary not only to confirm the presence of anxiety symptoms, but also to explore possible biopsychosocial etiological factors for anxiety.
Physical examination and laboratory investigations are important to detect and treat physical disorders that predispose, precipitate or mimic anxiety. Medications such as steroids, antidepressants and anticholinergics can cause anxiety, and alcohol and other substance use should be evaluated. Despite the careful assessment of anxiety in dementia, diagnosing anxiety can be difficult and are often overlooked by clinicians.10 The reasons for this: first, the symptoms of dementia and anxiety may overlap. Diagnostic & Statistical Manual of Mental Disorders-V (DSM-V) criteria of GAD include excessive anxiety and worry that is difficult to control with at least three of the following anxiety symptoms: restlessness, fatigue, concentration problems, irritability, muscle tension, and sleep disturbance for 6 months. However, anxiety symptoms such as restlessness, being easily fatigued, and difficulty in concentrating can also frequently occur in dementia patients without anxiety.10 It might also be difficult to distinguish between symptoms of anxiety and other behavioral and psychological symptoms of dementia (BPSD) such as irritability, aggression, wandering, and sleep disturbance.14 Therefore, anxiety symptoms are often considered a part of dementia itself and sometimes it regarded as a nonspecific result of severe dementia,2 but this is still unknown.15
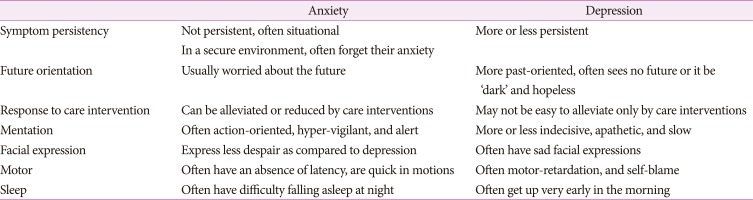
Second, differentiating anxiety from other neuropsychiatric symptoms might be difficult. Distinguishing anxiety from depression is important because co-morbid depression may increase risk of delayed remission and early relapse.16 The depression and anxiety is frequently co-occurred.1718 Between 68% and 75% of individuals with dementia and anxiety disorder also meet the criteria for a major depressive disorder.10 Observing patient behavior and body language may help clinicians to differentiate between symptoms of anxiety and depression in patients with dementia. Calleo and Stanley19 suggested three important points to differentiating between anxiety and depression: 1) defining the sequence of symptoms, i.e., which came first, anxiety or depression; 2) identifying the severity of the depression or anxiety; and 3) determining which symptom is more prominent in the clinical presentation: fear or sadness. Other subtle different clinical symptomatology may be helpful for differential diagnosis (Table 1).
Third, there is few consensus about how to define anxiety in dementia. Currently, the diagnostic criteria for GAD is the same for patients with and without dementia.10 Revised criteria for anxiety diagnosis in patients with dementia recommended excessive anxiety or worry that is difficult to control as the key components with at least three of the following symptoms: restlessness, irritability, muscle tension, excessive fears, and respiratory distress.15 However, recent study suggested only the muscle tension and fatigue are specific for the GAD in patients with dementia.20
Fourth, memory- and language problems in patients with dementia compromise expression of their feelings, and therefore, the assessment process may be difficult. In this situation, behavior of these patients can be more helpful for identifying these symptoms and caregiver, the information of caregiver for these patients are therefore of great importance.
In summary, the current diagnostic system of anxiety in patients with dementia is not sufficient yet, so multidisplinary and comprehensive approach may be essential for identification of this symptom.
The anxiety can be commonly occurred before the dementia is not apparent. A study of anxiety in elderly people with mild cognitive impairment (MCI) reported that individuals with a Generalized Anxiety Inventory score ≥10 showed more behavioral and psychological symptoms, agitation, anxiety, depression and sleep disorders.21 Instrumental activities of daily living and executive functions assessed by the Trail Making B Test are also more compromised. High levels of anxiety in patients with MCI have an adverse effect on executive functioning.
