Abstract
To address the problems associated with crowding in dissection laboratory, especially for dissections of the head and neck region, we adopted an alternate dissection strategy and explored its effects on student learning, and student perceptions of the approach. The alternate dissection approach was first introduced at our institution for dissection of the head and neck region in 2014, and was expanded to encompass the extremities in 2016. A survey on student perceptions of this new strategy was conducted at the end of anatomical courses held from 2014 to 2016, and practical and written examination scores from 2013 to 2016 were analyzed. The results showed that student perceptions were largely positive and became increasingly so each year. However, there was still some anxiety among the students regarding regions that they did not dissect themselves. Despite this, the alternate dissection strategy did not influence practical examination scores, with the exception of a transient decrease in 2014, i.e., the first year of implementation. Moreover, written examination scores improved both for the extremities and the head and neck regions in 2016. The alternate dissection strategy described herein solved the crowding problem in the dissection laboratory at our institution and had no negative effects on student learning outcomes. Therefore, this type of approach can be used to improve efficiency in dissection laboratories.
Anatomy is undoubtedly a cornerstone of medical education. Cadaver dissection is an important tool for learning anatomy, especially with respect to the three-dimensional organization of the human body [123456], and is thus regarded as the most important source of anatomical knowledge for students [7], as well as surgeons [8] and residents [9].
Over the past few decades, the medical education paradigm has evolved to focus on problem-based, studentcentered, integrated, and clinical competency-accentuated approaches [10]. Accordingly, the time spent acquiring a basic science education has been markedly reduced [111213]. Compared to 30 years ago, in 2009 in Korea, the amount of time devoted to anatomy lectures was 67% lower, while that spent in the dissection laboratory was 54% lower [1415]. Specifically, the lecture time decreased from 96±26 to 65±34 hours, and the dissection laboratory time from 155.6±50.0 to 85±47 hours [1415]. In addition to this reduced time, the increased content that must now be learnt due to advances in fields such as molecular biology, genetics, and bioinformatics leaves students feeling overwhelmed during anatomy lectures and dissections.
Another problem specific to our institution, in addition to those mentioned above, is crowding in the dissection laboratory. Eight students are assigned to a table, which is reasonable for dissection of the extremities, but is very crowded for dissection of the head and neck due to the relatively small area of this region. Under such conditions, equal participation of every student cannot be guaranteed, so certain students are frequently excluded from dissection practice regardless of their intentions. This could be solved either by increasing the dissection time or the number of cadavers used. However, these solutions are not feasible because of the above-mentioned issues and the restricted supply of cadavers.
Another possible solution is alternate dissection (hereafter abbreviated as AD), in which students are divided into two or three teams that take turns participating in the dissection laboratory. This kind of strategy has previously been adopted by some medical schools to reduce course time [1617], resolve issues associated with class size and a high student-to-body and/or student-to-faculty ratio [181920], or accommodate curricular changes [21]. Thus, we adopted this strategy in 2014 with the expectation that it would improve the dissection learning environment. However, we had some concerns since the opportunity for each student to participate in a hands-on dissection, which is one of the best ways to obtain anatomy skills, was decreased [722]. Furthermore, studies of the effects of AD on written examination scores showed somewhat conflicting results, including decreases [23], no changes [2024] or improvements [18]. These differing results caused us concern regarding the potential negative effects of AD on student learning outcomes.
In this study, we evaluated the effects of AD on student examination scores, as well as their perceptions of the approach.
Seoul National University College of Medicine operated two MD programs: a 6-year undergraduate entry program (UEP) and a 4-year graduate entry program (GEP). The number of students included in this study per year was around 155 (Table 1). The overall percentage of male students was 65.8% and 66.0% of the students were enrolled in the UEP. The Gross Anatomy course consisted of 48 of 50-minute lectures and 28 of 4-hour laboratory classes held over the first 12 weeks of the first year of a 4-year medical curriculum. The 28 laboratory classes consisted of 10 extremity region sessions, nine trunk region sessions (including the thorax, abdomen, and pelvis), and nine head and neck region sessions. Throughout the laboratory classes, one cadaver was assigned to each group of eight students. The content and progression schedule for each dissection laboratory were pre-determined and announced to the students. Dissections were usually preceded by lectures on the corresponding anatomical regions. During dissection, four to five faculty members circulated around the room and help the students perform the dissections according to the dissection guide book.
