Abstract
Purpose
This study aims to investigate the actual compliance with chemotherapy and analyze several factors affecting the compliance in patients with gastric cancer.
Methods
From February 2012 to December 2014, we collected data of patients with gastric cancer who received adjuvant chemotherapy (TS-1 monotherapy or XELOX: capecitabine/oxaliplatin) in Korea.
Results
We collected data of 1,089 patients from 31 institutions. The completion rate and dose reduction rate by age (≥60 years vs. <60 years) were 57.5% vs. 76.8% (P < 0.001) and 17.9% vs. 21.3% (P = 0.354); by body mass index (BMI) (≥23 kg/m2 vs. <23 kg/m2) were 70.2% vs. 63.2% (P = 0.019) and 19.2% vs. 19.9% (P = 0.987), respectively. The compliance by American Society of Anesthesiologists physical status (ASA PS) classification was as follows: completion rate was 74.4%, 62.8%, and 60% (P = 0.001) and the dose reduction rate was 18.4%, 20.7%, and 17.8% (P = 0.946) in ASA PS classification I, II, and III, respectively. The completion rate of TS-1 and XELOX was 65.9% vs. 70.3% (P = 0.206) and the dose reduction rate was 15.7% vs. 33.6% (P < 0.001). Furthermore, the completion rate of chemotherapy by surgical oncologists and medical oncologists was 69.5% vs. 63.2% (P = 0.028) and the dose reduction rate was 17.4% vs. 22.3% (P = 0.035), respectively.
Two large prospective randomized trials, Adjuvant Chemotherapy Trial of TS-1 (ACTS-GC) and Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC) trials, proved the survival benefit of adjuvant chemotherapy for advanced gastric cancer (AGC) [123]. Since these trials, most patients in the world, including Korea and Japan, who underwent radical D2 gastrectomy for AGC and histologically confirmed stages II and III were treated with TS-1 monotherapy or capecitabine and oxaliplatin after surgery.
In adjuvant chemotherapy for AGC, the compliance with chemotherapy is a critical issue because it could affect the survival with the TNM stage. Kim et al. [4] reported that a decreased relative dose intensity of TS-1 monotherapy led to a poor survival rate. Several studies, including those on colon and breast cancer, have advocated the significance of the compliance with adjuvant chemotherapy for the survival benefit [56]. However, few studies have investigated the compliance with adjuvant chemotherapy in gastric cancer. Since the commencement of health care insurance of adjuvant chemotherapy for AGC in 2013, no data have been collected on its compliance in Korea.
Our study group, named the Surgical Oncology Forum (SOF), conducted a nationwide survey on adjuvant chemotherapy for AGC. This study aims to investigate the actual compliance with adjuvant chemotherapy and analyze various factors affecting the compliance in patients with gastric cancer.
From February 2012 to December 2014, we collected data of patients with gastric cancer who received adjuvant chemotherapy (TS-1 monotherapy or XELOX: capecitabine/oxaliplatin) at 31 institutions in Korea. The inclusion criteria were as follows: patients with gastroesophageal junction or gastric adenocarcinoma who underwent curative surgery with D2 lymph node dissection, histologically confirmed stages II–III gastric adenocarcinoma according to the manual of the American Joint Committee on Cancer, 7th edition [7] , and no previous cancer treatments (radiotherapy, immunotherapy, and chemotherapy). We assessed the compliance by the following factors: sex, age, body mass index (BMI), American Society of Anesthesiologists physical status (ASA PS) classification, extent of resection, regimen, number of cycles, and subject of chemotherapy (i.e., surgical oncologists who can perform both surgery and chemotherapy or medical oncologists who can perform chemotherapy in transferred patients). We evaluated the compliance by completion rate of planned cycle and the dose reduction of the chemotherapeutic agents. The protocol of both chemotherapeutic agents was similar to the conventional study (ACTS-GC and CLASSIC trials) [12]. In this study, statistically significant differences were assessed using the chi-square test or the Fisher exact test for categorical variables. In addition, we used the t-test or the Mann-Whitney U-test for continuous variables. This study was approved by the Institutional Review Board (IRB) of each institution from where the data was collected (approval number: ED14245 at the institution of the principal investigator). Written informed consent was waived by the IRB.
In this study, we surveyed 2,006 patients at 31 institutions in Korea. Of these, we excluded 271 because of missing data and 646 who received chemotherapy other than TS-1 and XELOX. Finally, we examined 1,089 patients in this study.
First, we assessed patients' factors, including age (60 years), the extent of resection, ASA PS classifcation, and BMI (23 kg/m2), affecting the completion rate and dose reduction rate of chemotherapy (Table 1). The completion rate was statistically higher in patients younger than 60 years (76.8% vs. 57.5%, P < 0.001), with lower ASA PS classifcation (I: 74.4%; II: 62.8%; III: 60.0%, P = 0.001), and BMI higher than 23 kg/m2 (70.2% vs. 63.2%, P = 0.019). We observed no significant factors affecting the dose reduction rate.
