RESULTS
Patient characteristics
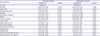
Among 13,516 patients registered in the KAMIR-NIH database, data of 10,455 patients with AMI were included in our analysis (non-DM, 6,236 patients; new-DM, 659 patients; known-DM, 3,560 patients). The proportion of patients with new-DM was 6.3%. The mean follow-up duration was 523 days. Among patients with known-DM, the mean duration of DM was 11.2 years.
Patients with known-DM were older, more likely to be female, and less likely to be a smoker at the time of admission for AMI. Patients in the known-DM group also had higher incidence of hypertension, dyslipidemia, prior ischemic heart disease (angina, myocardial infarction), renal dysfunction, and LV dysfunction. Furthermore, compared to the new-DM and non-DM groups, the known-DM group had higher incidence of left main coronary artery disease and multivessel disease. The LVEF and Killip class were poorer in patients with known-DM. PCI was performed for 90.6%, 90.0%, and 87.4% of patients in the non-DM, new-DM, and known-DM groups, respectively. Glycoprotein IIb/IIIa inhibitors were more frequently used in non-DM patients.
Compared to patients with non-DM or known-DM, those with new-DM were younger, more likely to be male and to smoke, and had higher levels of low-density lipoprotein (LDL)-cholesterol. Additionally, compared to the non-DM group, the new-DM group had a higher incidence of previous stroke, prior angina, depressed LV systolic function (ejection fraction <50%), type B2/C lesion, and use of beta-blockers. Patient characteristics were described at
Table 1.
Table 1
Baseline characteristics, clinical performance, and angiographic findings

|
Characteristics |
Non-DM (n=6,236) |
New-DM (n=659) |
Known-DM (n=3,560) |
|
Age (years) |
64.2±13.5 |
60.4±12.9*
|
66.3±11.1*,†
|
|
Men |
74.4 |
78.1*
|
68.3*,†
|
|
STEMI |
50.6 |
52.8 |
42.0*,†
|
|
Non-STEMI |
49.4 |
47.2 |
58.0*,†
|
|
Mean diabetes duration (years) |
|
|
11.2 |
|
Medical history |
|
|
|
|
Hypertension |
58.9 |
42.9 |
67.8*,†
|
|
Dyslipidemia |
10.6 |
9.6 |
14.9*,†
|
|
Current smoking |
40.6 |
53.4*
|
31.4*,†
|
|
Prior stroke |
6.0 |
5.5*
|
10.1*,†
|
|
Prior angina |
8.7 |
6.1*
|
13.7*,†
|
|
Prior myocardial infarction |
6.1 |
6.8 |
11.5*,†
|
|
Renal dysfunction (Cr >2.0 mg/dL) |
2.9 |
1.4 |
12.0*,†
|
|
Depressed LV systolic function (<50%) |
35.2 |
39.1*
|
44.2*,†
|
|
Laboratory finding |
|
|
|
|
HbA1c |
5.64±0.38 |
7.68±1.48*
|
7.61±1.66*
|
|
Glucose |
142.1±49.3 |
216.4±90.4 |
227.2±105.4*,†
|
|
|
Cr (mg/dL) |
1.07±2.73 |
0.97±0.57*
|
1.46±1.64*,†
|
|
|
LDL-cholesterol (mg/dL) |
113.9±38.1 |
122.9±41.5*
|
100.3±40.1*,†
|
|
|
Peak CK-MB (ng/mL) |
119.6±179.2 |
111.6±137.7 |
83.4±125.2*,†
|
|
|
Peak troponin I (ng/mL) |
48.4±111.8 |
53.2±102.7 |
43.9±89.4 |
|
|
Peak troponin T (ng/mL) |
5.7±18.3 |
7.4±23.5 |
4.7±6.3*,†
|
|
|
NT-proBNP |
1,989.1±5,625.9 |
2,301.1±9,500.0 |
4,732.8±13,992.4*,†
|
|
|
BNP |