In 2014 and 2015, AD was introduced for dissection of the head and neck region following completion of dissections of the extremities and trunk regions in the traditional manner. For AD, eight students were divided into teams A and B, each consisting of four members. Team A performed the dissection first, while members of team B had free time. During the next dissection, team A explained to their colleagues what they had done in the previous laboratory session, for 15–20 minutes, and team B continued the dissection while team A had free time. In the next dissection, team B explained what they had done during the previous dissection before team A continued the dissection. In 2016, AD was expanded to encompass dissection of the extremities based on its positive reception in the previous years.
The practical and written examination data from 2013 to 2016 were collected and analyzed. The practical examination included 40 specimen-based questions on the names and characteristics of anatomical structures. The written examination was composed of a variety of questions, including multiple choice, single-answer, fill-in-the-blank, and essay questions. Written and practical examinations were performed by students immediately after lectures and dissections. With the exception of 2014 (when the examination was completed only at midterm and at the end of term), the written examination was assigned three times per year. It was not possible to obtain scores for all anatomical regions in 2014, so the written examination results for that year were excluded from the analysis. The scores were compared to those the year before AD was implemented (2013) by one-way ANOVA. SPSS for Windows software version 22.0 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses.
After AD was introduced, we conducted a five-item survey at the end of the Gross Anatomy course to evaluate student opinions of AD. In 2016, two more items—“I made good use of the allocated free time” and “I agree with maintaining (or introducing) alternate cadaver dissection for the following anatomical regions”—were added. The response rate for the survey was 83.8% (130/155), 64.1% (102/159), and 78.6% (114/145) in 2014, 2015, and 2016, respectively.
We first analyzed the examination scores. Since there was no significant difference in scores according to sex or program type (UEP vs. GEP) (data not shown), we did not divide the students into groups. For the practical examinations (Table 2), the mean score for the head and neck region in 2014, the first year of AD implementation, was significantly lower than that for the previous year (66.0±13.9 vs. 73.6±14.6). However, the scores in 2015 and 2016, the second and third years of AD implementation, were comparable to those of 2013. There were no differences between the practical examination scores for the extremities in 2016 compared to those of other years, suggesting that AD had no effect on learning.
For the written examinations (Table 3), both the head and neck and extremities scores improved after the introduction of AD. The written examination scores for the extremities in 2016 were significantly higher than those in 2013 and 2015. Similarly, the written examination scores for the head and neck region for 2015 and 2016 were significantly higher than those for 2013.
Next, we analyzed student perceptions of AD (Tables 4, 5). In contrast to the examination scores, about half of the students reported either modest or significant difficulty when studying anatomy (Q1) or preparing for the practical examination (Q2) due to the AD approach. However, this negative perception had somewhat improved by 2016. Interestingly, the percentage of those who selected the response option of “significant” decreased to 1.8% both for Q1 and Q2 in 2016. Regarding the peer explanation (Q3) and overall satisfaction with AD (Q4) items, less than 20% of the students responded negatively, and the perception became more positive every year. The proportion of positive answers (including “strongly agree” and “agree”) for Q4 showed an increasing trend, being 65.4%, 68.4%, and 81.0% in 2014, 2015, and 2016, respectively.
In 2016, most of the students answered that they made good use of the free time given to them when they did not attend the dissection laboratory (Q5; mean score of 4.16 out of 5). In addition, most students agreed that the AD strategy should be maintained for the extremities (86.3%) and head and neck regions (83.5%) (Q6). However, only 56% of the students agreed that AD should also be applied for the trunk region.