Table 2 shows that the compliance depended on the subject of chemotherapy (surgical oncologists vs. medical oncologists). Of the 1,089 patients, 614 (56.4%) received chemotherapy from surgical oncologists and 475 (43.6%) from medical oncologists. We observed differences in age, T stage, and choice of chemotherapeutic regimen (TS-1 or XELOX) based on the subject of chemotherapy. When surgical oncologists were the subject of chemotherapy, the completion rate was relatively high (69.5% vs. 63.2%, P = 0.028) and the dose reduction rate was significantly low (17.4% vs. 22.3%, P = 0.035).
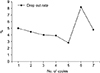
An analysis was conducted, whether the regimen was TS-1 or XELOX (Table 3). Patients who underwent XELOX chemotherapy (n = 232) were younger than those who received TS-1 (n = 857) and exhibited higher T and N stages (P < 0.001). In addition, although no difference was observed between the completion rate (65.8% vs. 70.3%, P = 0.206), the dose reduction rate was relatively high in the XELOX group (15.8% vs. 33.6%, P < 0.001). In all patients, the completion rate was 66.8% (n = 727) and the dose reduction rate was 19.5% (n = 213). Furthermore, the interruption rate of chemotherapy was the highest at the sixth cycle (8.2%) (Fig. 1).
Despite its decreasing incidence rate, gastric cancer is a major health concern worldwide because of its high mortality rate. In Korea and Japan, the incidence of early gastric cancer has been increasing compared to AGC because of the prevalence of mass screening programs and use of advanced diagnostic instruments [89]. However, AGC accounts for about 40% of total gastric cancer cases detected. According to the 2014 revised Japanese gastric cancer treatment guidelines [10], adjuvant chemotherapy should be administered in patients who were diagnosed with stages II–III gastric cancer. Several studies have been conducted to determine the efficacy of adjuvant chemotherapy in prolonging the survival of patients with gastric cancer [11121314], and several prospective randomized trials have demonstrated positive results [12315].
Reflecting the results of these studies, the insurance benefits of TS-1 monotherapy and XELOX therapy have been announced in Korea since 2013. Subsequently, chemotherapy, which was differently performed for each institution, has been standardized, and most Korean oncologists prescribe both regimens in adjuvant chemotherapy for patients with AGC. However, not many studies exist on patients' compliance with these 2 chemotherapeutic regimens. Improving the compliance is an essential issue because adjuvant chemotherapy aims to enhance the probability of curing cancer [4]. If chemotherapy is interrupted or an inappropriate dosage is administered for some reasons, it might affect the survival rate of patients. We defined the completion rate and dose reduction rate of planned chemotherapy as compliance and examined the factors that affected the compliance.
The factors affecting the compliance with adjuvant chemotherapy in gastric cancer are age, ASA PS classification, BMI, and the subject of chemotherapy. The compliance was lower in patients who were older than 60 years of age, had BMI < 23 kg/m2, and had higher ASA PS classification; however, sex and extent of resection did not affect the compliance. These findings imply that the nutritional status or performance of patients plays an important role in chemotherapy, and the oncologists should carefully check the condition of the patients before treatment. As the nutrition status, for example, is a factor that can be corrected, oncologists should treat this factor during chemotherapy. Since compliance itself is an independent prognostic factor of the survival rate [4], it facilitates in estimating the prognosis if factors affecting the compliance are considered in each patient before chemotherapy.
The interesting finding of this study is that it established a difference in the compliance depending on the subject of chemotherapy. To date, no study has compared the differences in the compliance between surgical oncologists and medical oncologists in adjuvant chemotherapy. Recently, the pros and cons of surgeons performing postoperative chemotherapy have been extensively debated, and no objective grounds for this have been suggested. In this study, when surgical oncologists led chemotherapy, the completion rate was higher and the dose reduction rate was lower than that of medical oncologists. Even though it was a simple univariate analysis, the actual compliance was better.
Various resections and anastomosis methods have been performed to treat stomach cancer; various post-gastrectomy complications may arise [16]. These complications are common causes of chemotherapy interruption and surgeons are most likely to cope with it. Surgeons understand patients' anatomy better and, hence, could promptly distinguish the complication. For example, when patients present with symptoms such as diarrhea or vomiting during chemotherapy, surgeons can assess easily whether these are side effects of chemotherapy or post-gastrectomy syndrome (dumping syndrome, mechanical obstruction). In addition, there will be advantageous effects of surgeons who understand the patient best in terms of rapport and emotional support. As surgeons could provide comprehensive care from the first surgery to the postoperative treatment, they can follow-up on patients more effectively.
