This article has been
cited by other articles in ScienceCentral.
Abstract
This study investigated and classified the various types of moderator band (MB) in relation to the anterior papillary muscle, with the aim of providing anatomical reference information and fundamental knowledge for use when repairing the congenital defects and understanding the conduction system. The study investigated 38 formalin-fixed human hearts of both sexes obtained from donors aged 38–90 years. The MB was evident in 36 of the 38 specimens (94.7%). The morphology of the MB and its connection with the APM took various forms. The MBs that had a distinct shape were classified into three types according to their shape: cylindrical column, long and thin column, and wide and flat column. Types 2 and 3 were the most common, appearing in 15 (41.7%) and 14 (38.9%) of the 36 specimens, respectively, while type 1 was observed in seven specimens (19.4%). Type 3 was divided into subtypes based on their length. The MB usually originated from a single root (91.7%), with the remainder exhibiting double roots. The pairs of roots in the latter cases had different shapes. The originating point of the MB ranged from the supraventricular crest to the apex of the ventricle. The most-common originating point was in the middle (25 of 36 specimens, 69.4%), followed by the upper third (13.9%), the lower third (11.1%), and the top fifth (5.6%) of the interventricular septum. This study has produced fundamental anatomical and clinical information that will be useful when designing cardiac surgical procedures.
Go to :

Keywords: Moderator band, Right ventricle, Anterior papillary muscle, Conduction system
Introduction
The moderator band (MB, also known as the septomarginal trabecula) found in all human hearts is derived from the muscle band of the interventricular septum, begins below the septal end of the supraventricular crest, and runs toward the anterolateral wall of the ventricle [
1]. The role of the MB as part of the conduction system of the heart involves the right atrioventricular bundle, since conduction cardiomyocytes move toward the apex of the ventricle before entering the anterior papillary muscle (APM) [
2].
Several anatomical studies that have investigated the shape of the MB [
134567] have revealed that the MB takes various forms. It has been reported that an anomalous MB has clinical significance in the double-chamber right ventricle and in atrial and ventricular septal defects [
389101112]. Large apical muscular ventricular septal defects, especially those located just beneath the MB with a poorly defined muscular rim, were considered suitable for the sandwich technique [
11]. The MB and the multiple trabeculations beneath it create a multiperforated wall that hides the apical muscular ventricular septal defect in a transtricuspid view [
12].
This study investigated and classified the various types of MB in relation to the APM, with the aim of providing anatomical reference information and fundamental knowledge for use when repairing the congenital defects and understanding the conduction system.
Go to :

Materials and Methods
The study investigated 38 formalin-fixed human hearts of both sexes obtained from donors aged 38–90 years (23 males, 15 females; mean age, 67.4 years). To observe the MB, an incision was made from the apex of the right ventricle, along its medial and lateral margins, to the tricuspid valve. After opening the right ventricle, the MB, APM, and their adjacent structures were carefully inspected.
The location of the MB was observed from the interventricular septum to the inferior border of the anterior wall in the right ventricle. The relationship of the MB with the APM was observed, and we measured the length and thickness of the MB using digital calipers (Mitutoyo, Kawasaki, Japan).
Go to :