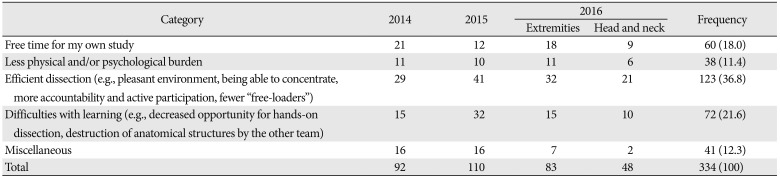
We also asked the students to submit positive or negative comments regarding AD. Student comments were categorized and are presented in Table 6. The positive feedback regarding AD included the provision of additional free time to study on their own (18.0% of all comments) and the decreased physical and mental burden associated with attendance of the cadaver dissection (11.4% of all comments). The most well-represented comment category was “efficient dissection environment” (36.8% of all comments). The most frequently cited factor that rendered the dissection laboratory more efficient was the small number of participating students, which meant that the students could concentrate, be heard, and actively participate in the dissection to a greater extent, resulting in fewer passive participators.
The largest proportion of negative comments pertained to learning efforts being hindered (21.6% of all comments); specifically, students could not fully understand the anatomy of the regions that they did not dissect themselves, and they did not observe structures dissected by team members. Students also had a negative opinion about the unfair division of tasks between teams.
In this study, we explored the effect of AD on student academic achievement, as well as student perceptions of AD. We were concerned that the decrease in dissection hours would have a negative impact on learning. Even though there was a transient decrease in the practical examination scores in the first year of AD implementation, scores recovered to previous levels from the second year on. Furthermore, written examination scores tended to improve each year, both for the extremities and the head and neck regions. Students reported positive opinions of various aspects of the new approach, including the provision of free time, reduced physical and mental burden, and effective dissection classes, although many students also reported experiencing anxiety regarding the regions they did not dissect themselves.
In our institution, AD was introduced to solve crowding and other problems in the dissection laboratory. Overall, students had a positive reaction to AD. In 2016, most students preferred AD (80.1%) and were satisfied with the peer explanation aspect of the approach (82.6%) (Table 5). Overall, 86.3% and 83.5% of students agreed that this strategy should be maintained for the dissection of the extremities and head and neck regions. This positive perception of the AD approach seemed to be due to the “less crowded environment” that it engendered. One previous study reported that when there were three to four students per table, 88% of them felt that the table was not crowded, while 83% felt the number was sufficiently low for efficient dissection [20]. Our students also cited “efficiency” in the dissection laboratory as a major advantage of AD. This efficiency manifested in improved ability to concentrate, and a more responsible, cooperative, and actively participating team (Table 6). The students attributed this improved efficiency to the lack of crowding. Thus, introduction of AD in our institution seems to have been successful in solving crowding problems.
Unfortunately, many students still felt either modestly or significantly uncomfortable (Table 4) about the anatomical regions that they did not dissect themselves. About 20% of comments alluded to “difficulty in learning” about structures the students did not dissect themselves. This anxiety is likely due to our students believing that hands-on dissection is the most important pathway to anatomical knowledge [7]. Similar results were also reported by other studies [172023], which implies that this negative feeling is common across cultures.
However, in contrast to what some students anticipated, examination scores either remained stable or improved following the introduction of AD: AD had minimal influence on practical examination scores, except for a transient decrease in the first year of implementation. Likewise, other studies of AD reported no changes in practical examination scores in various contexts [182023]. In contrast, Marshak et al. [24] found that practical examination scores were increased for regions that students dissected themselves compared to those that they did not dissect. However, the difference was less than 1 point (mean scores for all 50 questions: 80.0±13.0 vs. 78.3±14.1 for regions dissected and not dissected by students themselves, respectively) and lacked statistical significance. These results seem to support the assertion of Yeager [16] that dissecting only half of the body may be sufficient for students to acquire a basic understanding of anatomy.