254.6±606.5 |
258.3±554.2 |
557.2±1,086.2*,†
|
|
|
hs-CRP |
1.65±13.7 |
1.61±3.93 |
2.34±10.81*
|
|
BMI (kg/m2) |
24.8±49.8 |
24.9±3.7 |
24.5±15.9 |
|
Ejection fraction (%) |
52.7±10.8 |
51.2±11.1*
|
50.1±12.1*,†
|
|
Killip class (III, IV) |
10.9 |
12.6 |
17.8*,†
|
|
Angiographic finding |
|
|
|
|
1 vessel disease |
53.8 |
50.7 |
41.2*,†
|
|
Left main related |
3.7 |
2.6 |
5.4*,†
|
|
Multivessel disease |
46.2 |
49.3 |
58.8*,†
|
|
Lesion type (type B2/C) |
86.6 |
90.2*
|
86.6†
|
|
Culprit vessel |
|
|
|
|
Left main |
1.9 |
2.3 |
3.2*
|
|
Left anterior descending artery |
46.6 |
44.7 |
45.5*
|
|
Left circumflex artery |
17.6 |
17.2 |
16.7*
|
|
Right coronary artery |
33.9 |
35.8 |
34.6*
|
|
Initial-TIMI flow (0 or 1) |
59.8 |
60.0 |
52.4*,†
|
|
Post-TIMI flow (<3) |
3.5 |
3.1 |
3.6 |
|
PCI |
90.6 |
92.0 |
87.4*,†
|
|
Medication during admission |
|
|
|
|
Aspirin |
99.6 |
100.0 |
99.1*,†
|
|
Clopidogrel |
78.5 |
78.1 |
81.7*,†
|
|
Ticagrelor |
22.5 |
20.3 |
18.7*
|
|
Prasugrel |
11.7 |
15.2*
|
10.1*,†
|
|
Cilostazol |
9.7 |
12.0 |
12.8 |
|
Beta-blocker |
81.3 |
85.4*
|
80.5†
|
|
ACE inhibitor |
49.2 |
54.0*
|
39.8*,†
|
|
ARB |
29.9 |
29.0 |
36.2*,†
|
|
Statin |
91.6 |
92.7 |
85.8*,†
|

Clinical outcomes
The incidence of all-cause death, cardiac death, re-AMI, re-PCI, CHF, and MACE were significantly higher in the known-DM group than in the non-DM and new-DM groups. However, the groups did not differ in terms of stent thrombosis or cerebral infarction rate (
Figure 2). The cumulative incidence of MACEs (i.e., cardiac death, re-AMI, re-PCI, or hospitalization related to CHF) was greater in the known-DM group and similar between the new-DM and non-DM groups (
Figure 3).
 | Figure 2
Long-term clinical outcomes after AMI. Patients were stratified according to DM status at admission for AMI: non-DM, DM not diagnosed at the time of admission for AMI; known-DM, DM diagnosed prior to admission for AMI; new-DM, DM diagnosed at admission for AMI.
AMI = acute myocardial infarction; CHF = congestive heart failure; DM = diabetes mellitus; known-DM = previously diagnosed diabetes mellitus; MACE = major adverse cardiac event; new-DM = newly diagnosed diabetes mellitus; re-AMI = recurrent acute myocardial infarction; re-PCI = revascularization via repeat percutaneous coronary intervention.
*p<0.05 vs. non-DM, †p<0.05 for known-DM vs. new-DM.

|
 | Figure 3
Kaplan-Meier curves for survival free of adverse events and reintervention after AMI. (A) Cumulative incidence of MACEs, (B) cardiac mortality, (C) re-AMI, (D) re-PCI, and (E) hospitalization related to CHF.
AMI = acute myocardial infarction; CHF = congestive heart failure; DM = diabetes mellitus; known-DM = previously diagnosed diabetes mellitus; MACE = major adverse cardiovascular event; new-DM = newly diagnosed diabetes mellitus; re-AMI = recurrent acute myocardial infarction; re-PCI = revascularization via repeat percutaneous coronary intervention.

