Abstract
Purpose
To evaluate contrast sensitivity in patients with Behçet's disease (BD) without ocular involvement.
Methods
The study group was composed of 47 BD patients (20 to 50 years of age) who did not have ocular involvement. The control group was composed of 47 normal volunteers who were similar to the study group in terms of age and gender. No participants in this study had any ocular or systemic pathologies except for BD. The contrast sensitivity measurements were performed using the Functional Acuity Contrast Test under photopic conditions, and the results were compared between the two groups.
Results
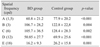
The mean age of the BD patients and control subjects was 34.5 ± 9.7 and 33.2 ± 7.6 years, respectively. The mean disease duration of the BD patients was 5.5 ± 6.4 years. There was a statistically significant decrease at five spatial frequencies (A, 1.5; B, 3; C, 6; D, 2; and E, 18 cycles per degree) in patients with BD compared with control subjects (p < 0.001, p = 0.004, p = 0.002, p < 0.001, and p = 0.001, respectively).
Behçet's disease (BD) is a systemic disease characterized by recurrent aphthous ulcers, vasculitis, and intraocular inflammation [12]. According to the International Study Group for Behçet's Disease, the diagnostic criteria of BD are recurrent oral ulcerations and at least two of the following: recurrent genital ulcers, ocular lesions, skin lesions, or a positive pathergy test [23].
Although the etiology of BD is unknown, genetic and environmental factors are involved [4]. BD mainly occurs in a region known historically as the Silk Road [5]. The prevalence of BD is 2 to 30 per 100,000 in Asian countries, and 0.1 to 7.5 per 100,000 in America and European countries [2].
Previous studies have reported that ocular involvement occurs in 23% to 96% of BD patients [678]. Although ocular involvement may be the initial symptom, it usually occurs in the second or third year of the disease [78] and is generally in the form of panuveitis and retinal vasculitis [8].
Contrast sensitivity (CS) tests measure the ability of the patient to visualize small, medium, and large symbols in different contrast conditions [910]. These tests assess aspects of vision that cannot be evaluated by visual acuity tests [11]. Visual function and early forms of eye disease can be investigated with CS tests [12]. Impairment of CS has been reported in many eye diseases and neurological disorders. Glaucoma, cataract, corneal edema, keratoconus, amblyopia, macular diseases, retinitis pigmentosa, diabetic retinopathy, optic neuropathies, Parkinson's disease, and Alzheimer's disease have been reported to reduce CS [131415]. In this study, we aimed to evaluate CS in patients with BD without ocular involvement.
The participants included in this prospective study were divided into two groups. The study group was composed of 47 patients (20 to 50 years of age) with BD who did not have ocular involvement. The control group was composed of 47 healthy volunteers who were similar to the study group in terms of age and sex distributions. A written informed consent was obtained from all participants before the study, and the tenets of the Declaration of Helsinki were followed. The study protocol was approved by Malatya Clinical Research Ethical Committee (2015/192).
A complete ophthalmic examination of all participants was performed by the same ophthalmologist. First, the best spectacle-corrected visual acuity was evaluated using the Snellen chart, and individuals with incomplete vision were excluded from the study. Biomicroscopic examinations, intraocular pressure measurements, and fundus examinations were performed on patients who had a bilateral visual acuity of 20 / 20.
Individuals with any ocular or systemic pathology that could possibly affect CS test results, such as high myopia, corneal scar, cataract, glaucoma, diabetic or hypertensive retinopathy, uveitis, maculopathy, history of past ocular surgery or trauma, and optic neuritis, and patients who had used systemic drugs (except for colchicine) to treat BD during the last 3 months were excluded from the study. Refractive errors, when present, were <±1.00 diopters and were fully corrected during the CS testing. Spectral domain optical coherence tomography (SD-OCT) imaging was performed on the eyes of all participants. Two patients with BD showed deterioration of the junction between the inner and outer segments of the photoreceptor on OCT (Nidek, Fremont, CA, USA) imaging and were excluded from the study. The CS test was performed with a binocular view in all cases. Information about the test was presented to the participants before testing.