As for the transient decrease of the score in 2014, it might be an example of “performance dip” that sometimes occurs following a change in curriculum or program [25]. In 2014, not only the scores, but also their mean scores for the preference to AD and the satisfaction to the peer explanation were significantly lower than those in 2015 and 2016. These results mean that the first year students had no time to adapt the new approach, while students in 2015 and 2016 adapted. One of the possible factors that contributed to the adaptation and improved responses in these years of AD might be close relationship between junior and senior students frequently found in Confucian culture [26] including our institution. Certainly those students who have experienced AD should have provided the know-how to utilize the system to their junior students. That is what usually happens in Korean medical schools. Similarly, it has been also reported that the performance difference between dissectors and non-dissectors decreased as the students' familiarity with the new method increased [19].
Interestingly, written examination scores improved in 2015 and 2016 compared to those in 2013, both for the extremities and the head and neck region (Table 3). These results helped to alleviate student anxiety, but contradict those of other studies reporting that scores were decreased [23] or showed no change after the introduction of AD [2024]. One study also reported significantly improved written examination scores after AD implementation [18], which was attributed to the students being able to study when not participating in the dissection. In that study, 20 students were assigned to a cadaver before AD implementation, such that many students were forced to passively participate in the dissection; once AD was introduced, the 10 students not participating in the dissection were free to study on their own. In our case, given that there was no adjustment of the examination questions during the study period, the improved written examination scores were likely due to the increased study time given to the students. “Free time” was cited by the students as a positive aspect of AD (in 18% of all comments) (Table 6), and 87.4% of the students agreed or strongly agreed that they made good use of this additional time (Tables 4, 5).
There were some limitations to this study. Previous research suggests that hands-on dissection is more helpful for retaining knowledge than studying an already dissected cadaver [16]. In our study, we did not evaluate the long-term effects of the reduced opportunity for hands-on dissection. Particularly, it is even more so in the case of extremities, in that we used only 1-year data, those of year 2016, to compare before and after the change. However, these data should be available shortly. AD also includes elements of peer teaching. In our case, students provided teaching to other team members for 15–20 minutes at the beginning of the dissection, with respect to what they had done in the previous laboratory session. Although some authors disregard this reciprocal peer teaching [20], others insist that it has beneficial effects [2728]. It is also possible that the effects of AD observed herein could have been intermixed with those of reciprocal peer teaching, even though the time allocated for peer explanations was relatively limited. However, we did not evaluate this in our study, such that the effect of peer teaching in the context of AD needs to be further explored. It may be desirable to devise a more organized way of delivering peer teaching, given that a structured format facilitates better transfer of information [29].
In summary, our new dissection strategy solved the crowding problem in the dissection laboratory at our institution and had no negative effects on student learning outcomes, which lead to the conclusion that this type of approach can be used to improve efficiency in dissection laboratories.
Acknowledgements
The authors acknowledge the all students who agreed to participate in the course and study. This work was supported by the Education and Research Encouragement Fund of Seoul National University Hospital (2018).
References
1. Marks SC Jr. The role of three-dimensional information in health care and medical education: the implications for anatomy and dissection. Clin Anat. 2000; 13:448–452. PMID: 11111898.
2. Granger NA. Dissection laboratory is vital to medical gross anatomy education. Anat Rec B New Anat. 2004; 281:6–8. PMID: 15558779.
3. Rizzolo LJ, Stewart WB. Should we continue teaching anatomy by dissection when...? Anat Rec B New Anat. 2006; 289:215–218. PMID: 17109419.
4. Korf HW, Wicht H, Snipes RL, Timmermans JP, Paulsen F, Rune G, Baumgart-Vogt E. The dissection course: necessary and indispensable for teaching anatomy to medical students. Ann Anat. 2008; 190:16–22. PMID: 18342138.
5. Papa V, Vaccarezza M. Teaching anatomy in the XXI century: new aspects and pitfalls. ScientificWorldJournal. 2013; 2013:310348. PMID: 24367240.
6. Pizzimenti MA, Pantazis N, Sandra A, Hoffmann DS, Lenoch S, Ferguson KJ. Dissection and dissection-associated required experiences improve student performance in gross anatomy: Differences among quartiles. Anat Sci Educ. 2016; 9:238–246. PMID: 26536279.
