Abstract
Purpose
This study aimed to assess hand hygiene (HH) compliance among visitors at a long-term care hospital in South Korea.
Methods
The study was conducted at a 502-bed long-term care hospital located in Gyeonggi-do Province. From July 1 to August 15, 2017, including more than 6 weekends and one holiday, a trained observer covertly assessed visitors' HH at all five units (360 beds in total) of the study hospital building until the completion of 1,000 HH opportunities (i.e., 200 opportunities per unit). The modified World Health Organization (WHO) HH observation form was used. Instead of professional categories and the “before clean/aseptic procedure” moment, the estimated age range for each visitor were recorded in four categories: children (<14 years old), adolescents (14~18), adults (19~64), and the elderly (≥65). The collected data were analyzed using SPSS 22.0.
Results
A total of 1,000 HH opportunities were observed from 766 visitors (an average of 1.31 per visitor) and the overall HH compliance rate was 20.3%. Overall, 53.7% of the HH cases were performed with soap and water. Among the 4 HH moments, the “after body fluid exposure risk” moment showed the highest compliance rate (83.5%); 93.9% used soap and water. The most commonly exposed potential body fluid among visitors was saliva (48.1%).
Since healthcare personnel's hands can be the common mediator for microbial propagation in hospital environments, hand hygiene has been the best strategy to reduce the human-to-human transmission of microorganisms [1]. Hand hygiene is the most effective prevention method that protects both patients and visitors from healthcare-associated infections in hospital settings [2]. Because the hand hygiene compliance rate is the most basic and indispensable indicator for infection control [3], most Korean hospitals have conducted hand hygiene monitoring activities for their healthcare personnel [4]. According to the World Health Organization (WHO), hand hygiene compliance rates among healthcare personnel have been reported at around 30~80% in general since 2007 [3]. The hand hygiene compliance rate of healthcare personnel in Korea has been reported to be 32~95% [567]. A variety of interventions to improve hand hygiene compliance have been made around the world, including providing hand hygiene training to healthcare personnel to improve hand hygiene performance, improving the accessibility of alcohol-based gel hand sanitizers in hospitals, and developing hand hygiene monitoring and feedback programs [89]. Some studies also reported that the improvement in hand hygiene performance as a result of these interventions significantly reduced the incidence of healthcare-associated infections [101112].
Theoretically, not only healthcare personnel but also hospital visitors can be seen as sources of infectious agents [13], but the impact of hospital visitors on infection transmission has not been yet clearly assessed. Regarding the Middle East Respiratory Syndrome (MERS) epidemic that occurred in 2015, the Korea-WHO MERS Joint Assessment Team evaluated that visitors' unlimited access to hospital wards facilitated the rapid spread of MERS. In fact, among domestic MERS confirmed cases, 34.9%(N=65) were family members or visitors [14]. This indicates that the visitors' role in transmission of healthcare-associated infections in Korea is not negligible. However, since most infection control guidelines in healthcare settings are only for healthcare personnel or employees, the need for standardized infection control guidelines targeting visitors has been raised recently in various studies [151617]. Although hand hygiene practices by visitors must be performed both before and after touching a patient [15], several studies abroad have reported that the hand hygiene performance of hospital visitors was significantly lower than that of healthcare personnel. According to an observational study that examined hand hygiene compliance among 3,000 total visitors in terms of the use of alcohol-based hand sanitizer at the hospital lobby of a U.S. hospital with 749 beds, the hand hygiene compliance rate of visitors was 0.52% before the intervention [18]. After the intervention of installing an alcohol-based hand sanitizer stand and an information display, the rate rose to 11.67%. These rates were substantially lower when considering that the study evaluated hand hygiene compliance only in a hospital lobby. Similarly, a previous study examined hand hygiene compliance among a total of 6,603 visitors after a different arrangement of alcohol-based hand sanitizer stands in the lobby of a US tertiary hospital with 560 beds, and it reported that the hand hygiene compliance rate was as low as 3.71% on average [19]. In a study conducted in the U.K., the direct, 24-hour observation of two internal medicine wards showed that the hand hygiene compliance of visitors was 57% [20]. According to a systematic literature review about the studies of hand hygiene compliance that covered publications up to May 2016, the hand hygiene compliance rates of visitors were 0.5~11% at the hospital entrance, 9~35% in the general ward and surgical ward, 11% in the isolation room, 39% in the pediatric ward, 3.95~49.1% at the patient's bedside, and 7~94% in the intensive care unit [21]. Nevertheless, considering the environments of Korean healthcare settings where visitors frequently spent time in patient rooms, infection control activities targeting visitors are very important, but research on the hand hygiene of visitors is insufficient in Korea due to a lack of resources and a shortage of healthcare personnel.