In early AD, anxiety (but not depression) predict a decline in learning as measured on the Auditory Verbal Learning Test.22 In a prospective study of anxiety and cognition in 1481 men aged between 48 and 67, participants were reassessed after 17 years' follow-up.23 Vascular risk factors and poorer premorbid cognitive function were significantly associated with anxiety, and decline in learning and memory was associated with high baseline anxiety scores. Older adults reporting high levels of anxiety and depression perform poorly on tasks assessing attention and concentration, set-shifting, and working and episodic memory.24 Recent longitudinal study of AD and DLBD with anxiety of 4 years follow up showed no clear association between anxiety and the rate of cognitive decline or dementia severity.25 These conflicting results may be result from methodological differences and non-linear interactions between anxiety and test difficulty. So well-designed prospective study may be needed to clarify these relationships.
Neuropsychiatric symptoms, such as depression and anxiety, are frequent in MCI. Much research has focused on the link between depression and AD, however, there is few studies concerning anxiety as a risk factor for dementia as a general. Several studies regarding specifically to AD are present now. Past or current anxiety in MCI may augment the risk of AD conversion by as much as 2.5-fold.262728 Conversely, anxiety may be protective factor against AD29 or have no impact.30 Although methodologic differences may account for the disconcodant results, potential impact of concurrent depression should be considered.31 Thus, although evidence from large observational studies supports an association between anxiety in MCI and AD risk, how much depression contribute toward this is not yet clear.
There are few structured and standardized measures for screening, diagnosing and rating the severity of anxiety comorbid with dementia. The screening tools for identifying anxiety should be used alongside the screening tools for depression and other BPSD because of their high co-existence.
The Behavioral Pathology in Alzheimer's Disease Scale (BEHAVE-AD) comprises seven domains, and each domain are assessed based on a caregiver interview.32 The anxiety domain encompass four sub-items: anxiety regarding upcoming events, other anxieties, fear of being left alone, and other phobias. Thus the BEHAVE-AD asks the caregiver to make broad judgments about the presence of fears and anxieties, rather than asking about specific symptoms (e.g., sweating).
The Neuropsychiatric Inventory (NPI) comprises ten domains, two additional domains are added in a later version.33 Thus assess the symptoms within the last 30 days and, like the BEHAVE-AD, the NPI score is based on an interview with a caregiver. For each domain, a screening question is done and if yes for this question, then followed by more specific questions. For anxiety, the specific questions are: worrying about planned event, feeling shaky, unable to relax or tense, shortness of breath or gasping, butterflies in stomach or racing/pounding heart, avoiding certain situations, nervousness when separated from caregiver, and other symptoms of anxiety. Strong correlations have been reported between the NPI and the BEHAVE-AD anxiety domains but, because the rate of overall neuropsychiatric symptoms was not controlled, they provide little information about construct validity.
Rating of Anxiety In Dementia (RAID) is dementia-specific instrument.34 This 20-item scale has good interrater reliability, sensitivity and specificity. It correlates highly with the DSM-IV diagnosis of GAD (American Psychiatric Association, 1994). RAID is highly correlated with the anxiety domains of the BEHAVE-AD rating scale and the NPI.33
The Worry Scale is designed as a self-report measure for anxiety in mild dementia and has good internal consistency. This is well correlated with trait and state anxiety, and it also correlates strongly with measures of depression.35 Other scales that are also sensitive to the presence of depression include the Hospital Anxiety and Depression Scale, although this was not designed for use in dementia.
However, none of the existing instruments is entirely adequate, because it has not confirmed the constructal validity, but three instruments (the NPI, BEHAVE-AD and RAID) have some preliminary support and used for several studies. The NPI or the BEHAVE-AD can also be used to assess neuropsychiatric symptoms in general, including anxiety. For studies where anxiety is a primary focus, the RAID, though it is imperfect, has the best option at this point.
Both psychological and biological mechanisms probably cause the anxiety in patients with dementia. Patients with dementia experience less coping ability in daily living, lose overview and control, and might fear for the future.1036 In addition, atrophy and dysfunctions in the limbic structures may compromise the ability of coping with fear and anxiety.37 Higher levels of cortisol due to stress can also cause hippocampal atrophy.38 In animal models of AD, stress-level glucocorticoid steroid administration resulted in increases in amyloid formation and tau accumulation.39 The well-established relationships among stress, cortisol, and hippocampal atrophy in humans suggest that anxiety may increase AD risk indirectly through cortisol-mediated hippocampal neurotoxicity.40 Chronic stress may also contribute to development of through pathways related to increased allostatic load, such as effects on the cardiovascular system and plasticity changes to brain structures.
