Abstract
Purpose
The purpose of this study was to build and test a model outlining the factors related to nurses' patient safety management activities. The exogenous variables were personal factor, job factor and organizational support. The endogenous factors were safety-related recognition, patient safety culture and patient safety management activities.
Methods
A survey using a structured questionnaire was conducted among 500 nurses in Korea. The collected data were analyzed using PASW Statistics 18.0 and AMOS 20.0 programs.
Results
Personal factors, job factors, safety-related recognition, and patient safety culture significantly affected nurses' patient safety management activities.
Conclusion
These results suggest that patient safety accidents can be prevented by increasing the safety culture and safety related recognition. To improve the safety culture and safety related recognition, measures should be taken to reduce the turnover rate of career nurses and provide sufficient manpower allocation, education and policies.
Patient safety is the first common principle to all members of a hospital in providing health care, and should be a priority for all procedures in the hospital. Patient safety accident encompasses all types of errors, mistakes, and accidents occurring in a hospital, regardless of whether the patient was injured or not [1]. According to a report of the U.S. Institute of Medicine (IOM), 44,000~98,000 patients died at the end of 1999 due to errors during hospitalization, and it was revealed that death from safety accidents was a more frequent cause of death than death from breast cancer and AIDS [2]. Among the accidents occurring in Korean hospitals, 52.7% of accidents were caused by a lack of safety management, 42.1% were caused by neglect in management of medical equipments and facilities, and 5.2% were caused by negligence in medication management [3]. As disputes and damages from safety accidents increase, interest in patient safety has also risen. In addition, the accreditation for healthcare organization in Korea from 2004 has been the starting point to raising public interest in patient safety [4].
As the healthcare system has undergone dramatic changes, there has been an increase in opportunities to provide new advanced medical services, as well as increased medical accidents [5]. Despite the evolution of innovative medical technologies, medical services are bound to depend on human intervention. Nurses are the medical care personnel most engaged in direct intervention for patients. As the area of nurse's practice expands, the responsibilities of nurses are also increasing.
Nurses' Patient Safety Management Activities (PSMA) include precise patient check, fall preventive activity, adequate explanation, infection preventive activity, high-risk drug management, precise operation/surgery check, communication between medical personnel, fire fighting safety, medical instrument management, prevention of pressure ulcers, transfusion nursing, and emergency management [6]. The factors affecting PSMA can be classified into sociodemographic characteristics, job factors, organizational support, safety accident awareness, and patient safety culture [3456]. The sociodemographic characteristics related to PSMA as revealed in previous studies were position, education level, age, and work experience [5]. Job factors that affect PSMA include job demand [7]. PSMA was reported to be related to organizational support such as the attitude of management [6] and staffing [4]. In addition, factors affecting PSMA are patient safety culture [8] and safety-specific cognition factors such as safety control, safety-related recognition, leadership, and safety perception [9].
Although studies on the factors affecting PSMA in medical and nursing sites have been carried out, they analyzed correlations with related factors or direct effects only. Studies on model establishments comprehensively looking at direct/indirect effects including all those factors are lacking [9]. Therefore this study was done to identify the direct/indirect factors by classifying the cause variables into personal factors, job factors, and organizational support. Through this study various factors affecting nurses' PSMA were comprehensively identified and the effects of relevant factors on nurses' PSMA were validated using a structural model. Such an exploration will provide useful data to strengthen nurses' PSMA and contribute to the improvement of quality of nursing care.
This study's conceptual framework was based on the Health Promotion Model of Pender [10] and System Engineering Initiative for Patient Safety (SEIPS) Model of P Carayon et al. [11]. The Health Promotion Model of Pender explained that ‘Individual characteristics and experiences’ affect ‘Behavior specific cognitions and affect’ and that these bring about ‘Behavioral outcome’, that is, health promoting behavior. This model is suitable for explaining nurses' PSMA. This is because it is individuals who cause patient safety accidents, and personal factors and job factors affect nurses' perception and environment like culture, which in turn affects nurses' PSMA. In this study age and work experience were applied as the personal factors affecting nurses' PSMA. ‘Behavioral specific cognition and affect’ can be gauged on perceived benefits, perceived barriers, perceived self-efficacy, activity-related affect, and interpersonal influences, thus in this study safety-related recognition and patient safety culture were applied as patient safety related recognition and affect.