Results
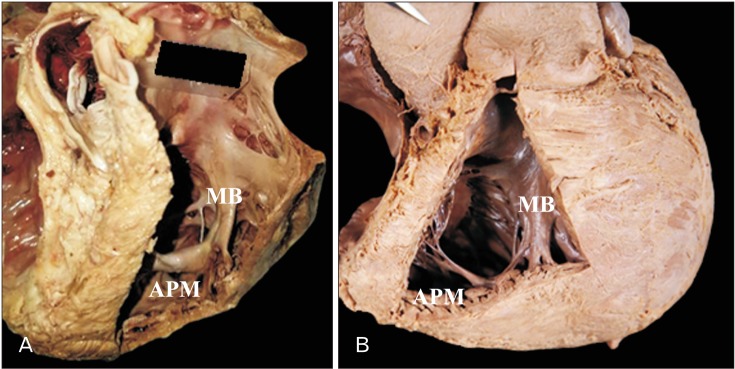
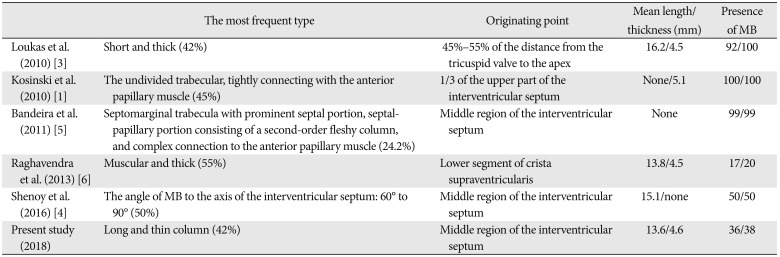
The MB was evident in 36 of the 38 specimens (94.7%). The morphology of the MB and its connection with the APM took various forms. The MBs that had a distinct shape were classified into three types according to their shape: (1) cylindrical column, (2) long and thin column, and (3) wide and flat column (
Fig. 1). Types 2 and 3 were the most common, appearing in 15 (41.7%) and 14 (38.9%) of the 36 specimens, respectively, while type 1 was observed in seven specimens (19.4%). Type 3 was divided into subtypes based on their length (
Table 1).
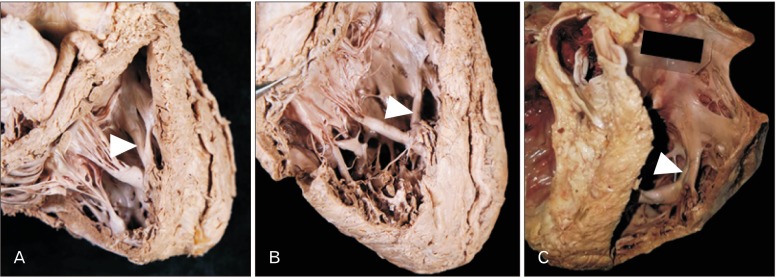 | Fig. 1Morphological classification of the moderator band (arrowheads). (A) Cylindrical column type. (B) Long and thin column type. (C) Wide and flat column type.
|
Table 1
Morphological classification of the MB
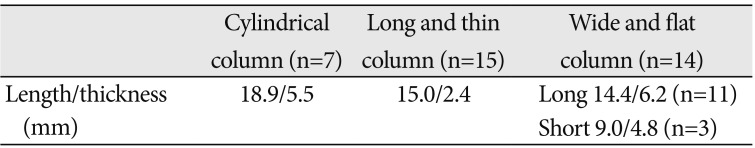
|
Cylindrical column (n=7) |
Long and thin column (n=15) |
Wide and flat column (n=14) |
|
Length/thickness (mm) |
18.9/5.5 |
15.0/2.4 |
Long 14.4/6.2 (n=11) |
|
Short 9.0/4.8 (n=3) |

