2. Paul M, Andreassen S, Tacconelli E, Nielsen AD, Almanasreh N, Frank U, et al. Improving empirical antibiotic treatment using TREAT, a computerized decision support system: cluster randomized trial. J Antimicrob Chemother. 2006; 58(6):1238–1245.


3. Fridkin SK, Steward CD, Edwards JR, Pryor ER, McGowan JE Jr, Archibald LK, et al. Surveillance of antimicrobial use and antimicrobial resistance in United States hospitals: project ICARE phase 2. Project Intensive Care Antimicrobial Resistance Epidemiology (ICARE) hospitals. Clin Infect Dis. 1999; 29(2):245–252.

4. Shlaes DM, Gerding DN, John JF Jr, Craig WA, Bornstein DL, Duncan RA, et al. Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis. 1997; 25(3):584–599.


5. McDanel J, Schweizer M, Crabb V, Nelson R, Samore M, Khader K, et al. Incidence of extended-spectrum β-lactamase (ESBL)-producing
Escherichia coli and
Klebsiella infections in the United States: a systematic literature review. Infect Control Hosp Epidemiol. 2017; 38(10):1209–1215.

6. Chang YT, Coombs G, Ling T, Balaji V, Rodrigues C, Mikamo H, et al. Epidemiology and trends in the antibiotic susceptibilities of Gram-negative bacilli isolated from patients with intra-abdominal infections in the Asia-Pacific region, 2010–2013. Int J Antimicrob Agents. 2017; 49(6):734–739.


7. Thaden JT, Fowler VG, Sexton DJ, Anderson DJ. Increasing incidence of extended-spectrum β-lactamase-producing
Escherichia coli in community hospitals throughout the southeastern United States. Infect Control Hosp Epidemiol. 2016; 37(1):49–54.

8. Kim YA, Kim JJ, Kim H, Lee K. Community-onset extended-spectrum-β-lactamase-producing
Escherichia coli sequence type 131 at two Korean community hospitals: the spread of multidrug-resistant
E. coli to the community via healthcare facilities. Int J Infect Dis. 2017; 54:39–42.

9. Logan LK, Weinstein RA. The epidemiology of carbapenem-resistant Enterobacteriaceae: the impact and evolution of a global menace. J Infect Dis. 2017; 215:suppl_1. S28–S36.
10. Muggeo A, Guillard T, Barbe C, Thierry A, Bajolet O, Vernet-Garnier V, et al. Factors associated with carriage of carbapenem-non-susceptible Enterobacteriaceaein North-Eastern France and outcomes of infected patients. J Antimicrob Chemother. 2017; 72(5):1496–1501.

11. Morrill HJ, Pogue JM, Kaye KS, LaPlante KL. Treatment options for carbapenem-resistant
Enterobacteriaceae infections. Open Forum Infect Dis. 2015; 2(2):ofv050.

12. Kim M, Song KH, Kim CJ, Song M, Choe PG, Park WB, et al. Electronic alerts with automated consultations promote appropriate antimicrobial prescriptions. PLoS One. 2016; 11(8):e0160551.

13. Hendrik TC, Voor In 't Holt AF, Vos MC. Clinical and molecular epidemiology of extended-spectrum beta-lactamase-producing Klebsiella spp.: a systematic review and meta-analyses. PLoS One. 2015; 10(10):e0140754.
15. Falcone M, Russo A, Giannella M, Cangemi R, Scarpellini MG, Bertazzoni G, et al. Individualizing risk of multidrug-resistant pathogens in community-onset pneumonia. PLoS One. 2015; 10(4):e0119528.

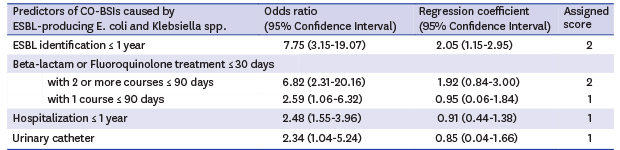
16. Augustine MR, Testerman TL, Justo JA, Bookstaver PB, Kohn J, Albrecht H, et al. Clinical risk score for prediction of extended-spectrum β-lactamase-producing
Enterobacteriaceae in bloodstream isolates. Infect Control Hosp Epidemiol. 2017; 38(3):266–272.

17. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383.


18. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004; 57(12):1288–1294.


19. Paterson DL, Ko WC, Von Gottberg A, Mohapatra S, Casellas JM, Goossens H, et al. International prospective study of
Klebsiella pneumoniae bacteremia: implications of extended-spectrum beta-lactamase production in nosocomial infections. Ann Intern Med. 2004; 140(1):26–32.

20. Tu JV, Naylor CD. Clinical prediction rules. J Clin Epidemiol. 1997; 50(6):743–744.


21. Harrell F. Regression coefficients and scoring rules. J Clin Epidemiol. 1996; 49(7):819.

22. Moons KG, Harrell FE, Steyerberg EW. Should scoring rules be based on odds ratios or regression coefficients? J Clin Epidemiol. 2002; 55(10):1054–1055.


23. Blot S, Vandewoude K, De Bacquer D, Colardyn F. Nosocomial bacteremia caused by antibiotic-resistant gram-negative bacteria in critically ill patients: clinical outcome and length of hospitalization. Clin Infect Dis. 2002; 34(12):1600–1606.


25. Van Aken S, Lund N, Ahl J, Odenholt I, Tham J. Risk factors, outcome and impact of empirical antimicrobial treatment in extended-spectrum β-lactamase-producing
Escherichia coli bacteraemia. Scand J Infect Dis. 2014; 46(11):753–762.

26. Denis B, Lafaurie M, Donay JL, Fontaine JP, Oksenhendler E, Raffoux E, et al. Prevalence, risk factors, and impact on clinical outcome of extended-spectrum beta-lactamase-producing Escherichia coli bacteraemia: a five-year study. Int J Infect Dis. 2015; 39:1–6.
27. Titelman E, Hasan CM, Iversen A, Nauclér P, Kais M, Kalin M, et al. Faecal carriage of extended-spectrum β-lactamase-producing Enterobacteriaceae is common 12 months after infection and is related to strain factors. Clin Microbiol Infect. 2014; 20(8):O508–O515.
28. Bar-Yoseph H, Hussein K, Braun E, Paul M. Natural history and decolonization strategies for ESBL/carbapenem-resistant Enterobacteriaceae carriage: systematic review and meta-analysis. J Antimicrob Chemother. 2016; 71(10):2729–2739.
29. Rottier WC, Ammerlaan HS, Bonten MJ. Effects of confounders and intermediates on the association of bacteraemia caused by extended-spectrum β-lactamase-producing
Enterobacteriaceae and patient outcome: a meta-analysis. J Antimicrob Chemother. 2012; 67(6):1311–1320.

30. Yokota PK, Marra AR, Martino MD, Victor ES, Durão MS, Edmond MB, et al. Impact of appropriate antimicrobial therapy for patients with severe sepsis and septic shock--a quality improvement study. PLoS One. 2014; 9(11):e104475.







 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download