The SEIPS model suggests that most of the inefficiencies and mistakes in patient nursing are caused not only by individual factors but also by inconsistent interactions and incomplete systems. The SEIPS model explains that work system affects the patient nursing process and has an effect on patient results such as patient safety or recovery level. For this study the SEIPS model's work system factors as exogenous factors affecting nurses' PSMA was applied and included job factor and organizational support as work system. Figure 1 shows the conceptual framework.
A cross-sectional design and used structured equation modeling was employed in this study. A hypothesized model for explaining nurses' PSMA was developed by conceptualizing a theoretical framework and tested by analyzing collected survey data.
The participants in this study were nurses with more than 3 months of work experience in six general hospitals in Seoul and Daejeon. Based on the view that the number of participants required for a structural equation model should be over 200 people to use maximum likelihood estimation [12], 500 copies of the questionnaire were distributed and 495 copies were collected (collection rate: 99.0%) and 486 copies were used for data analysis, excepting nine copies in which the responses were unreliable.
Job factors affecting PSMA of nurses were measured through job demand and job autonomy.
Job demand means burden level of job and includes time pressure, workload increase, suspension during the work, responsibility, and excessive job burden [13]. In this study, job demand was measured using a subscale of the Korean Occupational Stress Scale-Short Form (KOSS-SF) [13]. KOSS-SF has 8 subscales: physical environment, job demand, insufficient job control, interpersonal conflict, job insecurity, organizational system, lack of reward, occupational climate. Job demand comprised 4 items and 4 items were measured, but 2 items with low reliability were deleted and 2 items (A1, A2) were used in the study. In the 4-point scale (from 1 point [very so] to 4 points [not very so]), job demand becomes relatively lower as the score becomes higher. Scale reliability (Cronbach's α) was .68 in this study. The permission to use of the Korean Occupational Stress Scale-Short Form (KOSS-SF) was obtained by email from Chang et al. [13].
Job autonomy describes a work performing method, work plan establishment, and work criteria, and it refers to the discretionary power level [13]. In this study, job autonomy was measured using a subscale of the KOSS-SF. Four questions in total were measured, but, after the two questions with low confidence were excluded, only two questions (A7 and A8) were used for the study result. In the 4-point scale from 1 point (not very so) to 4 points (very so), job autonomy becomes relatively higher as the score becomes higher. In this study, Cronbach's α was .53.
Organizational support refers to corporate management affecting the work performing process and design and organizational practical work including human resource policy. For this study, classified organizational support into the attitude of management and staffing was analyzed.
The attitude of management refers to the awareness of management and various supporting factors [14]. For this study the attitude of management was measured using the hospital survey of patient safety culture developed by Agency for Healthcare Research and Quality (AHRQ) [1] translated and used by Kim et al.[15]. Three questions were measured in total, but just two questions (B1 and B2) were used for the study results. One question was excluded due to low confidence. Each question was scored with a 5-point scale from 1 point (not very so) to 5 points (very so) and as the score was higher, active awareness and support of management were indicated. Cronbach's α was .75 in the previous study [14], and .81 for the present study. This questionnaire for the Hospital Survey of Patient Safety Culture is open to be used without gaining special permission, and thus permission to use the tool from was acquired only from Kim [15], who translated it into Korean.
Staffing means the proper number of staff to promote the safety of patients and nurses in each department. Staffing was measured using the questionnaire developed by AHRQ [1] and translated and used by Kim et al. [15]. Four questions in total were measured, but only three questions (B4, B5, and B7) were used for the study result after one question with low confidence was excluded. Each question was scored with a 5-point scale from 1 point (not very so) to 5 points (very so) and a higher score indicated proper staffing. Cronbach's α was .55 in this study.
Safety-related recognition means that study participants are aware of, judge, remember, and control patient safety. Safety-related recognition was measured by self-efficacy, safety control, and safety knowledge.