7. Cho MJ, Hwang YI. Students' perception of anatomy education at a Korean medical college with respect to time and contents. Anat Cell Biol. 2013; 46:157–162. PMID: 23869263.
8. Sheikh AH, Barry DS, Gutierrez H, Cryan JF, O'Keeffe GW. Cadaveric anatomy in the future of medical education: What is the surgeons view? Anat Sci Educ. 2016; 9:203–208. PMID: 26213365.
9. Fillmore EP, Brokaw JJ, Kochhar K, Nalin PM. Understanding the current anatomical competence landscape: comparing perceptions of program directors, residents, and fourth-year medical students. Anat Sci Educ. 2016; 9:307–318. PMID: 26632977.
10. Association of American Medical Colleges. Physicians for the twenty-first century. The GPEP report: report of the panel on the general professional education of the physician and college preparation for medicine [Internet]. Washington, DC: Association of American Medical Colleges;1984. cited 2017 Nov 30. Available from: http://files.eric.ed.gov/fulltext/ED252102.pdf.
11. Gartner LP. Anatomical sciences in the allopathic medical school curriculum in the United States between 1967-2001. Clin Anat. 2003; 16:434–439. PMID: 12903066.
12. Drake RL, McBride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ. 2009; 2:253–259. PMID: 19890982.
13. Craig S, Tait N, Boers D, McAndrew D. Review of anatomy education in Australian and New Zealand medical schools. ANZ J Surg. 2010; 80:212–216. PMID: 20575945.
14. Hwang YI. Analysis of anatomy education in Korean medical schools. In : Proceedings of the 59th Annual Meeting of Korean Association of Anatomists; 2009 Oct 22-23; Daegu, Korea. Seoul: Korean Association of Anatomists;2009. p. 53.
15. Lee WB, Baik SH. Analysis of anatomy curricula of twenty-nine medical colleges in Korea. Korean J Med Educ. 1990; 2:42–50.
16. Yeager VL. Learning gross anatomy: dissection and prosection. Clin Anat. 1996; 9:57–59. PMID: 8838283.
17. Johnson JH. Importance of dissection in learning anatomy: personal dissection versus peer teaching. Clin Anat. 2002; 15:38–44. PMID: 11835543.
18. Nnodim JO. A controlled trial of peer-teaching in practical gross anatomy. Clin Anat. 1997; 10:112–117. PMID: 9058018.
19. Sandra A, Ferguson KJ. Analysis of gross anatomy laboratory performance using a student dissection/presentation teaching method. Teach Learn Med. 1998; 10:158–161.
20. Bentley BS, Hill RV. Objective and subjective assessment of reciprocal peer teaching in medical gross anatomy laboratory. Anat Sci Educ. 2009; 2:143–149. PMID: 19637291.
21. McWhorter DL, Forester JP. Effects of an alternate dissection schedule on gross anatomy laboratory practical performance. Clin Anat. 2004; 17:144–148. PMID: 14974103.
22. Kerby J, Shukur ZN, Shalhoub J. The relationships between learning outcomes and methods of teaching anatomy as perceived by medical students. Clin Anat. 2011; 24:489–497. PMID: 20949485.
23. Granger NA, Calleson D. The impact of alternating dissection on student performance in a medical anatomy course: are dissection videos an effective substitute for actual dissection? Clin Anat. 2007; 20:315–321. PMID: 16795027.
24. Marshak DW, Oakes J, Hsieh PH, Chuang AZ, Cleary LJ. Outcomes of a rotational dissection system in gross anatomy. Anat Sci Educ. 2015; 8:438–444. PMID: 25358463.
25. Bland CJ, Starnaman S, Wersal L, Moorehead-Rosenberg L, Zonia S, Henry R. Curricular change in medical schools: how to succeed. Acad Med. 2000; 75:575–594. PMID: 10875502.
26. Ho MJ, Lin CW, Chiu YT, Lingard L, Ginsburg S. A cross-cultural study of students' approaches to professional dilemmas: sticks or ripples. Med Educ. 2012; 46:245–256. PMID: 22324524.