In Korea, the number of long-term care hospitals increased from 202 in 2005, to 900 in 2011, and to 1,428 in 2016, due to an increase in geriatric diseases as Korea has become an aged society [22]. Elderly patients admitted to a long-term care hospital are likely to be exposed to infectious diseases or opportunistic infections due to their longer stay of hospitalization, and their highly frequent social contacts that increase cross-infection risks, such as routine face-to-face contact with caregivers or other patients, have been reported to increase healthcare-related infections in long-term care hospitals [23]. Therefore, this study aimed to investigate the hand hygiene performance among visitors of a long-term care hospital, and to compare the hand hygiene compliance rate by age, gender, and behavior type in order to provide basic data which can contribute to the development of infection control guidelines and hand hygiene education programs for visitors to long-term care hospitals.
This study is a cross-sectional, descriptive research to directly observe and evaluate the hand hygiene compliance rate of visitors to a long-term care hospital by covert observation.
This study was carried out at a long-term care hospital with 502 beds in Gyeonggi-do province, and it was conducted among visitors to five wards (360 beds total) located in the main building where elderly patients who need long-term care usually stay, excluding three wards in the new building where mainly cancer patients are hospitalized. The long-term care hospital where this study was conducted has continuously maintained its status as a first-grade hospital from a long-term care hospital accreditation evaluation by the Korea Institute for Healthcare Accreditation of the Ministry of Health and Welfare since 2013. The hospital also had received a first-grade evaluation for appropriateness as a long-term care hospital from the Health Insurance Review & Assessment Service at the time of this study. When this study was conducted, the long-term care hospital was equipped with infection control guidelines, which included recommendations for healthcare personnel, patients, and visitors, made by the hospital's infection control committee. With regard to the hand hygiene of hospital visitors, the guidelines stated that healthcare personnel should encourage visitor hand hygiene compliance and educate visitors about hand hygiene. Although there was no specific hand hygiene manual for visitors, instruction flyers on the importance of and techniques for hand hygiene compliance for visitors were attached to the entrance of the hospital and on the bulletin boards next to elevator doors on each floor. Alcohol-based gel hand sanitizers were located at the entrance of the hospital, next to each elevator, in nurses' rooms, and at the entrance of each patient room. Considering that many elderly patients with dementia were hospitalized, there was no hand sanitizer in patient rooms for the safety of patients. In all the wards of the main building, private caregivers, instead of family members, were resident at the bedside of patients. The subjects were selected as those who came to the hospital for the purpose of a visit during the observation period and who were in direct contact with the patient or in contact with the patient's surrounding environment. The private caregivers and healthcare personnel were excluded from observation.
The hand hygiene promotion strategy using the WHO Hand Hygiene Observation Form has been successful in various countries and different environments at diverse healthcare institutions around the world, and it is a valid method of investigating the hand hygiene compliance rate, as demonstrated by similar experimental studies involving 43 hospitals in five countries over two years [24]. In this study, we used a modified version of the WHO Hand Hygiene Observation Form (the revised version in 2009) [3] to reflect the characteristics of hospital visitors. The content recorded by the WHO Hand Hygiene Observation Form includes the location (facility, ward, and department), observation time (date, start and end time, period number, and session number), the observer's initials, the subject's profession, hand hygiene action categories (“hand hygiene action by handrubbing with an alcohol-based formula,” “hand hygiene action by handwashing with soap and water,” “no hand hygiene action performed,” and “gloves”), and the indication categories (“before touching a patient,” “before clean/aseptic procedure,” “after body fluid exposure risk,” “after touching a patient,” and “after touching patient surroundings”).