The mean overall length and thickness of the MB were 13.6 mm and 4.6 mm, respectively; these values in types 1, 2, and 3 were 18.9 mm and 5.5 mm, 15.0 mm and 2.4 mm, and 12.7 mm and 5.9 mm, respectively.
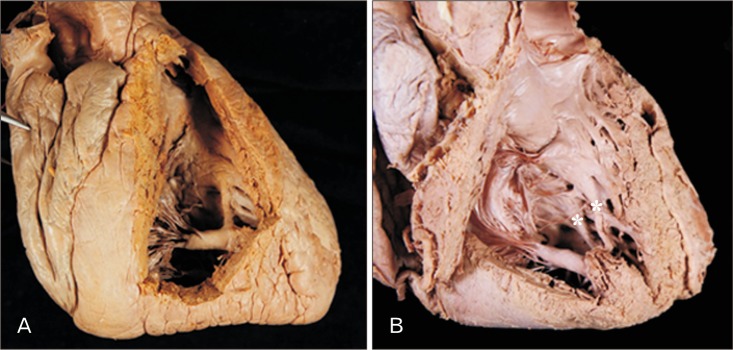
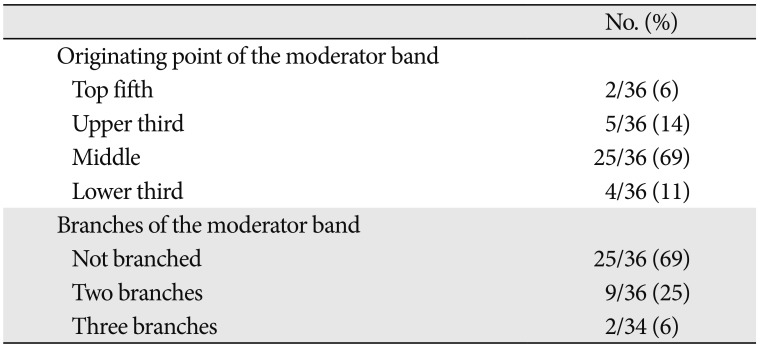
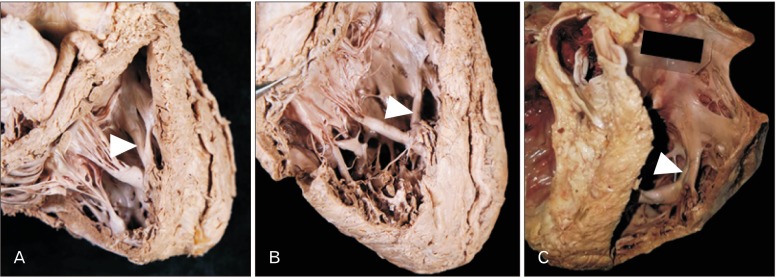
The MB usually originated from a single root (33 of 36 specimens, 91.7%), with the remainder exhibiting double roots (
Fig. 2). The pairs of roots in the latter cases had different shapes. The originating point of the MB ranged from the supraventricular crest to the apex of the ventricle. The most-common originating point was in the middle (25 of 36 specimens, 69.4%), followed by the upper third (5 of 36 specimens, 13.9%), the lower third (4 of 36 specimens, 11.1%), and the top fifth (2 of 36 specimens, 5.6%) of the interventricular septum (
Table 2).
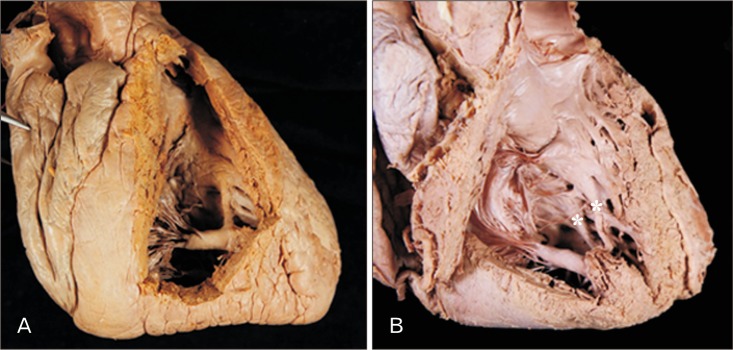 | Fig. 2Two types of roots of the moderator band (MB). (A) The MB usually originated from a single root. (B) A specimen that originated from double roots (asterisks).
|
Table 2
Originating point of the moderator band and branches of the moderator band
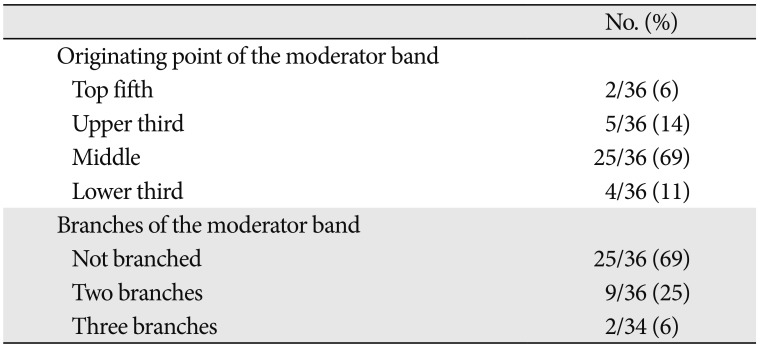
|
No. (%) |
|
Originating point of the moderator band |
|
|
Top fifth |
2/36 (6) |
|
Upper third |
5/36 (14) |
|
Middle |
25/36 (69) |
|
Lower third |
4/36 (11) |
|
Branches of the moderator band |
|
|
Not branched |
25/36 (69) |
|
Two branches |
9/36 (25) |
|
Three branches |
2/34 (6) |

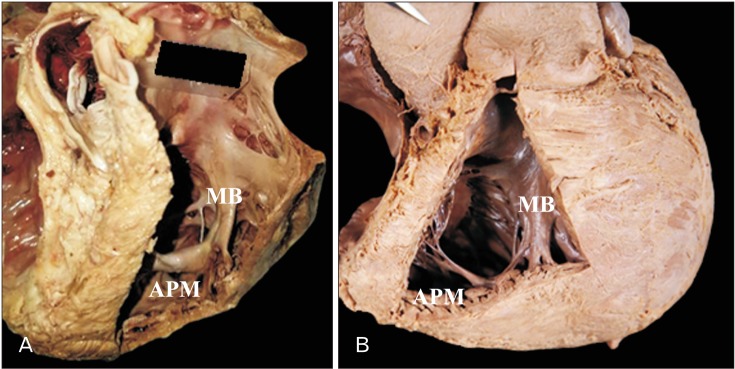
The MB was always attached to the APM in all but two specimens, in which it was attached to the anterior wall directly. The anterior papilla was present and distinctive in these two specimens. In 11 specimens (30.6%), the MB was divided into either 2 branches (9 specimens) or 3 branches (2 specimens) before it attached to the anterior wall of the right ventricle as well as the APM (
Table 2,
Fig. 3). In one of these specimens, most of the branches of the MB ran toward the anterior wall and the APM was surrounded by the MB.
 | Fig. 3Branches of the moderator band (MB). The MB sometimes divided into two branches (A) or three branches (B) before attaching to the anterior wall of the right ventricle as well as the anterior papillary muscle (APM).
|
Go to :