|
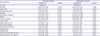
Effect of DM status on clinical outcomes
Next, we examined whether DM status was an independent predictor of clinical outcomes after AMI. In univariate analysis, known-DM was associated with increased incidence of MACEs (HR, 1.60; 95% CI, 1.45–1.76), cardiac death (HR, 1.91; 95% CI, 1.65–2.21), and re-AMI (HR, 1.91; 95% CI, 1.65–2.21). In multivariate analysis, known-DM remained an independent predictor for MACEs (HR, 1.20; 95% CI, 1.06–1.35), cardiac death (HR, 1.26; 95% CI, 1.01–1.57), re-AMI (HR, 1.26; 95% CI, 1.01–1.57), and hospitalization for CHF (HR, 1.58; 95% CI, 1.20–2.08). However, there was no significant association between DM status and the incidence of stent thrombosis, cerebral infarction, or re-PCI (
Table 2).
Table 2
Multivariate analysis for clinical outcomes

|
Clinical outcomes |
Non-DM |
New-DM |
Known-DM |
|
HR (95% CI) |
HR (95% CI) |
p value |
HR (95% CI) |
p value |
|
MACE |
870 (14.2) |
83 (12.9) |
|
767 (22.3)*,†
|
|
|
Unadjusted |
Reference |
0.87 (0.70–1.09) |
0.235 |
1.60 (1.45–1.76) |
<0.001 |
|
Adjusted |
Reference |
0.94 (0.72–1.23) |
0.648 |
1.20 (1.06–1.35) |
0.004 |
|
Cardiac death |
350 (5.6) |
29 (4.4) |
|
375 (10.5)*,†
|
|
|
Unadjusted |
Reference |
0.77 (0.53–1.12) |
0.171 |
1.91 (1.65–2.21) |
<0.001 |
|
Adjusted |
Reference |
0.92 (0.55–1.54) |
0.761 |
1.26 (1.01–1.57) |
0.042 |
|
Re-AMI |
137 (2.2) |
16 (2.4) |
|
135 (3.8)*
|
|
|
Unadjusted |
Reference |
0.77 (0.53–1.12) |
0.171 |
1.91 (1.65–2.21) |
<0.001 |
|
Adjusted |
Reference |
0.92 (0.55–1.55) |
0.761 |
1.26 (1.01–1.57) |
0.042 |
|
Stent thrombosis |
34 (0.5) |
4 (0.6) |
|
30 (0.8) |
|
|
Unadjusted |
Reference |
1.05 (0.37–2.96) |
0.924 |
1.54 (0.94–2.51) |
0.087 |
|
Adjusted |
Reference |
0.83 (0.25–2.74) |
0.762 |
1.47 (0.86–2.50) |
0.158 |
|
Cerebral infarction |
111 (1.8) |
10 (1.5) |
|
87 (2.4)*
|
|
|
Unadjusted |
Reference |
0.82 (0.43–1.57) |
0.558 |
1.40 (1.06–1.85) |
0.019 |
|
Adjusted |
Reference |
1.00 (0.48–2.01) |
0.996 |
1.17 (0.84–1.63) |
0.367 |
|
Re-PCI |
292 (4.7) |
26 (3.9) |
|
213 (6.0)*,†
|
|
|
Unadjusted |
Reference |
0.81 (0.54–1.21) |
0.308 |
1.31 (1.10–1.57) |
0.003 |
|
Adjusted |
Reference |
0.78 (0.52–1.22) |
0.286 |
1.09 (0.90–1.33) |
0.362 |
|
CHF |
133 (2.1) |
18 (2.7) |
|
137 (3.8)*
|
|
|
Unadjusted |
Reference |
1.22 (0.75–2.00) |
0.427 |
1.86 (1.46–2.36) |
<0.001 |
|
Adjusted |
Reference |
1.21 (0.68–2.16) |
0.522 |
1.58 (1.20–2.08) |
0.001 |

Subgroup analysis was performed according to several risk factors (
Table 3). Known-DM was an independent predictor for MACEs in patients who were female (HR, 1.32; 95% CI, 1.08–1.62), elderly (HR, 1.21; 95% CI, 1.05–1.40), had one vessel disease (HR, 1.28; 95% CI, 1.04–1.58), STEMI (HR, 1.20; 95% CI, 1.00–1.43), non-STEMI (HR, 1.19; 95% CI, 1.00–1.41), or a high BMI (HR, 1.27; 95% CI, 1.05–1.54). However, analysis indicated that known-DM was not an independent predictor for male patients or those with young age, multivessel disease, or low BMI.