Furthermore, anxiety in individuals with MCI was associated with abnormal concentrations of Ab42 and t-tau in cerebrospinal fluid, whereas conversely depression and apathy were not, which may also support the bio-pathological mechanisms.41
The all components of cognitive behavior therapy (CBT) suitable for elderly people may not be appropriate for individuals with dementia. However, the patients with dementia can learn and develop skills till later stage of dementia,42 which suggests that CBT could be used for patients with dementia as it has been done with other patients with intellectual disabilities. The CBT programs can be simplified: using basic principles such as distraction and relaxation may be sufficient, rather than focusing on in-depth therapy, which may be impossible because of difficulties in communication and cognition.42
Studies on CBT in older adults have focused largely on treating GAD, panic disorder, subjective worry and/or agoraphobia. From studies of CBT for elderly patients with anxiety, highly significant effect size (0.55) was reported.43 Recent randomized control study for dementia patients showed anxiety was significantly lower in the CBT group at 15 weeks (-4.32, 95% CI -8.21 to -0.43). However, when adjusted for baseline anxiety and cognition, this just fell short of statistical significance (-3.10, 95% CI -6.55 to 0.34).44 Though, these studies showed conflict results, CBT may be an option for elderly patients with anxiety comorbid with mild dementia or in the immediate after a diagnosis of dementia.
In summary, there is evidence that behavioral interventions and CBT are beneficial for anxiety or anxiety associated with agitation. However, further research is required in identifying specific psychosocial interventions targeting anxiety in people with dementia.
There is no well randomized clinical studies exploring drug treatment of anxiety in patients with dementia. Consequently, treatment strategies have to be largely extrapolated from studies conducted in younger anxiety patients without dementia, and considered drug pharmacokinetics, pharmacodynamics of elderly peoples.
The medication use should be based on the severity and duration of symptoms, comorbid conditions, concurrent medications and response to treatments in the past. These guidelines draw on the National Institute for Health and Clinical Excellence recommendations regarding the provision of psychological treatments by suitably trained staff (National Collaborating Centre for Mental Health, 2011) which not comment on this population. This lack of evidence-based manual is a significant problem in dementia care.
Benzodiazepines are associated with tolerance, dependence and a withdrawal syndrome that can aggravate cognitive dysfunction or BPSD. A short half-life (e.g., lorazepam) benzodiazepines are eliminated much more quickly than those with a long half-life (e.g., diazepam or alprazolam) and therefore may cause fewer problems of accumulation and consequent toxicity. However, short acting benzodiazepines are more likely to produce withdrawal symptoms and induce dependence. In dementia with Lewy bodies, clonazepam may be a first-line choice for the management of anxiety and associated behavioral problems. The British Association for Psychopharmacology guidelines report evidence in support of the use of diazepam and alprazolam in acute anxiety, but warn about the adverse effects.45
The advantage of using diazepam in older adults is less risk of dependence but, like all benzodiazepines, they may cause adverse effects in this population. They may contribute to respiratory insufficiency in patients with pulmonary disorders, and they potentiate the effects of alcohol and opioids. Benzodiazepine use in older people is associated with falls,46 and cognitive impairment.47 Benzodiazepine withdrawal delirium occurs most frequently in older people, giving rise to an increased rate of neuropsychiatric complications. Distressing discontinuation symptoms occur in as many as 90% of older patients who have been taking low daily doses. Symptoms such as irritability or restlessness are common. Psychosis, seizures and delirium, although uncommon, can last for 2–4 weeks.