The “profession” category of healthcare personnel included in the WHO Hand Hygiene Observation Form was not applicable for this study's subjects. Thus, instead of recording professions, we recorded the gender and age of the subjects, which were shown to have a significant relationship with hand hygiene compliance in previous studies [1925]. However, since it was not possible to inquire about the subjects' demographic information due to the nature of covert observation, the estimated gender and age of the subject were recorded instead. The estimated age ranges for each visitor were recorded in four groups: children (under 14 years), adolescents (14~18 years), adults (19~64 years), and the elderly (over 65 years). In addition, the types of indications observed were modified to include four types of moments for hand hygiene only, by excluding “before clean/aseptic procedure” moment, as this is irrelevant to visitors. With regard to hand hygiene indications for visitor subjects, the observation form was supplemented by creating the memorandum column for the observer's notes to briefly record more information about the situations related to moments for hand hygiene and the types of body fluids to which the subject was exposed, in order to analyze the observation results better. In particular, when the subject was exposed to two or more types of body fluids, the various types of body fluids were all recorded.
The pilot study with preliminary observation of 30 visitors was conducted on June 17, 2017 and the results showed that the number of moments for hand hygiene observed from a single visitor during a single observation period was not more than two, and the maximum number of moments observed was four. Based on the results, the study observation form was modified to record a maximum of five visitors in one page and a maximum of four moments for hand hygiene per subject.
Data collection was conducted from July 1 to August 15, 2017, on Saturday (6 times), Sunday (6 times), and a public holiday corresponding to a weekday (1 time) by one observer who had previous hand hygiene monitoring experience. Under realistic circumstances, since it was not possible to perform observation for 24 hours a day, including weekdays and public holidays, most of the observations were made between 11:00 am and 1:30 pm, around the lunch hour when there are usually the most visitors, reflecting the fact that most visitors were present around lunch or dinner in the study hospital during the pilot study. Some observations were conducted between 4:00 pm and 6:30 pm around dinner time.
Following the WHO recommendations for prior planning on hand hygiene observation location and time [3] and the guidelines of the Korean Centers for Disease Control and Prevention (KCDC) [2], the observation of hand hygiene compliance was performed for 30 minutes per each ward per session by turns (including ward observation time of 20~30 minutes and the observer's travel time to the next ward). Since it is recommended by the KCDC and WHO that at least 200 observations of moments for hand hygiene should be performed for each observed unit (department) to obtain meaningful results [23], we set the goal of observing 200 moments for hand hygiene per ward (5 wards, a total of 1,000 observation cases). To ensure the accuracy of observation, the maximum number of visitors observed by the observer at one time was limited to 3 [3]. In order to minimize the distortion of the results of hand hygiene compliance due to long visits or frequent visits of specific visitors, the observer tried to exclude the same visitors for the next period in her best, based on the observer's memory. To perform covert observation successfully, the observer wore everyday clothing as other visitors.
The collected data were analyzed with descriptive statistics using SPSS 22.0 (Chicago, IL, USA). The hand hygiene compliance rate was calculated by dividing the number of times hand hygiene was actually performed at the moments for hand hygiene by the total number of the moments for hand hygiene, and then multiplying the result by 100. The numbers of observation cases by estimated age group, gender of visitors, and type of indications were analyzed by calculating the frequency and percentage through frequency analysis. The differences in hand hygiene compliance according to age group, gender, and type of indications were analyzed using the χ2 test. The differences in the hand hygiene methods by visitor gender were also analyzed using the χ2 test. When the expected frequency was 5 or less, Fisher's exact test was performed to compare the differences in hand hygiene methods by the age group and type of indications. All statistical significance levels for statistical tests were set at p<.050.
