1. Mavrodi A, Paraskevas G. Evolution of the paranasal sinuses' anatomy through the ages. Anat Cell Biol. 2013; 46:235–238. PMID:
24386595.
2. Nuñez-Castruita A, López-Serna N, Guzmán-López S. Prenatal development of the maxillary sinus: a perspective for paranasal sinus surgery. Otolaryngol Head Neck Surg. 2012; 146:997–1003. PMID:
22267494.
3. Standring S. Gray's anatomy: the anatomical basis of clinical practice. 41st ed. London: Elsevier Health Sciences;2015.
4. Lang J. Clinical anatomy of the nose, nasal cavity, and paranasal sinuses. New York: Thieme Medical Publishers;1989.
5. Duncavage J. The maxillary sinus: medical and surgical management. New York: Thieme Medical Publishers;2011.
6. Chanavaz M. Maxillary sinus: anatomy, physiology, surgery, and bone grafting related to implantology: eleven years of surgical experience (1979-1990). J Oral Implantol. 1990; 16:199–209. PMID:
2098563.
7. Eberhardt JA, Torabinejad M, Christiansen EL. A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Oral Surg Oral Med Oral Pathol. 1992; 73:345–346. PMID:
1545967.
8. Kilic C, Kamburoglu K, Yuksel SP, Ozen T. An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur J Dent. 2010; 4:462–467. PMID:
20922167.
9. Roque-Torres GD, Ramirez-Sotelo LR, Vaz SL, Bóscolo SM, Bóscolo FN. Association between maxillary sinus pathologies and healthy teeth. Braz J Otorhinolaryngol. 2016; 82:33–38. PMID:
26727608.
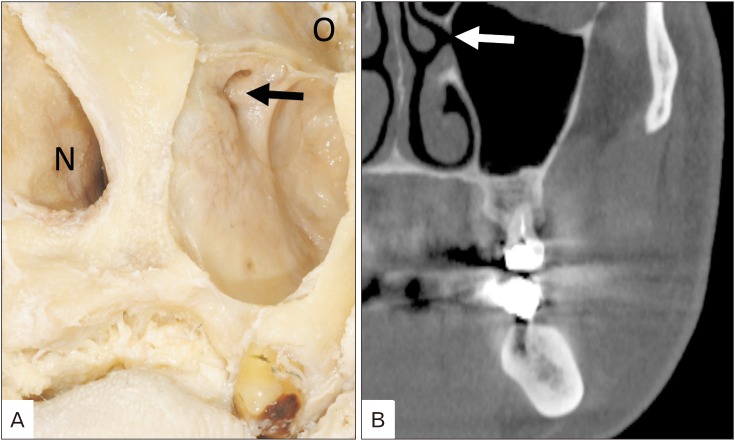
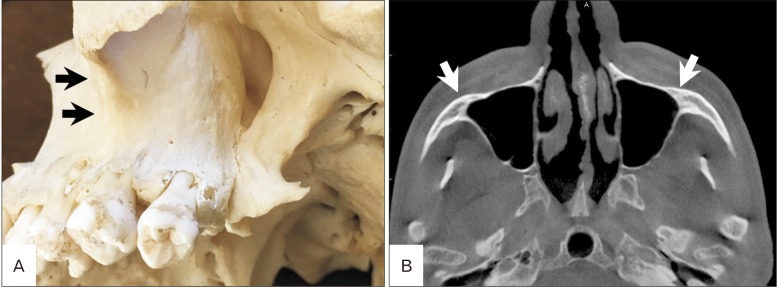
10. Kim MJ, Jung UW, Kim CS, Kim KD, Choi SH, Kim CK, Cho KS. Maxillary sinus septa: prevalence, height, location, and morphology: a reformatted computed tomography scan analysis. J Periodontol. 2006; 77:903–908. PMID:
16671885.
11. Krennmair G, Ulm CW, Lugmayr H, Solar P. The incidence, location, and height of maxillary sinus septa in the edentulous and dentate maxilla. J Oral Maxillofac Surg. 1999; 57:667–671. PMID:
10368090.
12. Underwood AS. An inquiry into the anatomy and pathology of the maxillary sinus. J Anat Physiol. 1910; 44(Pt 4):354–369. PMID:
17232856.