Therefore, use of benzodiazepines in elderly patients with dementia has to be determined according to the individual basis, taking into account comorbid physical illnesses, concurrent medications, the risks of treating vs. not treating, potential benefits of treatment and whether other psychosocial interventions could be successfully provided. Benzodiazepines have to be used with caution, at the lowest effective dose for the shortest period of time.
Depression commonly present with anxiety. A review of pharmacological treatments for neuropsychiatric symptoms in dementia reported that, of the antidepressants, citalopram was the one to be of benefit. It produced a 10-point reduction in the Neurobehavioural Rating Scale, with agitation and liability showing significant improvement compared with placebo.48 In a pooled analysis of five randomized controlled trials, venlafaxine was studied for GAD in adults (n=1839).49 In the subpopulation of patients aged over 60 (10% of the original sample), venlafaxine was superior to placebo, with benefits seen at 8 and 24 weeks and with an adverse effect profile no different from that of placebo. However, this study did not subanalyze the study population with cognitive impairment.
No published trials have specifically studied the use of acetylcholinesterase inhibitors to manage anxiety in dementia. There have been secondary analyses of specific symptoms on the NPI responding to cholinesterase inhibitors. Acetylcholinesterase inhibitors have been shown to be effective in treating depression, dysphoria, anxiety and apathy. They may also reduce aggression and agitation.50 Conversely, cholinesterase inhibitors may lead to increases in anxiety-like and pro depressive behavior in animal study.
Nevertheless, these medications do show benefit in treating cognitive symptoms of dementia and they are safer than antipsychotics.51 A rational approach might be to try them after or together with psychosocial interventions if behavioral disturbances are secondary to anxiety or anxiety is the predominant neuropsychiatric symptom. Though, one post marketing survey showed the 52% reduction of anxiety after memantine medication,52 there is no randomized control trials in this class of drugs.
In a 3-month, open-labelled study of risperidone involving 15 elderly patients with anxiety disorder who had failed to show a therapeutic response to antidepressant and benzodiazepine treatment, Moríñigo et al.53 report of a response in 13 patients. Quetiapine has been effective as an add on to selective serotonin reuptake inhibitos or venlafaxine in a study of anxiety comorbid with depression in 58 adults.54 However, careful application should be needed in extrapolating these findings to the management of anxiety in dementia, because of the risk of adverse effects (including sedation and cerebrovascular events) in older people.55
A antipsychotics should be used only in very special circumstances for the management of anxiety in dementia (e.g., severe, intractable anxiety that results in great distress to the patient or produces severe behavioral disturbance).
Go to : 
In patients with dementia, anxiety is a very common symptom, and this may be manifested as a various mental and physical symptoms. This can not only worsen the symptoms of dementia itself, but it can also have an adverse effects on the caregiver. However, though anxiety is a important factor to be considered in the treatment of dementia, there is little research on it compared to other behavioral psychological symptoms of dementia. The most important reason for this is that it is not easy to distinguish between anxiety in dementia and dementia itself or depression in dementia. Therefore, it is necessary to study more appropriate epidemiology, pathophysiology and treatment through development of diagnostic criteria and screening tools suitable for anxiety in dementia patients.
Finally, though studies have shown that anxiety is associated with brain lesions related with dementia pathology, but it should be kept in mind that elderly patients with dementia may have faced apparent ontological anxiety. By looking the process of being transformed into a being that should depend on others from being that is independent existence, patients may feel the ontological crisis and anxiety. Obviously, these patients may require adequate medication if symptom are severe enough, but underling ontological anxiety should not be overlooked and non-pharmacological psychosocial interventions should be considered as an important treatment options for anxiety in dementia.
Go to : 
References
1. Shankar KK, Orrell MW. Detecting and managing depression and anxiety in people with dementia. Curr Opin Psychiatry. 2000; 13:55–59.