Since the hospital where hand hygiene observation was conducted did not have an institutional review board (IRB), this study was conducted with the permission of the hospital president, after obtaining the IRB approval (IRB No. 1706/003-005) from the researchers' university. Since it was not possible to provide the explanations about the study to the subjects and get their consent due to the nature of covert observation, the IRB approved the waiver of informed consent of the subjects. Instead, while the observation of hand hygiene compliance was performed, a notice with information about the study period, purpose of observation, and contact information of the researcher was attached to the entrance of the hospital. The notice indicated for the opt-out option that visitors who did not want to be observed during the study of hand hygiene monitoring were requested to notify healthcare personnel or the researcher; no visitors showed their intention for the opt-out during the data collection period. To protect subjects' privacy and confidentiality, we did not record any personally identifiable information except for the estimated age group and gender.
The targeted 1,000 observations of moments for hand hygiene were accomplished from a total of 766 visitors. The average number of hand hygiene moments per visitor was 1.31. The average hand hygiene compliance rate was 20.3%(i.e., 203 cases among a total of 1,000 observations).
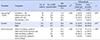
The general characteristics of 766 visitors observed were summarized in Table 1. Regarding gender, males were more predominant (56.8%) than females (43.2%). In terms of the estimated age group, most of the visitors were adults (76.2%), then, adolescents (10.2%), elderly (9.7%), and children (3.9%) in order. The adults group showed the highest hand hygiene compliance rate of 23.4% among all the age groups, as they accounted for the most observed (N=730). The groups of children and elderly showed significantly lower hand hygiene compliance rates of 9.4% and 8.2%, respectively. Gender differences in hand hygiene compliance were not observed.
Among the 203 cases of hand hygiene compliance, hand hygiene was performed using soap and water in 109 cases (53.7%), and alcohol-based gel was used in 84 cases (46.3%). Of note, 78.9% of compliant adolescents (N=15) used alcohol-based gel for their hand hygiene more frequently than soap and water. Regarding the type of hand hygiene indication, the hand hygiene method using alcohol-based gel was used more frequently than soap and water only in the cases of “before touching a patient” which was the most frequently observed (N=620).
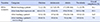
Although the most frequently observed indications were “before touching a patient” (16.1%) and “after touching a patient” (14.0%), the hand hygiene compliance rates for these two types of behaviors were significantly low at 16.1% and 14.0%, respectively. In particular, in the case of “after touching the patient's surroundings,” the hand hygiene compliance rate was the lowest at “7.5%,” and was extremely low at 0% (N=14) in all the age groups, except the adult group which showed a hand hygiene compliance rate of 9.1% (Table 2). In the case of the group of children, the number of observed cases of moments for hand hygiene per child was 1.77, which was higher than the average of 1.31 cases per visitor. In the total number of observations, the cases of “after touching a patient” accounted for 37.7% (20/53), which was higher compared to 18.4% (134/730) in the adult group and 22.7% (22/97) in the elderly group. In the group of children, 4 out of 5 cases of hand hygiene compliance were performed following their parents' behaviors or with their parents' assistance.
In the case of “after body fluid exposure risk,” the hand hygiene compliance rate was the highest at 83.5%, and most of the subjects (93.9%) performed hand hygiene with soap and water (Table 1). The total 79 cases related to “after body fluid exposure risk” were more likely to be potential exposures to body fluids while visitors assisted patient daily care, for instance, when touching an inserted bile bag during changing clothes. Of these, 4 cases exposed to two types of fluids at the same time (Table 3). The most commonly exposed potential body fluid was saliva (48.1 %), followed by excretions (17.7%), secretions (17.7%), sputum (11.4%), and blood (10.1%) in order; there is a possibility of exposure to the blood of patients through touching the insertion site of a venous catheter.
This study investigated the hand hygiene compliance rate of visitors of a long-term care hospital by the covert observation method and reported a 20.3% compliance rate, which is significantly lower than 32~95% among healthcare personnel reported in other studies [56]. Our hand hygiene compliance rate of hospital visitors was similar to the compliance rates (0.52~36.3%) reported in most studies on visitors' hand hygiene compliance from other countries [192627]. Considering the domestic hospital environments and the Korean cultural aspects of visiting a sick friend or relative in the hospital characterized by frequent visitations, it is necessary to pay attention to the hand hygiene of visitors.