Self-efficacy means judgment on one's own capacity to organize and conduct necessary behaviors to achieve specific work with a conviction that one can achieve required behaviors successfully in order to generate a certain result [16]. For this study self-efficacy was measured with a general self-efficacy tool developed by Sherer and Adams [17] and revised and used in a study by Kim [18]. The questions were five in total, and each question used a 5-point scale from 1 point (not very so) to 5 points (very so), while a negative question was calculated reversely. Cronbach's α was .87 in the study by Kim [18], while it was .81 in this study.
Safety control means personal cognitive ability [19] affecting work in relation to drawing safe results in performing work. In this study, safety control was measured with a safety control tool developed by Anderson et al.[19] and translated and used in the study by Chung [9]. Questions were seven in total, and measured on a 5-point scale from 1 point (not very so) to 5 points (very so). As the score was higher, self-control awareness for nurses' patient safety became higher. Cronbach's α was .84 in the study by Chung [9], while it was .85 in this study.
Safety knowledge means an adequate knowledge level on safety in treating or nursing a patient [9]. Safety knowledge was measured in this study using two scales developed by Probst and Brubaker [20] and Chung [9]. Chung [9] revised the safety knowledge tool of Neal, Griffin, and Hart [21]. The questions were five in total, and each question was measured with a 5-point scale from 1 point (not very so) to 5 points (very so). Higher scores indicated organizational member's knowledge level on safety was higher. Cronbach's α was .86 in the study by Chung [9], while it was .81 in this study.
Patient safety culture refers to personal and group values, attitude, awareness, capacity, and behavioral pattern deciding organizational health and safety management [22]. Patient safety culture was measured using the questionnaire developed by AHRQ [1] and translated by Kim et al.[15]. The questions consisted of four sub-areas: 14 questions on safety culture within a department, 4 questions on the immediate senior's/manager's attitude, 6 questions on communication and procedures, and 8 questions on safety culture between departments. There were 32 questions in total. Each question was scored with a 5-point scale from 1 point (not very so) to 5 points (very so). Higher scores indicate higher safety culture awareness. Cronbach's α was .78 in the study by Kim [15] and it was .93. in this study.
Patient safety management activities (PSMA) refer to activities that prevent all types of errors, mistakes, and accidents that may occur in the medical service delivering process, regardless of actual damages to the patient [1]. Patient safety management activities were measured using a 24 item questionnaire, modified from the accreditation of the healthcare organization developed by the Korea Health Industry Development Institute [23] to the questionnaire form used by this researcher. The items consisted of four questions on precise patient check, five on communication between medical personnel, two on high-risk drug management, three on precise operation/surgery check, seven on infection preventive activity, and three on fall preventive activity regarding PSMA. Each question was measured with a 5-point scale from 1 point (not so all the time) to 5 points (always so). As the score became higher, PSMA was higher as well. Cronbach's was .89 in this study, and Cronbach's α was .81~.93 for sub-area.
Data were collected using structured self-report questionnaires between June 25 to July 25, 2012. The researcher contacted nursing departments in six general hospitals in the Seoul and Daejeon areas. The researcher explained the purpose of the current study and its data collection methods to nurse managers and requested their participation in the study. Eligible participants were recruited per the inclusion criteria. The participants were asked to complete the informed consent form and fill out the survey. Signed consent forms and completed surveys were collected by the researcher after 2 weeks. Ethical approval was provided by the institutional review board (EU 12-24). All participants provided written informed consent before completing the questionnaires.
The collected data were analyzed using PASW Statistics 18.0 and Amos 20.0. Descriptive statistics were used for the participants' general characteristics and measured variables. The confidence of the tool was calculated with Cronbach's α whereas correlations between variables were calculated with Pearson correlation coefficient. Concerning the validation of the goodness of fit to evaluate whether the hypothetical model fit the data, the following were used: χ2 (CMIN), goodness of fit index (GFI), adjusted goodness of fit index (AGFI), root mean square error of approximation (RMSEA), comparative fit index (CFI), normed fit index (NFI), and standardized root mean square residual (SRMR).