However, these findings do not prove the superiority of surgical oncologists over medical oncologists when performing chemotherapy. It is only suggested that there is no reason to be occupied by medical oncologists anymore when selecting chemotherapeutic agents for adjuvant chemotherapy. Because the adjuvant chemotherapeutic regimen for gastrointestinal cancer has been standardized globally, it does not depend on the subject of chemotherapy, if administered using the same protocol. Regarding the continuity of treatment, surgical oncologists are advantageous to patients' compliance rather than medical oncologists. Hence, the results of this study suggest that surgeons should not only participate in surgery but also be actively involved in chemotherapy and general medical care of patients.
Regarding the compliance depending on the regimen of chemotherapy, patients who received chemotherapy with TS-1 were older, had a lower stage, and a lower dose reduction rate than patients who received XELOX chemotherapy. No statistical difference was observed between the completion rates (65.8% vs. 70.3%, P = 0.206); in addition, it was not significantly different from two prospective studies (ACTS-GC and CLASSIC trial). In Korea, both regimens have been established as a standard treatment after receiving the insurance benefits. However, no investigation has been conducted to assess which regimen is better or more efficient and which regimen is to be selected in each situation. In other words, each institution empirically selected chemotherapy from one of these two regimens, with no consideration of its effectiveness or compliance. Both TS-1 and XELOX regimens have different pharmacological characteristics and exhibit a partial difference in the antitumor effect [17]. Based on the compliance result, our SOF group is planning to check the long-term outcomes (recurrence and survival analysis) in patients who have received these 2 regimens in gastric cancer. This will be the cornerstone of making a new indication of 2 regimens in adjuvant chemotherapy.
At the sixth cycle, the interruption rate of chemotherapy was the highest (Fig. 1). Although several reasons exist for discontinuing chemotherapy, the major factor is a poor general condition caused by the accumulation of toxicity. Typically, most patients who experienced side effects of chemotherapy (asthenia, hand-foot syndrome, etc.) become tired and stop chemotherapy. However, it is not easy to precisely explain why the interruption rate is high in the sixth cycle. Thus, the analysis of toxicity, socioeconomic aspects, and psychological factors should be considered to understand this phenomenon.
This study has some limitations. First, it is a retrospective analysis that might have been biased by unrecognized factors. It was a follow-up of patients through medical records in 31 institutions, and the subjects of the survey were all surgeons, implying the possibility of a selection bias. Hence, further integrated studies with other departments (medical oncology) are required to conduct extensive studies, such as randomized controlled trial, for compliance. Second, the definition of the compliance in this study might have a problem. The compliance is defined which patients are performing well on the treatment plan established by doctors. In other words, compliance could be measured by several methods, as its definition is not precise. In this study, the compliance was determined by whether the planned cycle was completed or by the dose reduction rate. However, more points need to be considered in the compliance such as whether the cycle is delayed, whether schedules are changed, and when chemotherapy started after the operation. Finally, this study was a simple univariate analysis on compliance of adjuvant chemotherapy from a general perspective, and no variables were statistically significant in multivariate analysis.
In conclusion, this study identified the current state of adjuvant chemotherapy for patients with gastric cancer and examined factors that affected patients' compliance. Notably, this is the first study in Korea to compare and analyze the compliance of patients with gastric cancer according to the subject and regimen of chemotherapy. Hence, it is expected to play an important role as a base study for long-term outcomes and can be widely used as an evidence for securing the validity of surgeon-led chemotherapy.
Figures and Tables
ACKNOWLEDGEMENTS
The authors wish to thank Min Chan Kim, Jae-Seok Min, Chang Min Lee, Sung Il Choi, Kyung Won Seo, Do Joong Park, Yong Hae Baik, Myoung-Won Son, Won Hyuk Choi, Sungsoo Kim, Kyung Ho Pak, Min Gyu Kim, Joong-Min Park, Sang Ho Jeong, Moon-Soo Lee, Sungsoo Park, In-Hwan Kim, In-Kyu Kwon, Hyoung-Il Kim, Han Hong Lee, Sang-Il Lee, Hyundong Chae and all members of the Surgical Oncology Forum (SOF) study group for data sharing, discussion, and collaboration in this study.
References
1. Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007; 357:1810–1820.