Table 3
Subgroup analysis for MACEs

|
MACEs |
Non-DM |
New-DM |
Known-DM |
|
HR (95% CI) |
p value |
HR (95% CI) |
p value |
|
Gender |
|
|
|
|
|
|
Female |
Reference |
1.13 (0.70–1.82) |
0.613 |
1.32 (1.08–1.62) |
0.008 |
|
Male |
Reference |
0.88 (0.64–1.21) |
0.426 |
1.14 (0.97–1.33) |
0.105 |
|
Age (years) |
|
|
|
|
|
|
Young age (<60) |
Reference |
0.92 (0.60–1.42) |
0.713 |
1.14 (0.89–1.47) |
0.296 |
|
Old age (≥60) |
Reference |
0.95 (0.68–1.34) |
0.767 |
1.21 (1.05–1.40) |
0.008 |
|
Multivessel disease |
|
|
|
|
|
|
One vessel disease |
Reference |
1.13 (0.75–1.72) |
0.557 |
1.28 (1.04–1.58) |
0.022 |
|
Multivessel disease |
Reference |
0.83 (0.59–1.18) |
0.303 |
1.14 (0.98–1.33) |
0.091 |
|
Final diagnosis |
|
|
|
|
|
|
Non-STEMI |
Reference |
0.80 (0.53–1.21) |
0.296 |
1.19 (1.00–1.41) |
0.047 |
|
STEMI |
Reference |
1.08 (0.76–1.54) |
0.665 |
1.20 (1.00–1.43) |
0.046 |
|
BMI |
|
|
|
|
|
|
Low |
Reference |
0.89 (0.61–1.31) |
0.563 |
1.15 (0.98–1.35) |
0.097 |
|
High |
Reference |
1.02 (0.71–1.48) |
0.903 |
1.27 (1.05–1.54) |
0.013 |

Risk factors for MACEs
The predictors of MACEs in patients with AMI were analyzed (
Table 4). Univariate analysis indicated that the HR with 95% CI for MACEs was 0.87 (95% CI, 0.70–1.09; p=0.235) and 1.60 (95% CI, 1.45–1.76; p<0.001) in new-DM and known-DM patients, respectively, relative to that of non-DM patients. Other significant predictors for MACEs were old age (HR, 2.16; 95% CI, 1.93–2.41; p<0.001), male sex (HR, 0.67; 95% CI, 0.60–0.73; p<0.001), BMI group (>24 kg/m
2; HR, 0.71; p=0.001), current smoking (HR, 0.65; 95% CI, 0.58–0.72; p<0.001), low LVEF (HR, 1.92; 95% CI, 1.74–2.13; p<0.001), poor Killip class (HR, 3.15; 95% CI, 2.84–3.50; p<0.001), multivessel disease (HR, 1.83; 95% CI, 1.66–2.03; p<0.001), low post-TIMI (HR, 2.17; 95% CI, 1.75–2.68; p<0.001), hypertension (HR, 1.61; 95% CI, 1.45–1.79; p<0.001), dyslipidemia (HR, 0.76; 95% CI, 0.65–0.89; p=0.001), previous myocardial infarction (HR, 1.60; 95% CI, 1.38–1.86; p<0.001), and renal failure (HR, 3.39; 95% CI, 2.96–3.88; p<0.001).
