This article has been
cited by other articles in ScienceCentral.
Abstract
Background
The reports about fertility desire and pregnancy outcome among women infected with human immunodeficiency virus (HIV) in Korea are scarce. This study aimed to determine the changing trend in pregnancy incidence among women infected with HIV in Korea.
Materials and Methods
We retrospectively reviewed the medical records of women infected with HIV visiting Pusan National University Hospital between January 1990 and October 2018.
Results
A total of 149 women with HIV infection visited the study hospital. Among them, 33 pregnancies in 24 (16.1%) women were identified. There were 17 live births (51.5%) and 13 abortions (39.4%), whereas 3 women (9.1%) were transferred to another hospital or were lost to follow-up. The number of live birth rose from 0 in 1990-1998 to 17 in 1999-2018. The proportion of repeated pregnancies after HIV diagnosis also increased steeply, from 14.3% in 1999-2008 to 50% in 2009-2018. However, the number of abortions also increased over time. There were 8 induced abortions, 7 (87.5%) of them were diagnosed with HIV infection during pregnancy and 3 (37.5%) were unplanned pregnancies. Eighteen babies, including 1 twin case, were born from 17 births. There was no mother-to-child HIV transmission in our study.
Conclusion
The number of pregnancies among women with HIV infection and repeated pregnancies after HIV diagnosis has been increasing in Korea, probably due to the desire of HIV patients to have more children. However, the number of abortions also increased, probably due to health concerns and uncertain pregnancy outcome.
Keywords: Human immunodeficiency virus, Live birth, Mother-to-child transmission, Pregnancy
Introduction
Almost half of the people living with human immunodeficiency virus (PLWH) globally are women and many of these are of childbearing age [
1]. Fertility issues for human immunodeficiency virus (HIV)-infected women are becoming increasingly important, but pregnancy decision-making is complicated for women with HIV infection. In the absence of any intervention, the rate of mother-to-child transmission (MTCT) of HIV ranges from 15% to 45%. Antiretroviral therapy (ART) and other effective preventive interventions can reduce this risk to below 2% [
2]. As ART has increased the life expectancy of PLWH, women with HIV infection are now more frequently considering becoming pregnant [
34]. Additionally, a growing number of women with HIV infection have second and even third pregnancies after HIV diagnosis [
5]. Nevertheless, many women with HIV infection still avoid pregnancy because of continuing concerns regarding their own personal health and their baby's health [
6]. Despite the importance of planning pregnancies when dealing with HIV infection, many pregnancies remain unplanned. Deliberate termination is often the outcome of unintended pregnancies [
78].
In Korea, approximately 10% of PLWH are women. By the end of 2017, the reported cumulative number of women with HIV infection in Korea was 1501, including 473 (31.5%) of racial and ethnic minorities. Approximately 60% of women with HIV infection are of reproductive age (15-44 years old) at the time of HIV diagnosis [
910]. Fertility issues for women with HIV infection are becoming increasingly important. Although there has been one recent report [
11], the data about the pregnancy rate and outcome among women with HIV infection in Korea are scarce. The aim of this study was to examine the trends in pregnancy and pregnancy outcome over the past 28 years in women with HIV infection at a tertiary care hospital in Korea.
Materials and Methods
We retrospectively reviewed the medical records of women infected with HIV visiting Pusan National University Hospital between January 1990 and October 2018. The hospital is a 1,450-bed university-affiliated teaching hospital and provides HIV care for PLWH in the southeastern region of Korea. The collected data included patient demographics, HIV diagnosis date, CD4 cell count, HIV RNA viral load, presence of coinfection, ART use and timing, delivery and obstetrical history, history of preventive chemotherapy, neonatal ART, follow-up, and transmission outcomes. Pediatric HIV monitoring was performed with the HIV-1 plasma viral load test [Amplicor HIV-1 Monitor HIV-1 test, (Roche Molecular Systems, Branchburg, NJ, USA) or Cobas AmpliPrep/Cobas TaqMan HIV-1 test (Roche Molecular Systems)] and HIV antibody test [ASYM HIV 1/2gO® MEIA assay (Abbott Laboratories, Abbott Park, IL, USA), ARCHITECT® HIV Ag/Ab Combo assay (Abbott Laboratories, Wiesbaden, Germany), or Elecsys® HIV combi PT assay (Roche Molecular Systems, Branchburg, N.J)]. HIV RNA PCR tests were performed within 24 hours, 1-2 months, or 4-6 months after birth and the HIV antibody test was performed 18 months after birth. HIV genotypic resistance was determined with the ViroSeq HIV-1 Genotyping System (ViroSeqTM, HIV-1 Genotyping system v2.0, v3.0 Celera Corporation, Foster City, CA, USA). All statistical analyses were performed using IBM SPSS version 20 (IBM Co., Armonk, NY, USA). The study protocol was approved by the institutional review board of Pusan National University Hospital (IRB No H-1712-001-061), which recommended waiver of informed consent.
Results
Between January 1990 and October 2018, a total of 149 women with HIV infection visited the study hospital. Their median age at entry into HIV care was 40 years [interquartile range (IQR) 30-53, range 14-72] and 84 (56.4%) were of reproductive age (15-44 years old). The majority of women were Koreans (89.9%) and 15 (10.1%) belonged to ethnic minorities or were immigrants.
During the study period, there were 33 pregnancies in 24/149 (16.1%) women with HIV infection. Of these, 17 pregnancies (48.5%) ended in live births, 8 (24.2%) in induced abortions, 4 (12.1%) in miscarriages, and 1 (3%) in ectopic pregnancy. In 3 cases (9.1%), pregnancy outcome was unknown because 2 women were transferred to other hospitals and 1 was lost to follow-up. Of the 33 pregnancies, 11 (33.3%) were reported as unplanned. Four of them ended in live births, 6 in terminations (3 induced abortions, 2 miscarriages and 1 ectopic pregnancy) and 1 was lost to follow-up. Of the 8 induced abortions, 7 (87.5%) were diagnosed with HIV during pregnancy and 3 (37.5%) were unplanned pregnancies. There was only 1 case of induced abortion in pregnancies after HIV diagnosis. Partner`s HIV status was identified in 29 pregnancies. Live births were more likely in serodiscordant couples than in seroconcordant couples (
Table 1).
Table 1
Pregnancy events and outcome of 17 live births in 11 women with human immunodeficiency virus infection