2. Bang YJ, Kim YW, Yang HK, Chung HC, Park YK, Lee KH, et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012; 379:315–321.


3. Noh SH, Park SR, Yang HK, Chung HC, Chung IJ, Kim SW, et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014; 15:1389–1396.


4. Kim SJ, Kim YJ, Kim JH, Park DJ, Kim HH, Lee JS, et al. Safety, compliance, and predictive parameters for dosage modification in adjuvant S-1 chemotherapy for gastric cancer. Cancer Sci. 2013; 104:116–123.


5. Taylor SE, Lichtman RR, Wood JV. Compliance with chemotherapy among breast cancer patients. Health Psychol. 1984; 3:553–562.


6. Lonardi S, Sobrero A, Rosati G, Di Bartolomeo M, Ronzoni M, Aprile G, et al. Phase III trial comparing 3-6 months of adjuvant FOLFOX4/XELOX in stage II-III colon cancer: safety and compliance in the TOSCA trial. Ann Oncol. 2016; 27:2074–2081.

7. Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol. 2010; 17:3077–3079.


8. Information Committee of Korean Gastric Cancer Association. Korean Gastric Cancer Association Nationwide Survey on Gastric Cancer in 2014. J Gastric Cancer. 2016; 16:131–140.


9. Katai H, Ishikawa T, Akazawa K, Isobe Y, Miyashiro I, Oda I, et al. Five-year survival analysis of surgically resected gastric cancer cases in Japan: a retrospective analysis of more than 100,000 patients from the nationwide registry of the Japanese Gastric Cancer Association (2001-2007). Gastric Cancer. 2018; 21:144–154.


10. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017; 20:1–19.
11. Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC, Stemmermann GN, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001; 345:725–730.


12. Smalley SR, Benedetti JK, Haller DG, Hundahl SA, Estes NC, Ajani JA, et al. Updated analysis of SWOG-directed intergroup study 0116: a phase III trial of adjuvant radiochemotherapy versus observation after curative gastric cancer resection. J Clin Oncol. 2012; 30:2327–2333.



13. Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006; 355:11–20.


14. GASTRIC (Global Advanced/Adjuvant Stomach Tumor Research International Collaboration) Group. Paoletti X, Oba K, Burzykowski T, Michiels S, Ohashi Y, et al. Global Advanced/Adjuvant Stomach Tumor Research International Collaboration) Group, Paoletti X, Oba K, Burzykowski T, Michiels S, Ohashi Y, et al. Benefit of adjuvant chemotherapy for resectable gastric cancer: a meta-analysis. JAMA. 2010; 303:1729–1737.

15. Sasako M, Sakuramoto S, Katai H, Kinoshita T, Furukawa H, Yamaguchi T, et al. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol. 2011; 29:4387–4393.






 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download