1. Sabik JF 3rd, Lytle BW, Blackstone EH, Houghtaling PL, Cosgrove DM. Comparison of saphenous vein and internal thoracic artery graft patency by coronary system. Ann Thorac Surg. 2005; 79(2):544–551.


2. Hwang HY, Kim JS, Kim KB. Angiographic equivalency of off-pump saphenous vein and arterial composite grafts at one year. Ann Thorac Surg. 2010; 90(2):516–521.


3. Lüscher TF, Diederich D, Siebenmann R, Lehmann K, Stulz P, von Segesser L, et al. Difference between endothelium-dependent relaxation in arterial and in venous coronary bypass grafts. N Engl J Med. 1988; 319(8):462–467.


4. Pearson PJ, Evora PR, Schaff HV. Bioassay of EDRF from internal mammary arteries: implications for early and late bypass graft patency. Ann Thorac Surg. 1992; 54(6):1078–1084.


5. van Son JA, Smedts F, Vincent JG, van Lier HJ, Kubat K. Comparative anatomic studies of various arterial conduits for myocardial revascularization. J Thorac Cardiovasc Surg. 1990; 99(4):703–707.


6. Kim KB, Kang CH, Chang WI, Lim C, Kim JH, Ham BM, et al. Off-pump coronary artery bypass with complete avoidance of aortic manipulation. Ann Thorac Surg. 2002; 74(4):S1377–S1382.

7. Dion R. Complete arterial revascularization with the internal thoracic arteries. Oper Tech Thorac Cardiovasc Surg. 1996; 1(2):84–107.

8. Kim KB, Hwang HY, Hahn S, Kim JS, Oh SJ. A randomized comparison of the saphenous vein versus right internal thoracic artery as a Y-composite graft (SAVE RITA) trial: one-year angiographic results and mid-term clinical outcomes. J Thorac Cardiovasc Surg. 2014; 148(3):901–907.


9. Hwang HY, Kim JS, Oh SJ, Kim KB. A randomized comparison of the saphenous vein versus right internal thoracic artery as a Y-composite graft (SAVE RITA) trial: early results. J Thorac Cardiovasc Surg. 2012; 144(5):1027–1033.


10. Tedoriya T, Kawasuji M, Sakakibara N, Ueyama K, Watanabe Y. Pressure characteristics in arterial grafts for coronary bypass surgery. Cardiovasc Surg. 1995; 3(4):381–385.

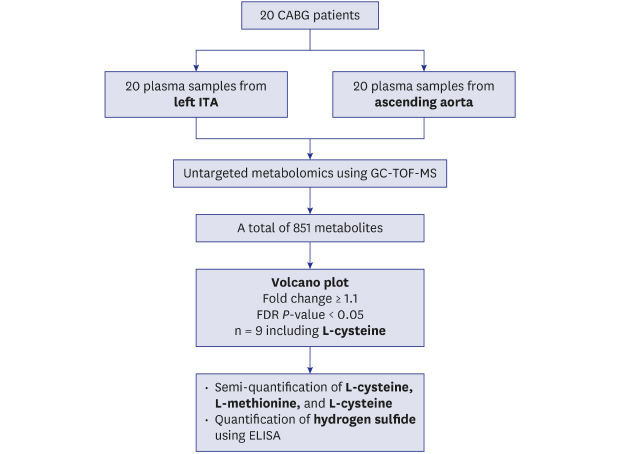
11. Fiehn O. Metabolomics by gas chromatography-mass spectrometry: combined targeted and untargeted profiling. Curr Protoc Mol Biol. 2016; 114(1):30.4.1–32.

13. Xia J, Wishart DS. Using metaboanalyst 3.0 for comprehensive metabolomics data analysis. Curr Protoc Bioinformatics. 2016; 55(1):14.10.1–91.

19. Storey JD. A direct approach to false discovery rates. J R Stat Soc Series B Stat Methodol. 2002; 64(3):479–498.

21. Chen L, Cheng CY, Choi H, Ikram MK, Sabanayagam C, Tan GS, et al. Plasma metabonomic profiling of diabetic retinopathy. Diabetes. 2016; 65(4):1099–1108.


23. Al-Ruzzeh S, Modine T, Athanasiou T, Mazrani W, Azeem F, Nakamura K, et al. Can the use of the radial artery be expanded to all patients with different surgical grafting techniques? Early clinical and angiographic results in 600 patients. J Card Surg. 2005; 20(1):1–7.


24. Jung SH, Song H, Choo SJ, Je HG, Chung CH, Kang JW, et al. Comparison of radial artery patency according to proximal anastomosis site: direct aorta to radial artery anastomosis is superior to radial artery composite grafting. J Thorac Cardiovasc Surg. 2009; 138(1):76–83.


25. Watson RA, Hamza M, Tsakok TM, Tsakok MT. Radial artery for coronary artery bypass grafting: does proximal anastomosis to the aorta or left internal mammary artery achieve better patency? Interact Cardiovasc Thorac Surg. 2013; 17(6):1020–1024.


26. Dimitrova KR, Hoffman DM, Geller CM, Dincheva G, Ko W, Tranbaugh RF. Arterial grafts protect the native coronary vessels from atherosclerotic disease progression. Ann Thorac Surg. 2012; 94(2):475–481.


27. Shen Y, Shen Z, Luo S, Guo W, Zhu YZ. The cardioprotective effects of hydrogen sulfide in heart diseases: from molecular mechanisms to therapeutic potential. Oxid Med Cell Longev. 2015; 2015:925167.

28. Stipanuk MH. Sulfur amino acid metabolism: pathways for production and removal of homocysteine and cysteine. Annu Rev Nutr. 2004; 24(1):539–577.


30. Szabó G, Veres G, Radovits T, Gero D, Módis K, Miesel-Gröschel C, et al. Cardioprotective effects of hydrogen sulfide. Nitric Oxide. 2011; 25(2):201–210.


31. Liu YH, Lu M, Hu LF, Wong PT, Webb GD, Bian JS. Hydrogen sulfide in the mammalian cardiovascular system. Antioxid Redox Signal. 2012; 17(1):141–185.


32. Wang Q, Wang XL, Liu HR, Rose P, Zhu YZ. Protective effects of cysteine analogues on acute myocardial ischemia: novel modulators of endogenous H(2)S production. Antioxid Redox Signal. 2010; 12(10):1155–1165.


33. Shackebaei D, King N, Shukla B, Suleiman MS. Mechanisms underlying the cardioprotective effect of L-cysteine. Mol Cell Biochem. 2005; 277(1-2):27–31.


34. Elsey DJ, Fowkes RC, Baxter GF. L-cysteine stimulates hydrogen sulfide synthesis in myocardium associated with attenuation of ischemia-reperfusion injury. J Cardiovasc Pharmacol Ther. 2010; 15(1):53–59.


35. Hamza RZ, El-Shenawy NS. The beneficial effects of l-cysteine on brain antioxidants of rats affected by sodium valproate. Hum Exp Toxicol. 2017; 36(11):1212–1221.












 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download