|
Characteristics |
No. of observations |
% |
|
Age at conception, median (years) |
29 |
IQR 26–32 |
|
Korean ethnicity (out of 11 women) |
10 |
90.1 |
|
Marital status |
|
|
|
Married at the time of the first birth (out of 11 women) |
7 |
63.6 |
|
Married at the time of repeated birth (out of 5 women) |
5 |
100 |
|
Nullipara before first birth (out of 11 women) |
9 |
81.8 |
|
Fertility intention |
|
|
|
Intended pregnancy in the first birth (out of 11 pregnancies) |
7 |
63.6 |
|
Intended pregnancy in repeated birth (out of 6 pregnancies) |
6 |
100 |
|
Time of HIV diagnosis (out of 11 women) |
|
|
|
Before the first live birth pregnancy |
8 |
72.7 |
|
During the first live birth pregnancy |
3 |
27.3 |
|
Partner's HIV status |
|
|
|
HIV infected partners in the first birth (12 partners for 11 women) |
5 |
41.7 |
|
Serostatus unknown in the first birth (12 partners for 11 women) |
1 |
8.3 |
|
HIV infected partners in the second or third birth (out of 5 partners) |
1 |
20.0 |
|
The median CD4 cell count at third trimester of pregnancies (cells/µL) |
430 |
IQR 199–551 |
|
HBV or HCV seropositivea
|
3 |
27.3 |
|
Timing of combination ART |
|
|
|
Before conception |
9 |
52.9 |
|
During conception |
6 |
35.3 |
|
After delivery |
2 |
11.8 |
|
Drug resistance mutations in HIV-1 genotypic resistance test (out of 7 patients) |
1 |
14.3 |
|
Gestational age at delivery, median (weeks) |
37+4
|
IQR 37+1–38+0
|
|
Mode of delivery |
|
|
|
Scheduled cesarean delivery |
13 |
76.5 |
|
Emergency cesarean deliveryb
|
4 |
23.5 |
|
Pregnancy outcome (out of 18 babies)c
|
|
|
|
Body weight, median (g) |
2,700 |
IQR 2,415–2,985 |
|
Preterm delivery |
4 |
22.2 |
|
Mother-to-child transmission of HIV (RT-PCR negative at 6 months after birth, out of 13 babies)d
|
0 |
0 |