13. Lee WJ, Lee SJ, Kim HS. Analysis of location and prevalence of maxillary sinus septa. J Periodontal Implant Sci. 2010; 40:56–60. PMID:
20498761.
14. Maestre-Ferrín L, Carrillo-García C, Galán-Gil S, Peñarrocha-Diago M, Peñarrocha-Diago M. Prevalence, location, and size of maxillary sinus septa: panoramic radiograph versus computed tomography scan. J Oral Maxillofac Surg. 2011; 69:507–511. PMID:
21238847.
15. Velásquez-Plata D, Hovey LR, Peach CC, Alder ME. Maxillary sinus septa: a 3-dimensional computerized tomographic scan analysis. Int J Oral Maxillofac Implants. 2002; 17:854–860. PMID:
12507246.
16. González-Santana H, Peñarrocha-Diago M, Guarinos-Carbó J, Sorní-Bröker M. A study of the septa in the maxillary sinuses and the subantral alveolar processes in 30 patients. J Oral Implantol. 2007; 33:340–343. PMID:
18240793.
17. Bell GW, Joshi BB, Macleod RI. Maxillary sinus disease: diagnosis and treatment. Br Dent J. 2011; 210:113–118. PMID:
21311531.
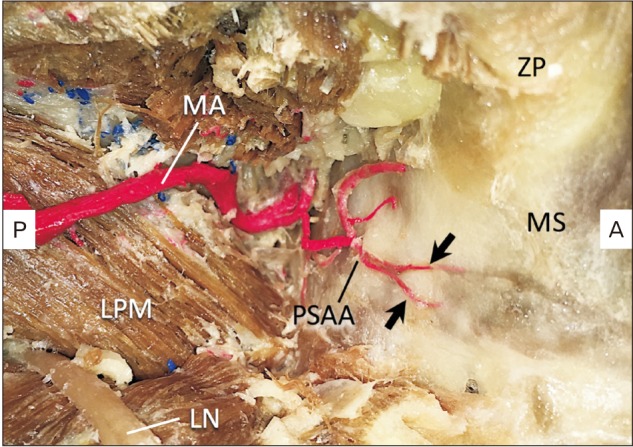
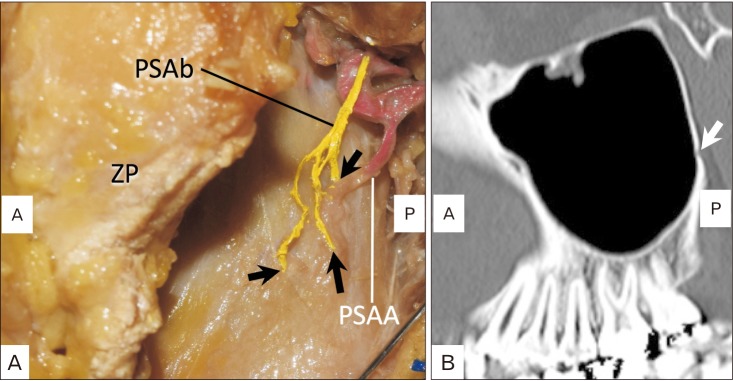
18. Kqiku L, Biblekaj R, Weiglein AH, Kqiku X, Städtler P. Arterial blood architecture of the maxillary sinus in dentate specimens. Croat Med J. 2013; 54:180–184. PMID:
23630145.
19. Flanagan D. Arterial supply of maxillary sinus and potential for bleeding complication during lateral approach sinus elevation. Implant Dent. 2005; 14:336–338. PMID:
16361882.
20. Lovasova K, Kachlik D, Rozpravkova M, Matusevska M, Ferkova J, Kluchova D. Three-dimensional CAD/CAM imaging of the maxillary sinus in ageing process. Ann Anat. 2018; 218:69–82. PMID:
29627610.
21. Gosau M, Rink D, Driemel O, Draenert FG. Maxillary sinus anatomy: a cadaveric study with clinical implications. Anat Rec (Hoboken). 2009; 292:352–354. PMID:
19248167.