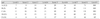
Measurements were performed with the Functional Acuity Contrast Test (FACT; Stereo Optical, Chicago, IL, USA) under photopic conditions. The FACT consists of light and dark colored bands called sinusoidal gratings. The panel contained 1.5, 3, 6, 12, and 18 cycles per degree (cpd) grating examples in five spatial frequencies from bottom to top. There were nine sinusoidal gratings for which the contrast decreased logarithmically from left to right. The contrast values of each sinusoidal grating, according to spatial frequency in the FACT, are shown in Table 1.
The eyes of all participants were evaluated at five spatial frequencies (A, 1.5; B, 3; C, 6; D, 12; and E, 18 cpd). After measurements were performed at all five frequencies, the average contrast values of each grating were recorded according to spatial frequency.
IBM SPSS Statistics ver. 20 (IBM Corp., Armonk, NY, USA) was used for the analysis. According to the power analysis, at least 46 participants were required in each group. The non-parametric Mann-Whitney U-test was used to compare the data of the two groups, because the variables measured by the CS test did not have a normal distribution according to the results of the Kolmogorov-Smirnov test. A p-value <0.05 was considered to be significant.
The study comprised 47 patients with BD and 47 control individuals. The demographic characteristics of the BD patients and control individuals are presented in Table 2. There were no statistically significant differences in mean age and sex between the BD and control groups.
The mean disease duration of the BD patients was 5.5 ± 6.4 years. In both groups, each individual's best spectacle-corrected bilateral visual acuity, which was measured by the Snellen chart, was 20 / 20 in all measurements. Intraocular pressure, biomicroscopic and funduscopic examinations were normal in both groups.
The mean CS measurements of BD group were statistically significantly lower than those of control group at five spatial frequencies (A, 1.5; B, 3; C, 6; D, 12; and E, 18 cpd) (p < 0.05) (Table 3 and Fig. 1). The BD group was subdivided into the following age groups: 20 to 29, 30 to 39, and 40 to 50 years. These three subgroups included 17, 14, and 16 patients, respectively. There was no statistically significant difference in CS between the subgroups (p > 0.05) (Table 4).
BD is a multisystemic clinical disorder that is most common in the geographical ancient Silk Road region, which includes Turkey. Ocular involvement, which is one of the three most common manifestations in BD, usually emerges two or three years after diagnosis [127]. The CS test assesses the patient's ability to see lower contrast patterns and provides more reliable information about visual function than the visual acuity test [916]. In our study, CS was determined in 47 BD patients with no ocular involvement and optimal visual acuity (20 / 20). In our literature review, we were unable to find any previous report of CS in BD patients.
BD vasculitis can affect large and small arterial or venous vessels [8]. BD can lead to very different clinical outcomes, and diagnosis may be difficult. Some studies have reported that BD affects the choroid [171819], and it has also been reported that the findings of indocyanine green angiography of the choroidal vessels may be affected in BD patients [1718]. Coskun et al. [19] reported a decrease in choroidal thickness on enhanced SD-OCT in BD patients. BD can affect the nutrient supply to the photoreceptors and cause photoreceptor damage via its effects on the choroidal vessels [819]. In our study, SD-OCT images were obtained for all participants. Two patients in the BD group were excluded from the study because of deterioration of the junction between the inner and outer segments of the photoreceptor. No other pathology was noted on the SD-OCT images.
Ocular BD generally present as panuveitis or retinal vasculitis. Posterior segment involvement can lead to permanent anatomical changes and loss of vision. The occurrence of posterior segment involvement has been reported in 50% to 93% of the ocular Behçet population [2]. The BD patients included in our study had no ocular involvement. Thus, the decrease in CS determined in our study was not associated with ocular BD.