Women made up 99.0% of the participants, those younger than 30 accounted for 63.1%, and the mean age was 30.26±6.67. Single participants accounted for 67.1%. Regarding education level, 42.0% were junior college graduates, 46.5% were university graduates, and 11.5% finished graduate school. As for work experience, the participants with more than 10 years of work experience had the highest percentage at 29.8%, followed by 5 years to less than 10 years at 28.3%, and 1 year to less than 3 years at 21.6%. Concerning work experience at the current department, the participants with 1 year to less than 3 years had the highest percentage at 31.1%, followed by 5 years to less than 10 years at 27.0%, and 3 years to less than 5 years at 20.2%. The mean work experience in the current department was 4.51±3.75 years. Regarding department, internal and surgical wards accounted for 58.4% while intensive care units accounted for 17.6%. As for participants' position, 82.3% were general nurses and 99.2% were nurses who had nurses' safety education experience.
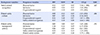
The descriptive statistics of the study variables used in the hypothetical model are as follows (Table 1): For job factors, the nurses' job demand was 2.06, and job autonomy, 2.44 out of 4 points. For organizational support, attitude of management scored 3.31, and staffing 2.46 out of 5 points. Regarding safety-related recognition, self-efficacy scored 3.73, safety control 3.52, and safety knowledge 3.53 out of 5 points. As for patient safety culture, safety culture within department scored 3.48 points, communication and procedures 2.83 points, attitude of immediate superior/manager 3.67 points, and safety culture between departments 3.33 points out of 5 points. PSMA scored 4.38±0.47 out of 5 points. For the sub-areas, high-risk drug management scored the highest with 4.58±0.57. Fall preventive activity showed 4.46±0.61 points, precise patient check, 4.45±0.57 points, precise operation/surgery check, 4.45±0.57 points, and infection preventive activity, 4.34±0.55 all high scores with more than 4 points. Communication between medical personnel was 3.96±0.71 points, the lowest among the six sub-areas.
The normality of the data was tested using the skewness and kurtosis. The absolute values were all less than 2, which met the assumption of normal distribution. If absolute correlation value (r) between measuring variables was more than .90, the problem of multicollinearity must be considered. However, the absolute correlation values between independent variables were all less than .80 in this study; therefore, no multicollinearity existed.
To enhance goodness of fit of the hypothetical model, the model was modified by allowing covariance, adding three path between the errors of y9 and y10, y10 and y12, y12 and y13 in consideration of theoretical background among the paths with more than ten modification indices. The goodness of fit of the hypothetical model was as follows: χ2=375.35, χ2 (CMIN/df)=134, GFI=.92, AGFI=.89, RMSEA=.06, NFI=.92, and CFI=.94. Therefore the criteria of the goodness of fit met the recommended levels.
The hypothetical model analysis results are shown in Table 2. In the hypothetical model, PSMA was significantly affected by job factors (γ=−.26, p=.074), safety-related recognition (β=.23, p=.025), and patient safety culture (β=.45, p<.001). The explanation power of PSMA by these variables was 29.1%. Patient safety culture was significantly affected by personal factors (γ=−.12, p=.032), organizational support (γ=.48, p<.001), and safety-related recognition (β=.38, p<.001). The explanation power of patient safety culture was 48.6%. Safety-related recognition was significantly affected by personal factors (γ=.37, p<.001), job factors (γ=.31, p=.036), and organizational support (γ=.28, p=.003). The explanation power of safety-related recognition was 44.7%(Figure 2).
Table 3 shows the standardization effect of the hypothetical model. PSMA was significantly and directly affected by job factors, safety-related recognition, and patient safety culture, and was significantly and indirectly affected by personal factors, job factors, organizational support, and safety-related recognition. PSMA showed significant and positive total effects from personal factors, organizational support, safety-related recognition, and patient safety culture. Patient safety culture received significant and direct effects from personal factors, organizational support, and safety-related recognition, and received significant and indirect effects from personal factors, job factors, and organizational support. Patient safety culture showed significant and positive total effects from organizational support and safety-related recognition. Safety-related recognition showed direct effects and total effects from personal factors, job demand, and organizational support.
The purpose of this study was to use structural equation modeling to build and test a model outlining factors influencing PSMA among nurses. These results of this study were validated by setting up 12 paths from exogenous variables to PSMA, which was the final dependent variable, through endogenous variables. As a result of validating the confirmed model, 9 hypotheses among 12 hypotheses were supported, and the other 3 were rejected.