Discussion
This study has provided morphological and morphometric data on the MB that can be useful when repairing apical ventricular septal defects as well as for understanding the contraction of the right ventricle and closure of the tricuspid valve.
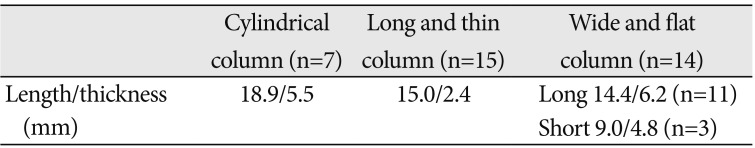
Previous studies have observed many diverse forms of the MB with different lengths and widths, and several morphological classifications of the MB with several subtypes have been defined (
Table 3) [
134567]. The present study also found, there were several types of the MB, despite its small size. A long and thin column type was the most common in the present study (41.7% of cases), which contrasts with a short and thick type being the most frequent in a previous study (45% of cases) [
1].
Table 3
Comparison of anatomical features of the MB between previous studies and the present study
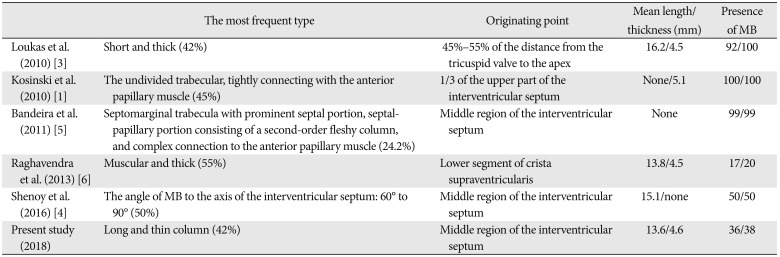
|
The most frequent type |
Originating point |
Mean length/thickness (mm) |
Presence of MB |
|
Loukas et al. (2010) [3] |
Short and thick (42%) |
45%–55% of the distance from the tricuspid valve to the apex |
16.2/4.5 |
92/100 |
|
Kosinski et al. (2010) [1] |
The undivided trabecular, tightly connecting with the anterior papillary muscle (45%) |
1/3 of the upper part of the interventricular septum |
None/5.1 |
100/100 |
|
Bandeira et al. (2011) [5] |
Septomarginal trabecula with prominent septal portion, septalpapillary portion consisting of a second-order fleshy column, and complex connection to the anterior papillary muscle (24.2%) |
Middle region of the interventricular septum |
None |
99/99 |
|
Raghavendra et al. (2013) [6] |
Muscular and thick (55%) |
Lower segment of crista supraventricularis |
13.8/4.5 |
17/20 |
|
Shenoy et al. (2016) [4] |
The angle of MB to the axis of the interventricular septum: 60° to 90° (50%) |
Middle region of the interventricular septum |
15.1/none |
50/50 |
|
Present study (2018) |
Long and thin column (42%) |
Middle region of the interventricular septum |
13.6/4.6 |
36/38 |