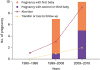
Among 24 women with HIV infection, 14 (58.3%) were diagnosed with HIV during pregnancy and 10 (41.7%) became pregnant after their HIV diagnosis. Seven (29.2%) women had more than one pregnancy. Of these, 5 women gave live birth more than once (2 live births in 4 women, 3 live births and a miscarriage in 1 woman) and 2 gave birth in their second pregnancies after deliberately terminating their first pregnancies. There is an increasing trend in the number of live births over time, with a corresponding change in the number of abortions (
Fig. 1). The number of live births rose from 0 in the pre-ART era (1990-1998) to 17 in the ART era (1999-2018). Although the number of live births has been steadily rising in the ART era, the proportion of repeated live births steeply increased from 14.3% in 1999-2008 to 50% in 2009-2018 (
Fig. 1).
 | Figure 1 Trends in pregnancy and live births among women living with human immunodeficiency virus in Korea by year, 1990–2018.
|
Pregnancy events and outcomes of 17 live births in 11 women with HIV infection are shown in
Table 1. Their median age at conception was 29 years (IQR 26-32, range 17-41). Four women were unmarried at the first birth. Two of them married later, 1 mother sent her baby to a child protection for adoption, and 1 was lost to follow up. The median CD4 cell count at third trimester of pregnancy was 430 cells/µL (IQR 199-551, range 112-760). In 6 (35.3%) pregnancies, ART was initiated during pregnancy; 2 of which were diagnosed with HIV during pregnancy and 4 before conception. The median gestational age at which ART was initiated was 19
+6 weeks (IQR 14
+2-22
+6 weeks, range 10-35 weeks). In 2 (11.8%) pregnancies in which emergency cesarean delivery was performed, ART was started just before the beginning of delivery. In 9 (52.9%) pregnancies, ART had been initiated prior to conception. The proportion of women with undetectable viral load was 47.1% (8 of 17) at entry into obstetric care and 82.4% (14 of 17) at the time of delivery. HIV-1 genotypic resistance was determined in 7 patients and 6 had no primary mutations associated with resistance to nucleoside reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors, and protease inhibitors (PIs). One woman had major mutations conferring drug resistance to NRTIs (M41L, M184V, T215F) and PIs (M46I, I54V, L76V, V82F) during her second pregnancy.
Eighteen babies, including 1 twin case, were born in 17 pregnancies of 11 women with HIV infection. The overall median gestational age at delivery was 37+4 weeks (IQR 37+1-38 weeks, range 32+4-40+1 weeks). Three births (17.6%) occurred before 37 weeks, due to premature rupture of membranes (33+4 weeks) and 2 preterm labor (33+1 and 35+3 weeks). Of the 17 births, scheduled cesarean delivery was performed in 13 (76.5%) and emergency cesarean delivery in 4 (23.5%). Fifteen (88.2%) received zidovudine before cesarean delivery and 2 (11.8%) had oral zidovudine and lamivudine due to unavailability of intravenous zidovudine. Neonatal post-exposure prophylaxis with zidovudine syrup was continued for the recommended 6 weeks in 15 newborns except for 2 taking zidovudine syrup continuously and 1 who was lost to follow-up after 4 weeks of birth. The median weight of 18 newborns was 2,740 g (IQR 2,415-2,985 g, range 1,570-3,700 g). The median Apgar score was 6 (IQR 6-8, range 3-8) and 8 (IQR 8-9, range 6-9) at 1 and 5 minutes after delivery, respectively.
Of the 18 babies born in the study hospital, HIV test by PCR was negative at 6 months after birth in 13 babies and is still pending for 3 babies. Results of HIV RNA performed within 24 hours and 1-2 months after birth were all negative. HIV antibody test at 18 months was negative in 12 babies and is still pending for 4 babies, who are less than 18 months old. One baby, who did not perform the test due to loss to follow-up, was negative for HIV transmission after 4 weeks of birth. One baby was sent to a child protection center for adoption and was confirmed to have no HIV transmission through patient's interview.
Discussion