22. Velasco-Torres M, Padial-Molina M, Avila-Ortiz G, García-Delgado R, O'Valle F, Catena A, Galindo-Moreno P. Maxillary sinus dimensions decrease as age and tooth loss increase. Implant Dent. 2017; 26:288–295. PMID:
28125519.
23. Paatero YV. Orthoradial jaw pantomography. Ann Med Intern Fenn Suppl. 1959; 48(Supp 28):222–227. PMID:
13637452.
24. Malina-Altzinger J, Damerau G, Grätz KW, Stadlinger PD. Evaluation of the maxillary sinus in panoramic radiography: a comparative study. Int J Implant Dent. 2015; 1:17. PMID:
27747639.
25. Bornstein MM, Scarfe WC, Vaughn VM, Jacobs R. Cone beam computed tomography in implant dentistry: a systematic review focusing on guidelines, indications, and radiation dose risks. Int J Oral Maxillofac Implants. 2014; 29(Suppl):55–77. PMID:
24660190.
26. Dula K, Benic GI, Bornstein M, Dagassan-Berndt D, Filippi A, Hicklin S, Kissling-Jeger F, Luebbers HT, Sculean A, Sequeira-Byron P, Walter C, Zehnder M. SADMFR guidelines for the use of cone-beam computed tomography/digital volume tomography. Swiss Dent J. 2015; 125:945–953. PMID:
26399521.
27. Maestre-Ferrín L, Galán-Gil S, Carrillo-García C, Peñarrocha-Diago M. Radiographic findings in the maxillary sinus: comparison of panoramic radiography with computed tomography. Int J Oral Maxillofac Implants. 2011; 26:341–346. PMID:
21483887.
28. Toraman Alkurt M, Peker I, Degerli S, Cebeci AR, Sadik E. Comparison of cone-beam computed tomography and panoramic radiographs in detecting maxillary sinus septa. J Istanb Univ Fac Dent. 2016; 50:8–14. PMID:
28955570.
29. Tehranchi M, Taleghani F, Shahab S, Nouri A. Prevalence and location of the posterior superior alveolar artery using cone-beam computed tomography. Imaging Sci Dent. 2017; 47:39–44. PMID:
28361028.
30. Chitsazi MT, Shirmohammadi A, Faramarzi M, Esmaieli F, Chitsazi S. Evaluation of the position of the posterior superior alveolar artery in relation to the maxillary sinus using the Cone-Beam computed tomography scans. J Clin Exp Dent. 2017; 9:e394–e399. PMID:
28298981.
31. Pandharbale AA, Gadgil RM, Bhoosreddy AR, Kunte VR, Ahire BS, Shinde MR, Joshi SS. Evaluation of the posterior superior alveolar artery using cone beam computed tomography. Pol J Radiol. 2016; 81:606–610. PMID:
28058075.
32. Danesh-Sani SA, Movahed A, ElChaar ES, Chong Chan K, Amintavakoli N. Radiographic evaluation of maxillary sinus lateral wall and posterior superior alveolar artery anatomy: a cone-beam computed tomographic study. Clin Implant Dent Relat Res. 2017; 19:151–160. PMID:
27238049.
33. Khojastehpour L, Dehbozorgi M, Tabrizi R, Esfandnia S. Evaluating the anatomical location of the posterior superior alveolar artery in cone beam computed tomography images. Int J Oral Maxillofac Surg. 2016; 45:354–358. PMID:
26516028.
34. Güncü GN, Yildirim YD, Wang HL, Tözüm TF. Location of posterior superior alveolar artery and evaluation of maxillary sinus anatomy with computerized tomography: a clinical study. Clin Oral Implants Res. 2011; 22:1164–1167. PMID:
21244499.
35. Ilgüy D, Ilgüy M, Dolekoglu S, Fisekcioglu E. Evaluation of the posterior superior alveolar artery and the maxillary sinus with CBCT. Braz Oral Res. 2013; 27:431–437. PMID:
24036981.
36. Solar P, Geyerhofer U, Traxler H, Windisch A, Ulm C, Watzek G. Blood supply to the maxillary sinus relevant to sinus floor elevation procedures. Clin Oral Implants Res. 1999; 10:34–44. PMID:
10196788.