The MB was unclear or absent in 5.3% of the present cases, while Loukas et al. [
3] reported that they were unable to identify the MB in 8% of Caucasian cadavers, and Raghavendra et al. [
6] reported that the MB was not visible in 15% of Indian cadavers. These observations suggest that the MB is not always distinctive in all specimens.
The function of the MB is to contract the APM to prevent the tricuspid regurgitation through tension of the chordae tendineae. When the MB is abnormally thick or enlarged, it might block the flow to the pulmonary trunk, and this could be the reason for a double-chamber right ventricle or an apical ventricular septal defects [
39101112]. Therefore, if the MB is removed during the surgical repair of an apical ventricular septal defect, this could adversely affect the contraction of APM or the normal role of the chordae tendineae inserted into the anterior and posterior tricuspid valve leaflets. The present study further demonstrates that attention should be paid to the various shapes of the MB, since this structure forms a crucial part of the conduction system and so may have major clinical consequences when it comes to congenital abnormalities.
Raghavendra et al. [
6] found septoparietal trabeculations extending from the anterior margin of the MB to the parietal wall in five of 20 specimens, and multiple minor trabeculations extending from the MB in many specimens. Branched MBs were also found in the present study, with two branches in nine specimens and three branches in two specimens. In these specimens the septoparietal trabeculation might carry part of the right branch of the atrioventricular bundle of the conduction system. It is therefore thought that the septoparietal trabeculation forwarding to the anterior wall also requires careful consideration.
The MB did not emerge toward the APM in two specimens, instead being attached to the anterior wall. Such cases were found previously in children and fetuses [
1], while they occurred in adults in the present study.
The mean overall length and thickness of the MB were 13.6 mm and 4.6 mm, respectively, which are consistent with previously reported values of 16.2 mm and 4.5 mm [
3], and 13.8 mm and 4.5 mm [
6]. The results of the present study are therefore consistent with previous findings.
This study has produced fundamental anatomical and clinical information that will be useful when designing cardiac surgical procedures. We hope that our new anatomical data will help anatomists, radiologists, cardiac surgeons, and physicians.
Go to :

Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2016R1D1A1B03930402). This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP; Ministry of Science, ICT & Future Planning) (NRF-2017R1C1B5075725).
Go to :

References
1. Kosiński A, Kozłowski D, Nowiński J, Lewicka E, Dabrowska-Kugacka A, Raczak G, Grzybiak M. Morphogenetic aspects of the septomarginal trabecula in the human heart. Arch Med Sci. 2010; 6:733–743. PMID:
22419933.
2. Standring S. Gray's Anatomy: the anatomical basis of clinical practice. 41st ed. Philadelphia, PA: Elsevier Churchill Livingstone;2016.
3. Loukas M, Klaassen Z, Tubbs RS, Derderian T, Paling D, Chow D, Patel S, Anderson RH. Anatomical observations of the moderator band. Clin Anat. 2010; 23:443–450. PMID:
20235167.
4. Shenoy P, Lucas M, Vinay KV, Ramos A. Morphometric study of septomarginal trabeculae (moderator band). Int J Anat Res. 2016; 4:3302–3308.
5. Bandeira ST, Wafae GC, Ruiz C, Nascimento SR, Fernandes JR, Wafae N. Morphological classification of the septomarginal trabecula in humans. Folia Morphol (Warsz). 2011; 70:300–304. PMID:
22117250.
6. Raghavendra AY, Kavitha , Kumar A, Tarvadi P, Harsha CR. Anatomical study of the moderator band. Nitte Univ J Health Sci. 2013; 3:78–81.
7. Kosiński A, Nowiński J, Kozlowski D, Piwko G, Kuta W, Grzybiak M. The crista supraventricularis in the human heart and its role in the morphogenesis of the septomarginal trabecula. Ann Anat. 2007; 189:447–456. PMID:
17910398.
8. Wu MC, Ku PM, Chou MC, Huang TY. Usefulness of 64-slice computed tomography for evaluation of double-chambered right ventricle combined with atrial and ventricular septal defects. Tex Heart Inst J. 2009; 36:74–75. PMID:
19436794.
9. Alva C, Ho SY, Lincoln CR, Rigby ML, Wright A, Anderson RH. The nature of the obstructive muscular bundles in double-chambered right ventricle. J Thorac Cardiovasc Surg. 1999; 117:1180–1189. PMID:
10343270.
10. Wong PC, Sanders SP, Jonas RA, Colan SD, Parness IA, Geva T, Van Praagh R, Spevak PJ. Pulmonary valve-moderator band distance and association with development of double-chambered right ventricle. Am J Cardiol. 1991; 68:1681–1686. PMID:
1746472.
11. Yoshimura N, Matsuhisa H, Otaka S, Kitahara J, Murakami H, Uese K, Ichida F, Misaki T. Surgical management of multiple ventricular septal defects: the role of the felt sandwich technique. J Thorac Cardiovasc Surg. 2009; 137:924–928. PMID:
19327519.
12. Stellin G, Padalino M, Milanesi O, Rubino M, Casarotto D, Van Praagh R, Van Praagh S. Surgical closure of apical ventricular septal defects through a right ventricular apical infundibulotomy. Ann Thorac Surg. 2000; 69:597–601. PMID:
10735705.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download