Our study found statistically significant differences in the hand hygiene compliance rate among age groups. In particular, the hand hygiene compliance rate in the age group of children was very low (9.4%). In the long-term care hospital in which this study was conducted, 5.3% of the visitors were children. Although children were not the main age group of the visitors, the average number of hand hygiene opportunities per child was 1.77 and the rate for the “after touching a patient” indication was 37.7%, which is higher than other age groups. In our study observation, since some parents had difficulty controlling the behavior of children, children ran around in the hospital after touching a patient and touched commonly shared items or patients' surroundings, which could cause spread of infections. In addition to children's likelihood of transmitting infection in the hospital environment, since children have immature immunity compared to adults [28], the need for hand hygiene is emphasized more when children visit a hospital. In particular, since children were observed carrying out hand hygiene mostly when following their parents' behavior or with their parents' help, it is necessary to develop a strategy for improving the hand hygiene performance of children in a long-term care hospital by including both children and their parents in the targets of a hand hygiene education program.
In our study, most visitors seemed sensitive to visible contaminations and tended to perform hand hygiene, but they did not routinely perform hand hygiene for hand hygiene moments that had invisible, potential contaminations. The most frequently observed hand hygiene moment among visitors was “before touching a patient”, but compliance was significantly low (16.1%). Conversely, the least observed hand hygiene moment was “after body fluid exposure risk”, but compliance was highest (83.5%). This is consistent with previous studies that reported a high hand hygiene compliance rate after behaviors involving body fluid exposure [320]. Moreover, the hand hygiene compliance rate for “after touching a patient's surroundings” was extremely low (7.5%). In particular, except for the adult group, the other age groups did not perform any hand hygiene for “after touching a patient's surroundings.” This result is similar with another study's finding that hand hygiene performance was the lowest after touching the patient's surroundings [29]. Therefore, it is necessary to develop an educational program to change visitors' awareness on hand hygiene moments by showing that microbial propagation can be possible not only by contamination but also by simple skin contact or contact with the patient's surroundings.
Our study finding that only adolescents used alcohol-based gel more than soap and water is similar to another study's result that the younger-aged group preferred to use alcohol-based gel compared with middle-aged and elderly groups [19]. This difference in the hand hygiene methods may be affected by the fact that alcohol-based gel sanitizers were not placed in patient rooms or near the beds but placed only at the entrance of each ward to prevent any harmful accidents, due to the frequent prevalence of dementia among hospitalized elderly patients in the study hospital. In addition, a single sink location for using soap and water in a shared patient room (i.e., 5~6 patients per a room) might affect visitors' hand hygiene compliance and hand hygiene methods.
Importantly, the results of this study revealed that visitors were also exposed to body fluids such as saliva, urine, feces, and sputum. Most family visitors had skin contacts with the patient, such as greeting, arm or leg massage, or moving support. Moreover, they were likely exposed to the patient's body fluids through contact with an inserted device (e. g., urine bag) while assisting patient care in ways that are commonly expected from the traditional Confucian ideals of caring for elderly parents. In some rare cases, some visitors were exposed to the blood of the patient through the contact with the insertion site of the central venous catheter or peripheral venous catheter of the patient. Fortunately, it was found that the hand hygiene compliance rate was much higher (83.5%) “after body fluid exposure risk,” and that most visitors performed hand hygiene with soap and water in such cases (93.9%). However, since it was shown that there is a sufficient possibility that visitors of long-term care hospital will be exposed to body fluids, it is necessary to implement active educational interventions to increase the hand hygiene performance among visitors.
This study has the following limitations. First, our study's compliance results among visitors are not generalizable, because hand hygiene observations were conducted for limited weekend meal-time periods when most visitors were present in the studied long-term care hospital. Second, although the direct observation method with the advantage of examining details such as the degree and duration of hand hygiene during observation [1] was applied, one observer had to observe a maximum of 3 visitors perform hand hygiene compliance at the same time around meal hours when there were a number of visitors. Thus, our study could not measure the duration of hand hygiene and the adequacy of the hand hygiene performance by visitors. In order to supplement this limitation, the two observers-method could be adopted for monitoring the hand hygiene performance at