2. Porter VR, Buxton WG, Fairbanks LA, Strickland T, O'Connor SM, Rosenberg-Thompson S, et al. Frequency and characteristics of anxiety among patients with Alzheimer's disease and related dementias. J Neuropsychiatry Clin Neurosci. 2003; 15:180–186. PMID: 12724459.

3. Lyketsos CG, Steinberg M, Tschanz JT, Norton MC, Steffens DC, Breitner JC. Mental and behavioral disturbances in dementia: findings from the Cache County study on memory in aging. Am J Psychiatry. 2000; 157:708–714. PMID: 10784462.

4. Gibbons LE, Teri L, Logsdon R, McCurry SM, Kukull W, Bowen J, et al. Anxiety symptoms as predictors of nursing home placement in patients with Alzheimer's disease. J Clin Geropsychol. 2002; 8:335–342.
5. Beekman AT, Bremmer MA, Deeg DJ, van Balkom AJ, Smit JH, de Beurs E, et al. Anxiety disorders in later life: a report from the longitudinal aging study Amsterdam. Int J Geriatr Psychiatry. 1998; 13:717–726. PMID: 9818308.

6. Ballard C, Neill D, O'Brien J, McKeith IG, Ince P, Perry R. Anxiety, depression and psychosis in vascular dementia: prevalence and associations. J Affect Disord. 2000; 59:97–106. PMID: 10837878.

7. Mendez MF, McMurtray A, Chen AK, Shapira JS, Mishkin F, Miller BL. Functional neuroimaging and presenting psychiatric features in frontotemporal dementia. J Neurol Neurosurg Psychiatry. 2006; 77:4–7. PMID: 16043457.

8. Chen JC, Borson S, Scanlan JM. Stage-specific prevalence of behavioral symptoms in Alzheimer's disease in a multi-ethnic community sample. Am J Geriatr Psychiatry. 2000; 8:123–133. PMID: 10804073.

9. Aarsland D, Cummings JL, Larsen JP. Neuropsychiatric differences between Parkinson's disease with dementia and Alzheimer's disease. Int J Geriatr Psychiatry. 2001; 16:184–191. PMID: 11241724.

10. Seignourel PJ, Kunik ME, Snow L, Wilson N, Stanley M. Anxiety in dementia: a critical review. Clin Psychol Rev. 2008; 28:1071–1082. PMID: 18555569.

11. Tanaka H, Hashimoto M, Fukuhara R, Ishikawa T, Yatabe Y, Kaneda K, et al. Relationship between dementia severity and behavioural and psychological symptoms in early-onset Alzheimer's disease. Psychogeriatrics. 2015; 15:242–247. PMID: 25737233.

12. Kwak YT, Yang YS, Kwak SG. Clinical characteristics of behavioral and psychological symptoms in patients with drug-naïve Alzheimer's disease. Dement Neurocogn Disorder. 2012; 11:87–94.

13. Brodaty H, Connors MH, Xu J, Woodward M, Ames D. PRIME study group. The course of neuropsychiatric symptoms in dementia: a 3-year longitudinal study. J Am Med Dir Assoc. 2015; 16:380–387. PMID: 25687925.

14. McClive-Reed KP, Gellis ZD. Anxiety and related symptoms in older persons with dementia: directions for practice. J Gerontol Soc Work. 2011; 54:6–28. PMID: 21170777.

15. Starkstein SE, Jorge R, Petracca G, Robinson RG. The construct of generalized anxiety disorder in Alzheimer disease. Am J Geriatr Psychiatry. 2007; 15:42–49. PMID: 17194814.

16. Neville C, Teri L. Anxiety, anxiety symptoms, and associations among older people with dementia in assisted-living facilities. Int J Ment Health Nurs. 2011; 20:195–201. PMID: 21492359.

17. Bergh S, Selbæk G. The prevalence and the course of neuropsychiatric symptoms in patients with dementia. Nor Epidemiol. 2012; 22:225–232.

18. Bierman EJ, Comijs HC, Jonker C, Beekman AT. Symptoms of anxiety and depression in the course of cognitive decline. Dement Geriatr Cogn Disord. 2007; 24:213–219. PMID: 17690554.

19. Calleo J, Stanley M. Anxiety disorders in later life: differentiated diagnosis and treatment strategies. Psychiatr Times. 2008; 25:24–27.
20. Calleo JS, Kunik ME, Reid D, Kraus-Schuman C, Paukert A, Regev T, et al. Characteristics of generalized anxiety disorder in patients with dementia. Am J Alzheimers Dis Other Demen. 2011; 26:492–497. PMID: 22062223.

21. Rozzini L, Chilovi BV, Peli M, Conti M, Rozzini R, Trabucchi M, et al. Anxiety symptoms in mild cognitive impairment. Int J Geriatr Psychiatry. 2009; 24:300–305. PMID: 18759379.

