Graphical Abstract
Malignant neoplasm is currently the most common cause of mortality in Korea.1 Most patients with end-stage cancer experience severe symptoms and general weakness. Radiotherapy, being minimally invasive and having limited acute toxicity, can alleviate the symptoms in certain regions of the body, accomplishing a palliative therapeutic role and improving the quality of life in these patients.
The role of radiotherapy in bone metastases, the most commonly presented metastatic area, is well established. In a randomized study (RTOG 97-14), two radiation schedules for bone metastasis were evaluated in terms of their effectiveness in pain relief. They observed that the extent of pain relief between multiple fraction (30 Gy/10 fractions) and single fraction (8 Gy/1 fraction) schedules was similar except that the re-treatment rate was higher in the single fraction group.2 In meta-analyses of randomized trials, the efficacy of single fraction schedules was also comparable to that of multiple fraction schedules in terms of pain relief.3 However, the schedule of 30 Gy/10 fractions is currently the most commonly performed clinical practice worldwide4 and Korea is not an exception.5 The question is: why would radiation oncologists still select multiple fraction schedules for treating bone metastases?
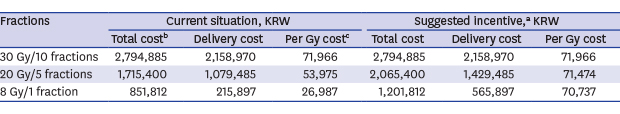
Radiation scheduling allows radiation oncologists to consider several patient's characteristics such as age, life expectancy, and general performance.6 However, as we know the Canadian cases, one thing cannot be ignored is the reimbursement system given by the physicians.7 The Korean National Health Insurance (KNHI) to provide equal opportunity for medical services to all national people using a restricted budget, only considers the fraction number and irradiation technique as the payment parameters for physicians. Noticeably, the extent of payment can be simulated according to the most popular radiation schedules for bone metastases (Table 1). For example, if a patient receives one course of 3D conformal radiotherapy in a tertiary hospital in 2019, the total hospital income of 8 Gy/1 fraction represents 30.5% of a 30 Gy/10 fractions schedule and 49.7% of a 20 Gy/5 fractions schedule. In addition, excluding the fixed preparation costs of radiotherapy planning, immobilization devices and shielding blocks, the actual cost per Gy of 8 Gy/1 fraction is 37.5% of the 30 Gy/10 fractions schedule and 50.0% of the 20 Gy/5 fractions schedule.
The cost-effectiveness of adopting single fraction schedules has been well validated in the simulation study of RTOG 97-14 despite allowing for the re-irradiation probability.8 Firstly, patients would require fewer visits to the hospital and save relevant indirect and partial direct medical costs. Secondly, KNHI could reduce the direct medical costs for radiotherapy. Lastly, the hospital's facilities could be more effectively used, decreasing machinery and manual loading in the ideal viewpoint. However, it is more practical aspect that the financial gain of hospital must decrease as much as the differences in the costs that KNHI saved at least, even though both uptime and labor per a fraction increased in single fraction schedule. It could not correspond the relative value scale, the basic policy of KNHI, to reimburse medical cost according to the actual workload. Furthermore, in cases that the hospital's facilities would be not fully utilized, there is no reason to seek decreasing the medical cost with effort.
I suggest assigning “fraction size” (dose per fraction) as a new parameter for radiotherapy KNHI reimbursement. The KNHI, for example, allocates KRW 70,000 as incentive for the application of radiation doses > 3 Gy. The total hospital income of 8 Gy/1 fraction would then represent 43.0% and 58.2% of the 30 Gy/10 fractions and the 20 Gy/5 fractions schedules, respectively. This effect would make the actual cost per Gy equivalent, regardless of the fraction schedule. As the popularization of intensity-modulated radiotherapy had been experienced after the change of reimbursement system,9 this compensation could motivate radiation oncologists to actively change their practice patterns in favor of the patients with bone metastases. Besides bone metastases, hypofractionated (decreasing fraction number through high fraction size) protocols combined with precise radiotherapy techniques could reduce treatment loadings for patients and medical costs in other definite settings.10,11 In addition, hypofractionated radiotherapy poses no moral concerns because radiation oncologists normally decide the total radiation dose based on the biological equivalent dose, which is positively affected by both fraction times and fraction size. We must find a point of compromise between reasonable incentives and regular application of hypofractionated radiotherapy, considering our low reimbursement system.
Another suggestion involves a long-term incentive feedback, proportional to the savings in costs derived from the changes in fraction schedules. As more radiation oncologists adopt the hypofractionated schedule for bone metastases, the KNHI budget will reduce costs in a proportion that could preferentially cover new technologies with promising clinical applications in the area of radiation oncology. For example, image-guided and breathing control radiotherapies could now be considered and publically performed in patients, improving the quality of radiotherapy.
Due to the above-mentioned financial limitations of the KNHI, medical practice charges are low and physicians compensate this situation using various methods. In our medical circle, if the conventional methods are more beneficial to physicians than the alternative methods, physicians generally tend to follow the former. This can be improved by warranting corresponsive reimbursements that should be proportional to the reduction in medical costs in every specific department. The payment offered for the application of alternative methods has to be more generous than that offered for the application of conventional methods and the long-term surplus KNHI funds obtained must be primarily allocated to the acquisition of new technology in the specific department that applied the alternative methods. In this way, patients can have access to the most convenient treatments and take advantage of new technologies or drugs earlier, at low economic costs.
In summary, considering fraction size as a new paradigm for radiotherapy payment can make cost-effective hypofractionated radiotherapies more widely used, depending only on the radiation oncologist's choice. Under active reimbursement policies, medical fields can search alternative methods to improve the cost-effectiveness of their practices.
Figures and Tables
Table 1
Cost comparison among three 3D conformal radiotherapy schedules in a Korean tertiary hospital in 2019