the same time, but inter-observer reliability between two observers needs to be secured. Moreover, in a rather uncrowded place like a long-term care hospital, some difficulties are expected to conceal the presence of two observers naturally and conduct covert observation. Third, there may be the limitation of excluding overlapped people from the observation of the next sessions based on the memory of the sole observer. Fourth, because the study was conducted by the covert observation method which makes it possible to accurately examine the actual performance of the subject because the subject does not know that his or her hand hygiene performance is being observed, factors which may influence hand hygiene performance such as the age, the education level, and the experience of hand hygiene education could not be examined and included in the analysis. Fifth, since the subject's age could not be accurately confirmed by the limitation of covert observation, the estimated age groups of visitors were divided only into children, adolescents, adults, and elderly, and could not be divided in a more specific manner. Sixth, since our study observation were conducted only during the specific time periods of weekends and the single holiday, our study could not monitor all of the hand hygiene compliance during 24 hours.
Despite the above limitations, this study is the first research attempt to examine the hand hygiene compliance rate among the visitors of long-term care hospitals in Korea, and provides meaningful basic data on the hand hygiene compliance rate of hospital visitors. In fact, to improve hand hygiene performance, multi-modal interventions are necessary because hand hygiene compliance is affected by various factors, such as the system change of healthcare institutions, policies, and social norms, as well as education and training [30]. Therefore, our study results are expected to contribute to the improvement of the hand hygiene compliance of visitors by being adopted for the development of the guidelines for infection control and the hand hygiene education program for hospital visitors.
This study was conducted to investigate the hand hygiene compliance rate among visitors of long-term care hospitals. A total of 1,000 cases of moments for hand hygiene were observed from 766 visitors, and the overall hand hygiene compliance rate of the visitors of a long-term care hospital was 20.3%. Therefore, hand hygiene education programs and infection control guidelines for hospital visitors in long-term care hospitals need to be developed and implemented.
Based on our study results, the following future studies are recommended. First of all, more studies on hand hygiene compliance among visitors are necessary at a number of different long-term care hospitals with various numbers of visitors. Moreover, not only limited to long-term care hospitals, more expanded research on visitors' hand hygiene compliance need to be conducted across healthcare settings, such as tertiary hospitals and general hospitals. Further studies on visitors' knowledge, attitude, and factors related hand hygiene performance would be essential to understand visitors' hand hygiene performance better. In addition, it would be meaningful to conduct a covert observation study to investigate the overall performance of the infection control guidelines for visitors, such as standard precautions and mask-wearing, not only for hand hygiene, at long-term care hospitals. Given the lack of standardized hospital visitors' infection control guidelines, we need more evidence to understand visitors' characteristics by age group, gender, and behaviors or interactions at each hospital setting. Based on our study results showing the differences in the hand hygiene compliance rate and the frequency of the use of hand hygiene methods among visitors, customized, effective educational programs for hospital visitors need to be established reflecting patient characteristics, hospital environments, and visitors' needs for education on infection control.
Figures and Tables
Table 1
Summary of Results of Hand Hygiene Practices among Visitors in a Long-term Care Hospital (Total Number of Hand Hygiene Opportunities=1,000)
Notes
References
1. World Health Organization. Hand hygiene technical reference manual [Internet]. Geneva: World Health Organization;2009. cited 2018 February 26. Available from: "http://whqlibdoc.who.int/publications/2009/9789241598606_eng.pdf.
2. Korea Centers for Disease Control and Prevention. Guideline for hand hygiene in healthcare facilities. Osong: Korea Centers for Disease Control and Prevention;2014. p. 58.
3. World Health Organization. WHO guidelines on hand hygiene in health care: First global patient safety challenge clean care is safer care [Internet]. Geneva: World Health Organization;2009. cited 2018 February 26. Available from: https://apps.who.int/iris/bitstream/handle/10665/44102/9789241597906_eng.pdf?sequence=1.
4. Jeong SY, Kim OS, Lee JY. The status of healthcare-associated infection control among healthcare facilities in Korea. Journal of Digital Convergence. 2014; 12(5):353–366. DOI: 10.14400/jdc.2014.12.5.353.