22. Bierman EJ, Comijs HC, Jonker C, Scheltens P, Beekman AT. The effect of anxiety and depression on decline of memory function in Alzheimer's disease. Int Psychogeriatr. 2009; 21:1142–1147. PMID: 19615124.

23. Gallacher J, Bayer A, Fish M, Pickering J, Pedro S, Dunstan F, et al. Does anxiety affect risk of dementia? Findings from the Caerphilly prospective study. Psychosom Med. 2009; 71:659–666. PMID: 19553290.

24. Derouesné C, Rapin JR, Lacomblez L. [Memory complaints in 200 subjects meeting the diagnostic criteria for age-associated memory impairment: psychoaffective and cognitive correlates]. Psychol Neuropsychiatr Vieil. 2004; 2:67–74. PMID: 15683970.
25. Breitve MH, Hynninen MJ, Brønnick K, Chwiszczuk LJ, Auestad BH, Aarsland D, et al. A longitudinal study of anxiety and cognitive decline in dementia with Lewy bodies and Alzheimer's disease. Alzheimers Res Ther. 2016; 8:3. PMID: 26812908.

26. Somme J, Fernández-Martínez M, Molano A, Zarranz JJ. Neuropsychiatric symptoms in amnestic mild cognitive impairment: increased risk and faster progression to dementia. Curr Alzheimer Res. 2013; 10:86–94. PMID: 23016837.

27. Palmer K, Berger AK, Monastero R, Winblad B, Bäckman L, Fratiglioni L. Predictors of progression from mild cognitive impairment to Alzheimer disease. Neurology. 2007; 68:1596–1602. PMID: 17485646.

28. Rosenberg PB, Mielke MM, Appleby BS, Oh ES, Geda YE, Lyketsos CG. The association of neuropsychiatric symptoms in MCI with incident dementia and Alzheimer disease. Am J Geriatr Psychiatry. 2013; 21:685–695. PMID: 23567400.

29. Liu HC, Wang PN, Wang HC, Lin KN, Hong CJ, Liu CY, et al. Conversion to dementia from questionable dementia in an ethnic Chinese population. J Geriatr Psychiatry Neurol. 2007; 20:76–83. PMID: 17548776.

30. Brodaty H, Heffernan M, Draper B, Reppermund S, Kochan NA, Slavin MJ, et al. Neuropsychiatric symptoms in older people with and without cognitive impairment. J Alzheimers Dis. 2012; 31:411–420. PMID: 22571979.

31. Kessler RC, Gruber M, Hettema JM, Hwang I, Sampson N, Yonkers KA. Co-morbid major depression and generalized anxiety disorders in the national comorbidity survey follow-up. Psychol Med. 2008; 38:365–374. PMID: 18047766.

32. Reisberg B, Auer SR, Monteiro IM. Behavioral pathology in Alzheimer's disease (BEHAVE-AD) rating scale. Int Psychogeriatr. 1996; 8(Suppl 3):301–308. discussion 351-354. PMID: 9154579.

33. Cummings JL. The Neuropsychiatric Inventory: assessing psychopathology in dementia patients. Neurology. 1997; 48(5 Suppl 6):S10–S16.

34. Shankar KK, Walker M, Frost D, Orrell MW. The development of a valid and reliable scale for rating anxiety in dementia (RAID). Aging Ment Health. 1999; 3:39–49.

35. LaBarge E. A preliminary scale to measure the degree of worry among mildly demented Alzheimer disease patients. Phys Occup Ther Geriatr. 1993; 11:43–57.

36. James I. Using a cognitive rationale to conceptualize anxiety in people with dementia. Behav Cogn Psychother. 1999; 27:345–351.

37. Boot BP, Orr CF, Ahlskog JE, Ferman TJ, Roberts R, Pankratz VS, et al. Risk factors for dementia with Lewy bodies: a case-control study. Neurology. 2013; 81:833–840. PMID: 23892702.