The variable that most significantly affected nurses' PSMA was patient safety culture. Patient safety culture showed direct effects on nurses' PSMA, and therefore as the score of patient safety culture was higher, PSMA became better. Nurses who reported high score for patient safety culture were more active in patient safety management activities and reported fewer safety accidents [4142425]. The reason seemed to be that in a positive patient safety culture where mutual encouragement and cooperation were practiced, errors were systematically reported without concealment, and improvement was made from error experience which had an important effect on PSMA. Therefore, to prevent patient safety accidents, it is necessary to improve the patient safety culture in the hospital.
Patient safety culture was significantly influenced by organizational factors and nurses' safety-related recognition. As safety-related recognition such as self-efficacy, safety control, and safety knowledge was higher, and as organizational support including the support of management and staffing was adequate, the patient safety culture score was also higher. Nurses with higher safety knowledge, safety control, and self efficacy have higher patient safety culture scores [926]. Nurses' patient safety culture score increased as the attitude of management was more positive. However, insufficient staffing was an obstacle to patient safety [214].
The variables significantly affecting safety-related recognition were personal factors, job factors, and organizational support, which meant that safety-related recognition was higher as the job demand was lower, and with longer career and age and job autonomy, and a more appropriate attitude for management and staffing. As nurses become more experienced, they experience diverse accidents in the hospital environment directly and indirectly, and there are more opportunities for education and training related to patient safety which can increase their knowledge and control of safety and increase their self-efficacy. The safety-related recognition of younger nurses with less work experience was lower than that of the nurses with more work experience, and thus safety-related recognition should be enhanced through continuous and repetitive safety education and training. A nurse needs more responsibility and independence than any other professionals. If a nurse suffers from excessive workload, it becomes difficult to pay adequate attention to PSMA, and he/she could not receive adequate education/training on safety. As a result, safety knowledge and safety control of nurses are lowered, making it difficult to provide safe nursing care. In this regard, efforts to reduce job demand and improve job autonomy could be important tasks.
The second variable significantly affecting PSMA was safety-related recognition. Safety-related recognition directly affected PSMA and also indirectly affected PSMA through patient safety culture. Such a result was consistent with the previous studies [927] reporting that the higher the safety efficacy, safety knowledge, safety control, and self-efficacy, the lower the level of safety accidents. Therefore, systematic and continuous safety education and training on various hazards and risk factors should be carried out in order to raise safety awareness. Thus, nurses' safety knowledge and safety control could be improved.
The third variable significantly affecting PSMA was organizational support. Organizational support showed a significant indirect effect on nurses' PSMA: As the support of management and staffing proved sufficient, safety-related recognition and patient safety culture awareness became higher, positively affecting nurses' PSMA. Therefore, management support should be provided for patient safety policies and safety standards, safety education, safety-related resources, and adequate staffing.
The fourth variable affecting PSMA was personal factors. Although personal factors did not show direct effects to PSMA, the personal factors showed significant indirect effects and total effects. Age and work experience did not affect PSMA directly, but they affected safety-related recognition and patient safety culture, which were mediating factors significantly affecting PSMA. Such a result was partially consistent with the previous studies [814] asserting that age and work experience at hospitals affected PSMA. The previous studies did not look into direct and indirect effects by building models, but they just looked at relations between the relevant variables, and therefore age and work experience appeared to directly affect PSMA. As a result of looking at the direct and indirect effects in this study that built the model, personal factors indirectly and positively affected PSMA. Consequently, education, training, and support suitable for age and work experience should be carried out to improve such parameters.