This descriptive study assessed the changing trend in pregnancy and childbirth over 28 years in women with HIV infection at a tertiary care hospital in Korea. In our study, approximately 16% of women with HIV infection had at least one pregnancy during HIV care in the study hospital. The number of reported pregnancies in women with HIV infection increased substantially in the ART era compared to the pre-ART era. In the ART era, the number of pregnancies has almost doubled in 2009-2018 compared to 1990-2008. These findings are consistent with previous studies examining pregnancy incidence in women with HIV infection, as their life span is extended with ART [
121314].
In ART era, the live birth rate in women with HIV infection is approaching closer to that in women without HIV infection [
15]. Nevertheless, pregnancy decision-making is complicated for women with HIV infection and there are still gaps between intention and practice. Women with HIV infection are concerned about their own health or about infecting their child and the child's future care and many pregnancies are unplanned or unintended [
7816]. Unintended pregnancies often end in abortion. In a study conducted in United States, despite that the live birth rate of HIV-positive women was similar to that of HIV-negative women, age-adjusted abortion rates remained unchanged [
15]. In our study, the number of abortions also increased over time, with the increase of the number of pregnancies. Especially, our results suggest that most induced abortions were performed in women diagnosed with HIV during pregnancy, probably due to concerns about their own health and pregnancy outcome.
In this study, we also found that the proportion of repeated pregnancies after HIV diagnosis increased over time, from 14.3% in 1999-2008 to 50% in 2009-2018. One woman conceived 4 times after HIV diagnosis including 3 live births and 1 miscarriage. Previous studies have reported a recent increase in repeated pregnancies among women with HIV infection [
5171819]. Repeated pregnancies are not just a consequence of lack of or ineffective contraception, but also reflect the desire of these individuals to have multiple children [
517]. In our study, 63.6% (7/11) of first-time pregnancies were intended, while all 6 repeated pregnancies were also intended due to the desire for additional childbearing; partners were HIV negative in 80% of these (
Table 1). Trends and patterns of pregnancy and childbirth may vary between different countries. Our results are consistent with other studies showing that women with HIV infection are increasingly choosing to become pregnant, even to have repeated pregnancies after their HIV diagnosis [
51719].
This study has some limitations. First, this is an observational study, thus we cannot exclude the presence of unmeasured confounding. Second, our study was conducted at a single center in the southeastern region of Korea and the number of women with HIV infection was relatively small; therefore, our findings may not be extrapolated to other regions of the country. Nevertheless, the number of patients included in this study is equivalent to 9.8% of all women with HIV infection in Korea. Third, we do not have reliable data on pregnancy intention or abortion access due to the retrospective design of the study.
In summary, we demonstrated that the number of reported pregnancies in women with HIV infection increased substantially. Accordingly, the proportion of repeated pregnancies after HIV diagnosis increased steeply due to desire for additional childbearing. However, the number of abortions also increased over time. Women with HIV infection chose induced abortion at the time of HIV diagnosis during pregnancy and rarely after HIV diagnosis, probably due to concerns about their own health and pregnancy outcome. These results suggest that trends in pregnancy and childbirth among women with HIV infection are changing, although there are still gaps between intention and practice in Korea. Further research is required to examine all variables affecting reproductive decision-making among women with HIV infection in Korea.
ACKNOWLEDGMENTS
This work was supported by a 2-year Research Grant of Pusan National University.
References
1. Libourel EJ, Sonneveld P, van der Holt B, de Maat MP, Leebeek FW. High incidence of arterial thrombosis in young patients treated for multiple myeloma: results of a prospective cohort study. Blood. 2010; 116:22–26.