27. Bruno PA, Love Green JK, Illerbrun SL, Holness DA, Illerbrun SJ, Haus KA, Poirier SM, Sveinson KL. Students helping students: Evaluating a pilot program of peer teaching for an undergraduate course in human anatomy. Anat Sci Educ. 2016; 9:132–142. PMID: 26060978.
28. Manyama M, Stafford R, Mazyala E, Lukanima A, Magele N, Kidenya BR, Kimwaga E, Msuya S, Kauki J. Improving gross anatomy learning using reciprocal peer teaching. BMC Med Educ. 2016; 16:95. PMID: 27000752.
29. Weiss MJ, Bhanji F, Fontela PS, Razack SI. A preliminary study of the impact of a handover cognitive aid on clinical reasoning and information transfer. Med Educ. 2013; 47:832–841. PMID: 23837430.
Table 1
Student characteristics
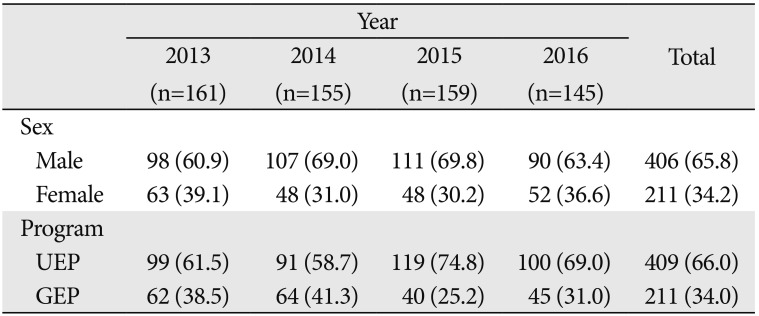
Table 2
Comparison of student practical examination scores among years
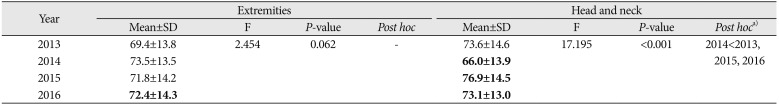
Table 3
Comparison of written examination scores among years
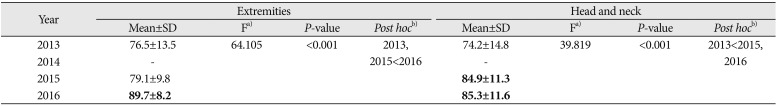
Bold letters denote examinations that were taken after implantation of the alternate dissection approach. Scores for 2014 (i.e., the year in which the written examination was completed twice instead of three times, were excluded from the analysis. a)Welch's F-test. b)A Games-Howell test was used to analyze data with unequal variance.
Table 4
Student attitudes towards alternate cadaver dissection: Q1 and Q2
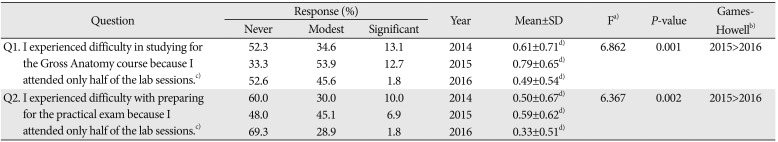
Table 5
Student attitudes towards alternate cadaver dissection: Q3–Q6
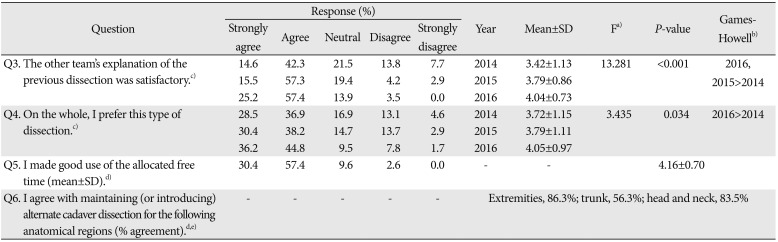
Table 6
Positive and negative comments made by students regarding alternate dissection




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download