5. Song JY, Jeong IS. The hawthorne effect on the adherence to hand hygiene. Perspectives in Nursing Science. 2015; 12(1):7–13. DOI: 10.16952/pns.2015.12.1.7.

6. Oh HS. Analysis of hand hygiene practices of health care personnels. Journal of the Korea Academia-Industrial cooperation Society. 2015; 16(9):6160–6168. DOI: 10.5762/KAIS.2015.16.9.6160.

7. Oh HS. Hand hygiene compliance of healthcare workers in a children's hospital. Pediatric Infecion and Vaccine. 2015; 22(3):186–193. DOI: 10.14776/piv.2015.22.3.186.

8. Kingston L, O'Connell NH, Dunne CP. Hand hygiene-related clinical trials reported since 2010: A systematic review. Journal of Hospital Infection. 2016; 92(4):309–320. DOI: 10.1016/j.jhin.2015.11.012.

9. Neo JR, Sagha-Zadeh R, Vielemeyer O, Franklin E. Evidence-based practices to increase hand hygiene compliance in health care facilities: An integrated review. American Journal of Infection Control. 2016; 44(6):691–704. DOI: 10.1016/j.ajic.2015.11.034.


10. MacDonald A, Dinah F, MacKenzie D, Wilson A. Performance feedback of hand hygiene, using alcohol gel as the skin decontaminant, reduces the number of inpatients newly affected by MRSA and antibiotic costs. Journal of Hospital Infection. 2004; 56(1):56–63. DOI: 10.1016/s0195-6701(03)00293-7.

11. Monistrol O, Calbo E, Riera M, Nicolas C, Font R, Freixas N, et al. Impact of a hand hygiene educational programme on hospital-acquired infections in medical wards. Clinical Microbiology and Infection. 2012; 18(12):1212–1218. DOI: 10.1111/j.1469-0691.2011.03735.x.


12. Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet. 2000; 356(9238):1307–1312. DOI: 10.1016/s0140-6736(00)02814-2.


13. Siegel JD, Rhinehart E, Jackson M, Chiarello L. Healthcare Infection Control Practices Advisory Committee. 2007 Guideline for isolation precautions: Preventing transmission of infectious agents in healthcare settings. American Journal of Infection Control. 2007; 35(10):S65–S164. DOI: 10.1016/j.ajic.2007.10.007.
14. Korean Medical Association. Middle East Respiratory Syndrome. Seoul: Korean Medical Association;2016. p. 260.
15. Banach DB, Bearman GM, Morgan DJ, Munoz-Price LS. Infection control precautions for visitors to healthcare facilities. Expert Review of Anti-infective Therapy. 2015; 13(9):1047–1050. DOI: 10.1586/14787210.2015.1068119.


16. Kang J, Weber DJ, Mark BA, Rutala WA. Survey of North Carolina hospital policies regarding visitor use of personal protective equipment for entering the rooms of patients under isolation precautions. Infection Control and Hospital Epidemiology. 2014; 35(3):259–264. DOI: 10.1086/675293.