aThe supposed incentive case means that ₩70,000 per Gy over 3 Gy are provided as incentive; bTotal cost includes the fixed preparation cost (KRW 635,915) per schedule as well as the delivery cost of the actual fraction; cThe per Gy cost corresponds to the delivery cost divided by the total dose (Gy).
References
1. Shin HY, Lee JY, Song J, Lee S, Lee J, Lim B, et al. Cause-of-death statistics in the Republic of Korea, 2014. J Korean Med Assoc. 2016; 59(3):221–232.

2. Hartsell WF, Scott CB, Bruner DW, Scarantino CW, Ivker RA, Roach M 3rd, et al. Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst. 2005; 97(11):798–804.


3. Rich SE, Chow R, Raman S, Liang Zeng K, Lutz S, Lam H, et al. Update of the systematic review of palliative radiation therapy fractionation for bone metastases. Radiother Oncol. 2018; 126(3):547–557.


4. Fairchild A, Barnes E, Ghosh S, Ben-Josef E, Roos D, Hartsell W, et al. International patterns of practice in palliative radiotherapy for painful bone metastases: evidence-based practice? Int J Radiat Oncol Biol Phys. 2009; 75(5):1501–1510.


5. Chung Y, Koom WS, Ahn YC, Park HC, Kim HJ, Yoon SM, et al. A survey of patterns of practice on palliative radiation therapy for bone metastasis in Korea. J Cancer Res Clin Oncol. 2013; 139(12):2089–2096.


6. Liu Y, von Eyben R, Kidd EA. Consideration of patient and disease characteristics in selecting radiation regimens for treatment of bone metastases. Pract Radiat Oncol. 2017; 7(6):403–410.


7. Olson RA, Tiwana MS, Barnes M, Kiraly A, Beecham K, Miller S, et al. Use of single- versus multiple-fraction palliative radiation therapy for bone metastases: population-based analysis of 16,898 courses in a Canadian province. Int J Radiat Oncol Biol Phys. 2014; 89(5):1092–1099.


8. Konski A, James J, Hartsell W, Leibenhaut MH, Janjan N, Curran W, et al. Economic analysis of radiation therapy oncology group 97-14: multiple versus single fraction radiation treatment of patients with bone metastases. Am J Clin Oncol. 2009; 32(4):423–428.


9. Rim CH, Lee J, Kim WC, Yang D, Yoon WS, Koom WS, et al. A survey of radiation therapy utilization in Korea from 2010 to 2016: focusing on use of intensity-modulated radiation therapy. J Korean Med Sci. 2018; 33(9):e67.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download