37. Traxler H, Windisch A, Geyerhofer U, Surd R, Solar P, Firbas W. Arterial blood supply of the maxillary sinus. Clin Anat. 1999; 12:417–421. PMID:
10545857.
38. Maes JJ, Clement PA. The usefulness of irrigation of the maxillary sinus in children with maxillary sinusitis on the basis of the Water's X-ray. Rhinology. 1987; 25:259–264. PMID:
2448862.
39. Eley KA, Watt-Smith SR, Boland P, Potter M, Golding SJ. MRI pre-treatment tumour volume in maxillary complex squamous cell carcinoma treated with surgical resection. J Craniomaxillofac Surg. 2014; 42:119–124. PMID:
23777920.
40. Yuan XP, Li CX, Cao Y, Singh S, Zhong R. Inflammatory myofibroblastic tumour of the maxillary sinus: CT and MRI findings. Clin Radiol. 2012; 67:e53–e57. PMID:
22974570.
41. Ng SH, Chang TC, Ko SF, Yen PS, Wan YL, Tang LM, Tsai MH. Nasopharyngeal carcinoma: MRI and CT assessment. Neuroradiology. 1997; 39:741–746. PMID:
9351114.
42. Asaumi J, Konouchi H, Hisatomi M, Kishi K. Odontogenic myxoma of maxillary sinus: CT and MR-pathologic correlation. Eur J Radiol. 2001; 37:1–4. PMID:
11274831.
43. Yasumoto M, Taura S, Shibuya H, Honda M. Primary malignant lymphoma of the maxillary sinus: CT and MRI. Neuroradiology. 2000; 42:285–289. PMID:
10872174.
44. Gray CF, Redpath TW, Smith FW, Staff RT, Bainton R. Assessment of the sinus lift operation by magnetic resonance imaging. Br J Oral Maxillofac Surg. 1999; 37:285–289. PMID:
10475650.
45. Gray CF, Staff RT, Redpath TW, Needham G, Renny NM. Assessment of maxillary sinus volume for the sinus lift operation by three-dimensional magnetic resonance imaging. Dentomaxillofac Radiol. 2000; 29:154–158. PMID:
10849541.
46. Gray CF, Redpath TW, Bainton R, Smith FW. Magnetic resonance imaging assessment of a sinus lift operation using reoxidised cellulose (Surgicel) as graft material. Clin Oral Implants Res. 2001; 12:526–530. PMID:
11564114.
47. Senel FC, Duran S, Icten O, Izbudak I, Cizmeci F. Assessment of the sinus lift operation by magnetic resonance imaging. Br J Oral Maxillofac Surg. 2006; 44:511–514. PMID:
16540215.
48. Lim D, Parumo R, Chai MB, Shanmuganathan J. Transnasal endoscopy removal of dislodged dental implant: a case report. J Oral Implantol. 2017; 43:228–231. PMID:
27996585.
49. Jeong KI, Kim SG, Oh JS, You JS. Implants displaced into the maxillary sinus: a systematic review. Implant Dent. 2016; 25:547–551. PMID:
26974033.
50. Matti E, Emanuelli E, Pusateri A, Muniz CC, Pagella F. Transnasal endoscopic removal of dental implants from the maxillary sinus. Int J Oral Maxillofac Implants. 2013; 28:905–910. PMID:
23748326.
51. Andreasi Bassi M, Andrisani C, Lico S, Ormanier Z, Barlattani A Jr, Ottria L. Endoscopic management of the schneiderian membrane perforation during transcrestal sinus augmentation: a case report. Oral Implantol (Rome). 2016; 9:157–163. PMID:
28042444.
52. Zheng J, Zhang S, Lu E, Yang C, Zhang W, Zhao J. Endoscopic lift of the maxillary sinus floor in Beagles. Br J Oral Maxillofac Surg. 2014; 52:845–849. PMID:
25174319.
53. Kunihiro T, Araki Y, Oba T. Minimally invasive endoscopic middle meatal antrostomy for the prevention of maxillary sinusitis in association with dental implantation in the posterior maxilla: a proposal. Fukuoka Igaku Zasshi. 2014; 105:182–189. PMID:
25639025.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download