Job factors did not show significant total effects on PSMA (such as precise patient check, communication between medical personnel, high risk drug management, precise operation/surgery check, infection preventive activity, and fall preventive activity), which means that job demand and job autonomy do not significantly affect PSMA. However, upon directly and indirectly examination of paths, job factors showed direct negative effects on PSMA, which means that nurses with high job demands and low job autonomy perform a lot of PSMA. Such a result showed differences from previous studies [728] insisting that excessive job demand has a negative correlation with the prevention of safety accidents, and longer the working hours result in a greater incidence of accidents. What this study showed was that there were more new nurses with low job autonomy and high job demand than experienced nurses, and most new nurses were engaged in direct nursing activities compared to the experienced nurses; therefore, their PSMA was high. Therefore, future research will need to be done to analyze the impact of job factors within the same career by dividing groups according to the careers of the nurses. Job factors showed significant and positive effects indirectly on safety-related recognition and patient safety culture, which were mediating factors. This means that the lower the job demand and the higher the job autonomy, the higher the safety-related recognition and patient safety culture become. However, job factors did not show statistically significant total effects to nurses' PSMA due to the offset of direct and indirect effects. Although the researcher of this study expected that job factors would have significant and direct and indirect effects on PSMA in the early stage of the study plan, there was no total effect due to significant and negative direct effects and significant and positive indirect effects as a result. Since there were few studies on the direct and indirect effects of job factors on PSMA, studies on this relation is needed.
In this study the factors affecting nurses' PSMA were discussed concerning the direct and indirect paths that each factor affected as mentioned above. The nurses' PSMA model in this study had meaning in that it was built by encompassing personal factors, job factors, and organizational support overall. This study set up the model by comprehensively integrating the factors related with nurses' PSMA through previous studies, validating its goodness of fit. In this manner, a causal relationship and influence among various factors affecting nurses' PSMA were identified. In addition, through this study, it was confirmed that safety-related recognition and patient safety culture play a mediating role in nurses' PSMA.
The aim of this study was to identify factors affecting nurses' PSMA, develop a model, test the fit between model and actual data, and present a model to account for PSMA. The model validated in this study was suitable for explaining the factors affecting nurses' PSMA. Furthermore, 9 of 12 hypothesized paths were significant. Factors that have a direct and indirect impact on nurses' PSMA are personal factors, organizational support, safety-related recognition, and patient safety culture. The explanation power of the variables included in the model on nurses' PSMA was 29.1%.
Based on all these results, it can be confirmed that personal factors, job factors, organizational support, safety-related recognition, and patient safety culture are important factors affecting nurses' PSMA. Also, results from this study show that safety-related recognition and patient safety culture played a mediating role in relation with many other factors that already existed in nurses' PSMA.
The following measures should be taken to enhance nurses' PSMA. First, personal factors such as age and work experience were found to be significant variables affecting PSMA. Therefore, a plan should be established to reduce the turnover rate of career nurses. Second, since organizational support has been found to be a significant variable influencing the PSMA, sufficient manpower allocation, education, and policy should be provided for each institution. In this study, job factors were not significant variables for PSMA, so it is necessary to study this relationship in the future.
References
1. Agency for Healthcare Research and Quality (US). Hospital survey on patient safety culture. AHRQ publication, vol 04-0041. Rockville, MD: U.S Department of Health and Human Services;Public Health Service, Agency for Healthcare Research and Quality;2004.
2. Kim EK, Kang MA, Kim HJ. Experience and perception on patient safety culture of employees in hospitals. Journal of Korean Academy of Nursing Administration. 2007; 13(3):321–334.
3. Korea Consumer Agency. A survey on the medical dispute related to safety management of hospital. Research Report. Seoul: Korea Consumer Agency;2006. 11. Report No.: 06-06.
4. Nam MH, Choi SH. The cognition level on patient safety and safe nursing activities according to nurse-patient ratios. Journal of Korean Clinical Nursing Research. 2011; 17(2):138–149.
5. Choi JH, Lee KM, Lee MA. Relationship between hospital nurses' perceived patient safety culture and their safety care activities. Journal of Korean Academy of Fundamentals of Nursing. 2010; 17(1):64–72.
6. Lee YJ. Patient safety culture and management activities perceived by hospital nurses [master's thesis]. Daejeon: Eulji University;2011. 62.
7. Kim YH, Kim SH, Kim NJ, Jung MH. Level of safety and health activities among hospital nurses. Journal of the Korean Society of Living Environmental System. 2011; 18(4):401–410.
8. Park SJ, Choi E, Lee K, Chung K. A study on perception and nursing activity for patient safety of operating room nurses. Journal of the Korea Academia-Industrial Cooperation Society. 2016; 17(11):332–339. DOI: 10.5762/KAIS.2016.17.11.332.