Neurological involvement is seen in 5% to 30% of BD patients and is referred to as neuro-Behçet disease (NBD) [2021]. NBD can take either a parenchymal or non-parenchymal form. The non-parenchymal form is more commonly associated with major cranial vascular involvement, while the parenchymal form involves the brain stem and spinal cord, hemispheric atrophy, and a meningoencephalitic presentation [2022]. In parenchymal NBD, pyramidal symptoms are seen in 96% of patients, and behavioral changes are observed in half of all patients [23]. Brain stem and hemispheric atrophy was observed in imaging studies performed for early detection of NBD in BD patients with no neurological involvement [22]. The decrease in CS detected in our study may be due to cranial parenchymal involvement. We think that our results indicate subclinical neural involvement in BD patients without ocular involvement. The lack of radiological examinations to support this idea is a limitation of our study.
In diabetic patients, CS decreases progressively with severity of diabetic retinopathy, but a significant proportion of diabetic patients with no signs of diabetic retinopathy also experience a decrease in CS, even some of those with normal Snellen visual acuity. These early changes in CS in diabetic patients can be indications of early-stage diabetic retinopathy or visual dysfunction [242526]. Similarly, the prevalence of reduced CS in human immunodeficiency virus-infected individuals without retinal disease is two to three times greater than in the normal population. These changes in CS may be caused by retinal microvasculopathy of human immunodeficiency virus disease [27]. Diabetes mellitus and acquired immunodeficiency syndrome are systemic diseases, as is BD. The decreases in CS in patients with diabetes mellitus or acquired immunodeficiency syndrome without ocular involvement support our idea of subclinical neural involvement in BD patients without ocular involvement.
Previous studies have reported that CS reached a maximum at approximately 20 years of age and decreased gradually after age 40 to 50 years [28]. In our study, the mean ages of the BD and control groups were similar (34.5 ± 9.7 and 33.2 ± 7.6 years, respectively). In addition, when the BD patients were divided into three subgroups according to age, there was no significant difference in CS. This may be due to the small number of cases in each group or to the upper age limit of 50 years. We set the upper age limit at 50 years to avoid advanced age-related CS reductions. If this study protocol was applied to a population with a younger upper age limit, it could be more valuable, but we could not reduce the upper age limit in this study due to the small number of patients. This is another limitation of our study.
Although the major effects of refraction on CS occur mainly at high spatial frequencies, it has some affect at all frequencies [29]. Also, a decrease in CS may occur in conjunction with a decrease in visual acuity due to refractive errors. The current study included individuals with low refractive errors (<±1.00 diopters) and a visual acuity of 20 / 20 to prevent any effects on the CS results.
Eye diseases, such as cataract and glaucoma, may affect CS. Cataract is the most common cause of decreased CS in middle-aged and elderly individuals [30]. Our study did not include individuals with cataract or glaucoma to avoid any effects of these diseases on the results of CS testing.
In conclusion, measurements performed with the FACT revealed a statistically significantly lower CS in BD patients without ocular involvement, at all spatial frequencies, compared with control individuals. This finding may indicate subclinical neural involvement in BD patients without ocular involvement. More valuable results could have been obtained if the study had been performed in a younger population and had included larger numbers of patients and radiological examinations. Future studies with these features will provide more information about the CS of BD patients without ocular involvement.
Figures and Tables
Fig. 1
The contrast sensitivity of the groups at five spatial frequencies. BD = Behçet's disease; cpd = cycles per degree.
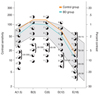
Table 1
The contrast values corresponding to each grating according to spatial frequencies in the Functional Acuity Contrast Test panel
Notes
References
2. Al-Dhibi H, Abouammoh M, Al-Harthi E, et al. Macular hole in Behcet's disease. Indian J Ophthalmol. 2011; 59:359–362.
3. Criteria for diagnosis of Behcet's disease. International Study Group for Behcet's Disease. Lancet. 1990; 335:1078–1080.