38. Mah L, Binns MA, Steffens DC. Alzheimer's Disease Neuroimaging Initiative. Anxiety symptoms in amnestic mild cognitive impairment are associated with medial temporal atrophy and predict conversion to Alzheimer disease. Am J Geriatr Psychiatry. 2015; 23:466–476. PMID: 25500120.

39. Green KN, Billings LM, Roozendaal B, McGaugh JL, LaFerla FM. Glucocorticoids increase amyloid-beta and tau pathology in a mouse model of Alzheimer's disease. J Neurosci. 2006; 26:9047–9056. PMID: 16943563.

40. Erickson K, Drevets W, Schulkin J. Glucocorticoid regulation of diverse cognitive functions in normal and pathological emotional states. Neurosci Biobehav Rev. 2003; 27:233–246. PMID: 12788335.

41. Ramakers IH, Verhey FR, Scheltens P, Hampel H, Soininen H, Aalten P, et al. Anxiety is related to Alzheimer cerebrospinal fluid markers in subjects with mild cognitive impairment. Psychol Med. 2013; 43:911–920. PMID: 22954311.

42. Spector A, Thorgrimsen L, Woods B, Royan L, Davies S, Butterworth M, et al. Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial. Br J Psychiatry. 2003; 183:248–254. PMID: 12948999.
43. Nordhus IH, Pallesen S. Psychological treatment of late-life anxiety: an empirical review. J Consult Clin Psychol. 2003; 71:643–651. PMID: 12924668.

44. Spector A, Charlesworth G, King M, Lattimer M, Sadek S, Marston L, et al. Cognitive-behavioural therapy for anxiety in dementia: pilot randomised controlled trial. Br J Psychiatry. 2015; 206:509–516. PMID: 25698766.

45. Baldwin DS, Anderson IM, Nutt DJ, Bandelow B, Bond A, Davidson JR, et al. Evidence-based guidelines for the pharmacological treatment of anxiety disorders: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2005; 19:567–596. PMID: 16272179.

46. Neutel CI, Hirdes JP, Maxwell CJ, Patten SB. New evidence on benzodiazepine use and falls: the time factor. Age Ageing. 1996; 25:273–278. PMID: 8831871.

47. Foy A, O'Connell D, Henry D, Kelly J, Cocking S, Halliday J. Benzodiazepine use as a cause of cognitive impairment in elderly hospital inpatients. J Gerontol A Biol Sci Med Sci. 1995; 50:M99–M106. PMID: 7874596.

48. Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA. 2005; 293:596–608. PMID: 15687315.
49. Katz IR, Reynolds CF 3rd, Alexopoulos GS, Hackett D. Venlafaxine ER as a treatment for generalized anxiety disorder in older adults: pooled analysis of five randomized placebo-controlled clinical trials. J Am Geriatr Soc. 2002; 50:18–25. PMID: 12028242.

50. Gauthier S, Feldman H, Hecker J, Vellas B, Ames D, Subbiah P, et al. Efficacy of donepezil on behavioral symptoms in patients with moderate to severe Alzheimer's disease. Int Psychogeriatr. 2002; 14:389–404. PMID: 12670060.
51. National Collaborating Centre for Mental Health, National Collaborating Centre for Primary Care. Generalised anxiety disorder and panic disorder (with or without agoraphobia) in adults: management in primary, secondary and community care (NICE clinical guideline 113). London: National Institute for Health and Clinical Excellence;2011.
52. Clerici F, Vanacore N, Elia A, Spila-Alegiani S, Pomati S, Da Cas R, et al. Memantine effects on behaviour in moderately severe to severe Alzheimer's disease: a post-marketing surveillance study. Neurol Sci. 2012; 33:23–31. PMID: 21584738.

53. Moríñigo A, Blanco M, Labrador J, Martín J, Noval D. Risperidone for resistant anxiety in elderly persons. Am J Geriatr Psychiatry. 2005; 13:81–82.

54. McIntyre A, Gendron A, McIntyre A. Quetiapine adjunct to selective serotonin reuptake inhibitors or venlafaxine in patients with major depression, comorbid anxiety, and residual depressive symptoms: a randomized, placebo-controlled pilot study. Depress Anxiety. 2007; 24:487–494. PMID: 17177199.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download