Table 4
Unadjusted and adjusted risks for MACEs
|
Characteristics |
Univariate analysis |
Multivariate analysis |
|
HR (95% CI) |
p value |
HR (95% CI) |
p value |
|
Non-DM |
Reference |
|
Reference |
|
|
New-DM |
0.87 (0.70–1.09) |
0.235 |
0.94 (0.72–1.23) |
0.648 |
|
Known-DM |
1.60 (1.45–1.76) |
<0.001 |
1.20 (1.06–1.35) |
0.004 |
|
Old age (>60 years) |
2.16 (1.93–2.41) |
<0.001 |
1.38 (1.19–1.60) |
<0.001 |
|
Male sex |
0.67 (0.60–0.73) |
<0.001 |
0.80 (0.70–0.92) |
0.001 |
|
BMI group (>24 kg/m2) |
0.71 (0.65–0.79) |
<0.001 |
0.86 (0.76–0.96) |
0.010 |
|
STEMI |
0.96 (0.88–1.06) |
0.445 |
0.96 (0.86–1.09) |
0.536 |
|
Current smoking |
0.65 (0.58–0.72) |
<0.001 |
0.97 (0.85–1.12) |
0.715 |
|
LVEF (<50%) |
1.92 (1.74–2.13) |
<0.001 |
1.48 (1.31–1.66) |
<0.001 |
|
Killips class (III, IV) |
3.15 (2.84–3.50) |
<0.001 |
1.55 (1.34–1.80) |
<0.001 |
|
Multivessel disease |
1.83 (1.66–2.03) |
<0.001 |
1.54 (1.38–1.74) |
<0.001 |
|
Post-TIMI flow (TIMI ≤2) |
2.17 (1.75–2.68) |
<0.001 |
1.52 (1.16–1.99) |
0.003 |
|
Hypertension |
1.61 (1.45–1.79) |
<0.001 |
1.32 (1.15–1.50) |
<0.001 |
|
Dyslipidemia |
0.76 (0.65–0.89) |
0.001 |
0.85 (0.70–1.02) |
0.078 |
|
Previous myocardial infarction |
1.60 (1.38–1.86) |
<0.001 |
1.41 (1.17–1.70) |
<0.001 |
|
Renal failure (Cr >2.0 mg/dL) |
3.39 (2.96–3.88) |
<0.001 |
2.13 (1.77–2.57) |
<0.001 |

Multivariate analysis also showed that the risk for MACEs was significantly higher in known-DM (HR, 1.20; 95% CI, 1.06–1.35; p=0.004) and not known-DM (HR, 0.94; 95% CI, 0.72–1.23; p=0.648). Multivariate analysis identified further risk factors for MACEs, such as old age (HR, 1.38; 95% CI, 1.19–1.60; p<0.001), male sex (HR, 0.80; 95% CI, 0.70–0.92; p=0.001), high BMI (HR, 0.86; 95% CI, 0.76–0.96; p=0.010), low LVEF (HR, 1.48; 95% CI, 1.31–1.66; p<0.001), poor Killip class (HR, 2.16; 95% CI, 1.93–2.41; p<0.001), multivessel disease (HR, 1.54; 95% CI, 1.38–1.74; p<0.001), low post-TIMI flow (HR, 1.52; 95% CI, 1.16–1.99; p=0.003), hypertension (HR, 1.32; 95% CI, 1.15–1.50; p<0.001), previous myocardial infarction (HR, 1.41; 95% CI, 1.17–1.70; p<0.001), and renal failure (HR, 2.13; 95% CI, 1.77–2.57; p<0.001).
DISCUSSION
In this multicenter, prospective, observational study, known-DM was a significant independent predictor of cardiac mortality, MACEs, re-AMI, and hospitalization for CHF during long-term follow-up after AMI. However, new-DM was not associated with increased risk of adverse clinical outcomes compared to the risk noted in non-DM patients. These results suggest that known-DM, but not new-DM, is strongly associated with worse clinical outcomes in patients with AMI.
The Multiple Risk Factor Intervention Trial and Framingham Heart Study reported on the importance of the association between DM and coronary heart disease (CHD).
12)
The risk of infarction was reported to be greatest in patients with DM and prior myocardial infarction.
13) Several studies reported that patients with AMI and known-DM have poor outcomes compared to those of patients with other comorbidities.
14)15) Previous studies using data from Korean registries also suggested that DM has a high association with 1-year mortality, which exceeds the in-hospital mortality of patients with AMI who underwent successful PCI.
16)
Several studies suggested that patients with DM may have poorer outcomes because of the greater prevalence of multivessel disease with atherosclerotic plaque burden, a pro-thrombotic state, and more neo-intimal proliferation.
17)18) In the present study, multivessel disease and left main coronary artery disease were indeed more prevalent in the known-DM group.