2. Centers for Disease Control and Prevention (CDC). Achievements in public health. Reduction in perinatal transmission of HIV infection--United States, 1985-2005. MMWR Morb Mortal Wkly Rep. 2006; 55:592–597.

3. Agangi A, Thorne C, Newell ML. European Collaborative Study. Increasing likelihood of further live births in HIV-infected women in recent years. BJOG. 2005; 112:881–888.


4. Blair JM, Hanson DL, Jones JL, Dworkin MS. Trends in pregnancy rates among women with human immunodeficiency virus. Obstet Gynecol. 2004; 103:663–668.


5. Firth J, Wang CC, Gillani F, Alexander N, Dufort E, Rana A, Cu-Uvin S. The changing face of HIV in pregnancy in Rhode Island 2004-2009. Infect Dis Obstet Gynecol. 2012; 2012:895047.

6. Finocchario-Kessler S, Sweat MD, Dariotis JK, Trent ME, Kerrigan DL, Keller JM, Anderson JR. Understanding high fertility desires and intentions among a sample of urban women living with HIV in the United States. AIDS Behav. 2010; 14:1106–1114.


7. Loutfy M, Raboud J, Wong J, Yudin M, Diong C, Blitz S, Margolese S, Hart T, Ogilvie G, Masinde K, Tharao W, Linklater G, Salam K, Ongoiba F, Angel J, Smaill F, Rachlis A, Ralph E, Walmsley S. Ontario HIV Fertility Research Team. High prevalence of unintended pregnancies in HIV-positive women of reproductive age in Ontario, Canada: a retrospective study. HIV Med. 2012; 13:107–117.


8. Darak S, Hutter I, Kulkarni V, Kulkarni S, Janssen F. High prevalence of unwanted pregnancies and induced abortions among HIV-infected women from Western India: need to emphasize dual method use? AIDS Care. 2016; 28:43–51.


10. Korean Centers for Disease Control and Prevention (KCDC). Annual report on the notified HIV/AIDS in Korea 2017. Accessed 15 October 2018. Available at:
http://www.cdc.go.kr.
11. Choi H, Kim MH, Lee SJ, Kim EJ, Lee W, Jeong W, Jung IY, Ahn JY, Jeong SJ, Ku NS, Baek JH, Choi YH, Kim HY, Kim JM, Choi JY. Pregnancy rates and outcomes of HIV-infected women in Korea. J Korean Med Sci. 2018; 33:e296.

12. Fok WK, Blumenthal PD. HIV and contraception. Curr Opin Obstet Gynecol. 2017; 29:419–426.


13. Sharma A, Feldman JG, Golub ET, Schmidt J, Silver S, Robison E, Minkoff H. Live birth patterns among human immunodeficiency virus-infected women before and after the availability of highly active antiretroviral therapy. Am J Obstet Gynecol. 2007; 196:541.e1–541.e6.

14. Whitmore SK, Zhang X, Taylor AW, Blair JM. Estimated number of infants born to HIV-infected women in the United States and five dependent areas, 2006. J Acquir Immune Defic Syndr. 2011; 57:218–222.


15. Haddad LB, Wall KM, Mehta CC, Golub ET, Rahangdale L, Kempf MC, Karim R, Wright R, Minkoff H, Cohen M, Kassaye S, Cohan D, Ofotokun I, Cohn SE. Trends of and factors associated with live-birth and abortion rates among HIV-positive and HIV-negative women. Am J Obstet Gynecol. 2017; 216:71.e1–71.16.

16. de Bruyn M. Safe abortion for HIV-positive women with unwanted pregnancy: a reproductive right. Reprod Health Matters. 2003; 11:152–161.


17. Floridia M, Tamburrini E, Masuelli G, Martinelli P, Spinillo A, Liuzzi G, Vimercati A, Alberico S, Maccabruni A, Pinnetti C, Frisina V, Dalzero S, Ravizza M. Italian Group for Surveillance of Antiretroviral Treatment in Pregnancy. Rate, correlates and outcomes of repeat pregnancy in HIV-infected women. HIV Med. 2017; 18:440–443.


18. Bryant AS, Leighty RM, Shen X, Read JS, Brouwers P, Turpin DB, LaRussa PS, Pacheco-Acosta E, Paul ME, Vajaranant M, Tuomala RE. Women and Infants Transmission Study. Predictors of repeat pregnancy among HIV-1-infected women. J Acquir Immune Defic Syndr. 2007; 44:87–92.







 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download