4. A SE, Moses PD, George R. Ocular manifestations of Behcet's disease. Indian Pediatr. 2005; 42:942–945.

5. Borhani Haghighi A, Sharifzad HR, Matin S, Rezaee S. The pathological presentations of neuro-Behcet disease: a case report and review of the literature. Neurologist. 2007; 13:209–214.

6. Saylan T, Mat C, Fresko I, Melikoglu M. Behcet's disease in the Middle East. Clin Dermatol. 1999; 17:209–223.

7. Yazici H, Fresko I, Yurdakul S. Behcet's syndrome: disease manifestations, management, and advances in treatment. Nat Clin Pract Rheumatol. 2007; 3:148–155.
8. Yuksel H, Turkcu FM, Sahin M, et al. Inner and outer segment junction (IS/OS line) integrity in ocular Behcet's disease. Arq Bras Oftalmol. 2014; 77:219–221.

9. Arden GB. The importance of measuring contrast sensitivity in cases of visual disturbance. Br J Ophthalmol. 1978; 62:198–209.



10. Olsen T, Corydon L. Contrast sensitivity as a function of focus in patients with the diffractive multifocal intraocular lens. J Cataract Refract Surg. 1990; 16:703–706.


11. Ginsburg AP. Contrast sensitivity: determining the visual quality and function of cataract, intraocular lenses and refractive surgery. Curr Opin Ophthalmol. 2006; 17:19–26.

12. Loshin DS, White J. Contrast sensitivity: the visual rehabilitation of the patient with macular degeneration. Arch Ophthalmol. 1984; 102:1303–1306.

13. Trick GL, Burde RM, Gordon MO, et al. The relationship between hue discrimination and contrast sensitivity deficits in patients with diabetes mellitus. Ophthalmology. 1988; 95:693–698.


14. Marmor MF. Contrast sensitivity versus visual acuity in retinal disease. Br J Ophthalmol. 1986; 70:553–559.



15. Ridder A, Muller ML, Kotagal V, et al. Impaired contrast sensitivity is associated with more severe cognitive impairment in Parkinson disease. Parkinsonism Relat Disord. 2017; 34:15–19.


16. Preti RC, Ramirez LM, Monteiro ML, et al. Contrast sensitivity evaluation in high risk proliferative diabetic retinopathy treated with panretinal photocoagulation associated or not with intravitreal bevacizumab injections: a randomised clinical trial. Br J Ophthalmol. 2013; 97:885–889.


17. Klaeger A, Tran VT, Hiroz CA, et al. Indocyanine green angiography in Behcet's uveitis. Retina. 2000; 20:309–314.


18. Gedik S, Akova Y, Yilmaz G, Bozbeyoglu S. Indocyanine green and fundus fluorescein angiographic findings in patients with active ocular Behcet's disease. Ocul Immunol Inflamm. 2005; 13:51–58.

19. Coskun E, Gurler B, Pehlivan Y, et al. Enhanced depth imaging optical coherence tomography findings in Behcet disease. Ocul Immunol Inflamm. 2013; 21:440–445.

20. Farahangiz S, Sarhadi S, Safari A, Borhani-Haghighi A. Magnetic resonance imaging findings and outcome of neuro-Behcet's disease: the predictive factors. Int J Rheum Dis. 2012; 15:e142–e149.
21. Borman P, Tuncay F, Kocaoglu S, et al. The subclinic autonomic dysfunction in patients with Behcet disease: an electrophysiological study. Clin Rheumatol. 2012; 31:41–47.

22. Hirohata S, Kikuchi H, Sawada T, et al. Retrospective analysis of long-term outcome of chronic progressive neurological manifestations in Behcet's disease. J Neurol Sci. 2015; 349:143–148.


23. van Ham C, Schrijvers D, De Picker L, et al. Neuropsychiatric features in Behcet's disease: a case report. Clin Neurol Neurosurg. 2014; 127:13–14.

24. Safi S, Rahimi A, Raeesi A, et al. Contrast sensitivity to spatial gratings in moderate and dim light conditions in patients with diabetes in the absence of diabetic retinopathy. BMJ Open Diabetes Res Care. 2017; 5:e000408.

25. Safi H, Safi S, Hafezi-Moghadam A, Ahmadieh H. Early detection of diabetic retinopathy. Surv Ophthalmol. 2018; 63:601–608.


26. Di Leo MA, Caputo S, Falsini B, et al. Nonselective loss of contrast sensitivity in visual system testing in early type I diabetes. Diabetes Care. 1992; 15:620–625.


27. Holland GN, Kappel PJ, Van Natta ML, et al. Association between abnormal contrast sensitivity and mortality among people with acquired immunodeficiency syndrome. Am J Ophthalmol. 2010; 149:807–816.



28. Owsley C, Sekuler R, Siemsen D. Contrast sensitivity throughout adulthood. Vision Res. 1983; 23:689–699.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download