Multiple mechanisms have been reported to lead to the increased incidence of MACEs in patients with DM. Specifically, a hypercoagulable state, plaque ulceration, and intracoronary thrombus were more frequently noted among DM patients,
19) as were shear-induced platelet adhesion and subendothelium aggregation.
20) Coronary tissue from patients with DM exhibits more lipid-rich atheromas, macrophage infiltration, and subsequent thrombosis.
21) DM increases the risk of heart failure independent of CHD and hypertension, and may cause cardiomyopathy. Recent research in humans and animals has provided novel insights into the underlying molecular and pathophysiological mechanisms that increase the vulnerability of patients with DM to heart to failure, including mitochondrial dysfunction, altered substrate metabolism, and activation of the renin-angiotensin system.
22)
Because the frequency of new-DM was higher in patients with AMI and since DM status at baseline affects clinical outcomes, prognosis evaluation should consider DM status.
4)5) The prevalence of new-DM was reported to be 3.8%–17.0% among patients with AMI. Data sets from the Cleveland Clinic, Valliant, HORIZONS-AMI, and Tian et al.'s studies
5) define 8.0%, 4.0%, 3.8%, and 17.0% of patients with AMI as new-DM, respectively.
4)8)23) Therefore, all patients with AMI should be screened for DM. In our study, 6.3% of patients were newly diagnosed with DM upon admission for AMI based on HbA1c >6.5%, indicating a slightly higher prevalence of new-DM compared to what is expected based on previous reports.
Diabetes can be diagnosed using HbA1c criteria or plasma glucose criteria after either fasting or at 2 hours after a 75 g oral glucose tolerance test.
24) Only HbA1c was used for diagnosis since we were restricted to tests that were included in the registry. As a result, diabetes may have been under-diagnosed. While DM is difficult to diagnose in AMI patients based solely on HbA1c because of temporarily increased glucose levels,
25) we observed an incidence of 6.3% for new-DM using a single HbA1c-based criterion.
Several studies have reported prognosis after AMI according to DM status and classified patients as new-DM, known-DM, or non-DM. In the VALIANT cohort study, subjects with AMI were divided into 3 such groups. Patients with known-DM had poorer clinical outcomes, similar to patients that exhibited new-DM for at least 1 year.
4) The HORIZONS-AMI trial database study suggested that patients with new-DM have a similarly poor prognosis after primary PCI in STEMI compared to those with known-DM for 3 years.
8) However, Tian et al.
5) reported that known-DM was an independent predictor for short-term mortality and MACEs in AMI patients, while new-DM was associated with similar outcomes as those noted for non-DM for 30 days. The observations from that study were similar to those in the present study. Meanwhile, the composite cardiovascular events were higher in the VALIANT (25% for 1 year) and HORIZON-AMI (20.9% for 3 years) studies in comparison to this study (16% for 17 months).
This study revealed that known-DM, not new-DM, resulted in increased risk of adverse outcomes in AMI, even after multivariate analysis.
In the VALIANT study, patients with cardiogenic shock or renal failure (Cr levels >2.5 mg/dL) were excluded. Moreover, the method of diagnosing new-DM was not described, and diagnosis was individually established by physician assessment. Finally, duration of DM was not indicated.
4) The HORIZONS-AMI was a sub-study of an antiplatelet study in patients with STEMI. As a result, patients with multivessel disease, bifurcation lesion, and left main disease were excluded. Moreover, they did not suggest a diagnostic method for diabetes nor did they record the duration of DM. Conversely, the study by Tian et al.
5) included all patients with AMI and used HbA1c levels to establish a cutoff in a manner similar to that performed in this study to establish DM diagnosis. Moreover, they did not exclude patients with cardiogenic shock or renal failure. We included patients with renal failure and cardiogenic shock, and these factors were entered into the multivariate analysis model.