9. Chung SK. A structural model of safety climate and safety compliance of hospital organization employees. Asia-Pacific Journal of Multimedia Services Convergent with Art, Humanities, and Sociology. 2017; 7(8):947–961. DOI: 10.14257/ajmahs.2017.08.84.

10. Pender NJ. Health promotion in nursing practice. 3rd ed. Norwalk: Appleton & Lange;1996.
11. Carayon P, Hundt AS, Karsh B, Gurses AP, Alvarado CJ, Smith M, et al. Work system design for patient safety: the SEIPS model. Quality & Safety in Health Care. 2006; 15(1):i50–i58. DOI: 10.1136/qshc.2005.015842.

12. Kline RB. Principles and practice of structural equation modeling. 4th ed. New York: The Guilford Press;2015. p. 534.
13. Chang SJ, Koh SB, Kang D, Kim SA, Kang MG, Lee CG, et al. Developing an occupational stress scale for Korean employees. Korean Journal of Occupational and Environmental Medicine. 2005; 17(4):297–317.

14. Jeong J, Seo YJ, Nam EW. Factors affecting patient safety management activities at nursing divisions of two university hospitals. Korean Journal of Hospital Management. 2006; 11(1):91–109.
15. Kim JE, Kang MA, An KE, Sung YH. A survey of nurses' perception of patient safety related to hospital culture and reports of medical errors. Journal of Korean Clinical Nursing Research. 2007; 13(3):169–179.
16. Bandura A. A Self-efficacy: The Exercise of control. New York: WH. Freeman and Company;1997. p. 604.
17. Sherer M, Adams CH. Construct validation of the self-efficacy scale. Psychological Reports. 1983; 53(3):899–902. DOI: 10.2466/pr0.1983.53.3.899.

18. Kim SJ. Moderating effect of emotional intelligence and self-efficacy on the relationship between career commitment and career performance [master's thesis]. Gyeongsan: Yeungnam University;2007. 109.
19. Anderson L. Roles of safety control and supervisory support in work safety. Paper presented at: The 19th Annual Conference of Society of Industrial/Organizational Psychology. 2004 April 1-4; Chicago.
20. Probst TM, Brubaker TL. The effects of job insecurity on employee safety outcomes: cross-sectional and longitudinal explorations. Journal of Occupational Health Psychology. 2001; 6(2):139–159. DOI: 10.1037/1076-8998.6.2.139.


21. Neal A, Griffin MA, Hart PM. The impact of organizational climate on safety climate and individual behavior. Safety of Science. 2000; 34:99–109. DOI: 10.1016/s0925-7535(00)00008-4.

22. Sorra J, Nieva V, Fastman BR, Kaplan H, Schreiber G, King M. Staff attitudes about event reporting and patient safety culture in hospital transfusion services. Transfusion. 2008; 48:1934–1942. DOI: 10.1111/j.1537-2995.2008.01761.x.


23. Ministry of Health and Welfare (KR). Korea Health Industry Development Institute. Guidelines for hospital evaluation programme. Policy-Healthcare, vol 2006-17. Seoul: Korea Health Industry Development Institute;2006.
24. Lee YM. Safety accident occurrence to perceptions of patient safety culture of hospital nurses. Journal of the Korea Academia-Industrial Cooperation Society. 2012; 13(1):117–124. DOI: 10.5762/kais.2012.13.1.117.

25. Lee WY. Influence of job insecurity, organizational commitment, and safety climate on safety behavior and accidents. In : Proceedings of 2005 Spring Conference of the Korean Society for Railway; 2005 May; Seoul. Korean Society for Railway;p. 32–37.
26. Park YS, Lee KM. The effects of the individual and job characteristics on career commitment. Korean Journal of Local Government Studies. 2011; 15(2):35–50.
27. An GY, Park NG. Empirical study based on the Neal, Griffin, and Hart's safety climate model. Journal of the Korea Safety Management & Science. 2005; 7(5):107–117.
28. An GY. The relationship among safety motivation, antecedents and employee safety participation in SME. Korean Small Business Review. 2003; 25(4):155–179.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download