17. Munoz-Price LS, Banach DB, Bearman G, Gould JM, Leekha S, Morgan DJ, et al. Isolation precautions for visitors. Infection Control and Hospital Epidemiology. 2015; 36(7):747–758. DOI: 10.1017/ice.2015.67.


18. Birnbach DJ, Nevo I, Barnes S, Fitzpatrick M, Rosen LF, Everett-Thomas R, et al. Do hospital visitors wash their hands? Assessing the use of alcohol-based hand sanitizer in a hospital lobby. American Journal of Infection Control. 2012; 40(4):340–343. DOI: 10.1016/j.ajic.2011.05.006.


19. Hobbs MA, Robinson S, Neyens DM, Steed C. Visitor characteristics and alcohol-based hand sanitizer dispenser locations at the hospital entrance: Effect on visitor use rates. American Journal of Infection Control. 2016; 44(3):258–262. DOI: 10.1016/j.ajic.2015.10.041.


20. Randle J, Arthur A, Vaughan N. Twenty-four-hour observational study of hospital hand hygiene compliance. Journal of Hospital Infection. 2010; 76(3):252–255. DOI: 10.1016/j.jhin.2010.06.027.

21. Compton D, Davenport TE. Compliance with hand-washing guidelines among visitors from the community to acute care settings. Journal of Acute Care Physical Therapy. 2018; 9(1):19–34. DOI: 10.1097/jat.0000000000000070.
22. Health Insurance Review and Assessment Service, National Health Insurance Service. 2016 National health insurance statistical yearbook [Internet]. Seoul: Health Insurance Review and Assessment Service & National Health Insurance Service;2017. cited 2018 February 26. Available from: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020045020000&brdScnBltNo=4&brdBltNo=2309&pageIndex=1#none.
23. World Health Organization. Hand hygiene in outpatient and home-based care and long-term care facilities [Internet]. Geneva: World Health Organization;2012. cited 2018 February 26. Available from: https://apps.who.int/iris/bitstream/handle/10665/78060/9789241503372_eng.pdf?sequence=1.
24. Allegranzi B, Gayet-Ageron A, Damani N, Bengaly L, McLaws M-L, Moro M-L, et al. Global implementation of WHO's multimodal strategy for improvement of hand hygiene: A quasi-experimental study. The Lancet Infectious Diseases. 2013; 13(10):843–851. DOI: 10.1016/s1473-3099(13)70163-4.


25. Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: Performance, beliefs, and perceptions. Annals of Internal Medicine. 2004; 141(1):1–8. DOI: 10.7326/0003-4819-141-1-200407060-00008.


26. Birnbach DJ, Nevo I, Barnes S, Fitzpatrick M, Rosen LF, Everett-Thomas R, et al. Do hospital visitors wash their hands? Assessing the use of alcohol-based hand sanitizer in a hospital lobby. American Journal of Infection Control. 2012; 40(4):340–343. DOI: 10.1016/j.ajic.2011.05.006.


27. Willison-Parry TA, Haidar EA, Martini LG, Coates AR. Handwashing adherence by visitors is poor: Is there a simple solution? American Journal of Infection Control. 2013; 41(10):928–929. DOI: 10.1016/j.ajic.2013.01.023.


28. Pessoa-Silva CL, Hugonnet S, Pfister R, Touveneau S, Dharan S, Posfay-Barbe K, et al. Reduction of health care associated infection risk in neonates by successful hand hygiene promotion. Pediatrics. 2007; 120(2):e382–e390. DOI: 10.1542/peds.2006-3712.

29. FitzGerald G, Moore G, Wilson AP. Hand hygiene after touching a patient's surroundings: The opportunities most commonly missed. Journal of Hospital Infection. 2013; 84(1):27–31. DOI: 10.1016/j.jhin.2013.01.008.

30. Kingston L, O'Connell NH, Dunne CP. Hand hygiene-related clinical trials reported since 2010: a systematic review. Journal of Hospital Infection. 2016; 92(4):309–320. DOI: 10.1016/j.jhin.2015.11.012.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download