Interestingly, the VALIANT study did not include information relating to several lab values, such as Cr and LDL-cholesterol. In the VALIANT study, Killip class was poorer in patients with new-DM and known-DM compared to non-DM patients. This is not in agreement with our findings or with those of Tian et al.,
5) that Killip class of new-DM was similar to that of non-DM, but was better that of known-DM patients. Another study reported that Killip class was a major predictor of mortality and morbidity after AMI,
26) and is likely related to the poor outcomes we found in patients with known-DM, but not in patients with new-DM or non-DM. In the HORIZON-AMI study, pre-TIMI flow and LVEF were poor in new-DM patients, while these factors were better in known-DM patients included in this study.
In new-DM patients, higher LDL-cholesterol levels have been successfully managed via guideline-based treatment, and it is likely that the younger age noted in new-DM patients partially accounts for the fact that clinical outcomes were similar to those of non-DM patients. The present study revealed that renal failure, LV dysfunction, high levels of brain natriuretic peptides, poor Killip class, low TIMI flow, multivessel disease, and left main coronary artery disease were more prevalent in patients with known-DM, but occurred at a similar incidence in new-DM and non-DM patients. Patients with known-DM had a higher incidence of comorbidities (previous hypertension, dyslipidemia, angina, myocardial infarction, stroke) and were more likely to be female, factors previously confirmed as independent predictors of cardiovascular events after AMI.
18)27) However, the new-DM and non-DM groups generally did not differ with respect to these characteristics.
Previously, Kang et al.
28) reported that smoking was associated with a 48% decrease in the risk of all-cause mortality after AMI. The rate of current smoking was higher in new-DM patients in this study, which may have influenced outcomes.
In the known-DM group, the mean duration of DM was 11.2 years. While this parameter could not be determined in patients with new-DM, DM duration was likely shorter in patients with new-DM than in those with known-DM. Previous studies in patients with AMI did not indicate DM duration. However, DM duration was independently associated with the risk of death related to CHD.
29) Prolonged DM was associated with intravascular ultrasound-defined thin-cap fibroatheroma, a plaque phenotype associated with risk of rupture and CHD.
30) Taken together, these results suggest that short-duration DM and improved baseline characteristics are the main factors responsible for better outcomes in patients with AMI and new-DM. Furthermore, we suspect that new-DM after AMI was managed via intensive medical therapy, which, combined with the relatively short-duration of DM, likely resulted in similar clinical outcomes as those noted for non-DM patients.
HbA1c level was similar between known-DM and new-DM patients. Unfortunately, there were no data regarding HbA1c level in patients with newly diagnosed diabetes who experienced an AMI. Although patients who were diagnosed with DM for the first time after AMI had relatively high HbA1c levels, this may be due to their history of AMI, advanced stage, and lack of medications.
Moreover, our subgroup analysis indicates that known-DM independently predicted MACEs in female patients or with those with old age, one vessel disease, STEMI, non-STEMI, or high BMI. Non-DM was not statically related to MACEs in all categories that were tested. The rate of PCI was higher in non-DM and new-DM patients compared to known-DM patients. Ultimately, we could not determine why patients did not undergo PCI; however, known-DM patients were associated with higher multivessel disease, older age, and unstable vital signs (poor Killip class), and these factors could contraindicate PCI.
Our study has several limitations. A major limitation is that the present study is based on registry data. Although rigorous adjustment analyses were performed, unmeasured hidden biases may remain, and a large number of patients were excluded due to lack of data regarding HbA1c level or diabetes history. The second drawback was a high rate of loss to follow-up. Since data collection was voluntary at each participating center, the follow-up data were partially incomplete. Third, glucose status and medication compliance could not be obtained from follow-up patients. The merits of this study include its large sample size, multicenter design, and prospective data collection. Furthermore, a single, unambiguous criterion was used to diagnose diabetes.
Known-DM was associated with a higher risk of long-term cardiac death, re-AMI, hospitalization related to CHF, and overall incidence of MACEs, and these trends held true even after multivariate adjustment. Our findings confirm similar previous observations; however, new-DM was not associated with increased risk of death or adverse cardiovascular events compared to the risk noted for non-DM. This observation may be related to differences in baseline characteristics and duration of DM. The outcome of patients with new-DM was similar to that of non-DM patients, which is explained by the fact that patients with new-DM likely received intensive medical therapy after AMI.










 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download