This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
American Thyroid Association's guidelines (2015) recommend that papillary thyroid carcinomas (PTCs) ≤4 cm without extrathyroidal extension (ETE) and clinical lymph node metastasis (cLNM) can be treated by a unilateral procedure if a slightly higher risk of locoregional recurrence is accepted. The aim of the present study is to evaluate impact of minimal ETE (mETE) on locoregional recurrence in PTCs ≤4 cm without cLNM.
Methods
The medical records of patients who underwent thyroidectomy for PTC ≤4 cm between January 1, 2007 and December 31, 2013 were retrospectively reviewed. Patients who had PTC with gross ETE and/or cLNM were excluded.-Patients with papillary thyroid microcarcinoma (PTMC) without ETE (group I; n=381) were compared with three other groups of patients: PTC 1–4 cm without ETE (group II; n=150); PTC ≤1 cm with mETE (group III; n=186); and PTC 1–4 cm with mETE (group IV; n=121). Mean follow-up period was 72.2±26.4 months.
Results
Multiplicity, bilaterality, LNM, and total thyroidectomy were more common in group III and IV. Five-year disease-free survival (DFS) was 100%, 97.9%, 95.9%, and 94.9% in group I, II, III, and IV, respectively. DFS rates were significantly higher in group I compared to the other groups (P<0.01). There were no significant differences among group II, III, and IV.
Conclusion
Compared to PTMC without ETE, mETE in PTC ≤4 cm without cLNM may be associated with more aggressive biological behavior and increased risk of recurrence, although the increments may be relatively small.
Keywords: Papillary thyroid carcinoma, Extrathyroidal extension, Lymph node metastasis, Disease-free survival
INTRODUCTION
Surgery is an important element in multidisciplinary treatment for papillary thyroid carcinoma (PTC), the most common differentiated thyroid carcinoma (DTC). The operation should be harmonized with the overall treatment strategy and follow-up plan. In recent decades, the paradigm for DTC management has changed considerably. Total thyroidectomy to facilitate radioactive iodine ablation or diagnostic whole-body scan (WBS) is losing favor. In addition, more patients are concerned about lower quality of life by potential complications and the life-long hormone therapy which accompanies total thyroidectomy.
For a long time, a bilateral procedure such as near-total or total thyroidectomy was recommended for PTC larger than 1 cm in diameter with or without evidence of locoregional or distant metastases (
1). In 2015, the American Thyroid Association (ATA) revised their recommendations to strongly suggest that the initial surgical procedure for PTC measuring 4 cm or less without extrathyroidal extension (ETE) and clinical lymph node metastasis (cLNM) can be either a bilateral or a unilateral procedure (
2). The relatively low locoregional recurrence rate of PTCs measuring 4 cm or less without ETE and cLNM is one of the primary reasons for updating the recommendation for surgery.
In addition, in 2017, the American Joint Committee on Cancer changed the T3b definition because of reported difficulties with accurate diagnosis and a lack of obvious prognostic significance related to minimal ETE (mETE). Currently, T3b is defined as a tumor of any size with gross ETE invading only strap muscles, excluding mETE involving peri-thyroidal adipose tissue, strap muscles, or small vascular structures (
3).
The aim of the present study is to evaluate the impact of mETE on locoregional recurrence in PTCs measuring 4 cm or less without cLNM.
MATERIALS AND METHODS
The medical records of patients who underwent thyroidectomy for PTC measuring 4 cm or less, from January 1, 2007 to December 31, 2013, were retrospectively reviewed. Prophylactic central neck dissection was routinely performed, unilaterally for lobectomy and bilaterally for total thyroidectomy. Patients diagnosed with PTC with gross ETE and/or cLNM were excluded from this study. Clinical LNM was defined as no evidence of LNM on preoperative physical examination, image studies and intraoperative palpation. ATA strongly recommends lobectomy for papillary thyroid microcarcinomas (PTMC) without ETE because of its known lowest risk of recurrence. In this study, patients with PTMC without ETE were set as group I (n=381) and compared with patients with PTC measuring 1–4 cm without ETE (group II; n=150); patients with PTC measuring ≤1 cm with mETE (group III; n=186); and patients with PTC measuring 1–4 cm with mETE (group IV; n=121). Mean follow-up period was 72.2±26.4 months. The SPSS 19.0KO for Microsoft Windows (IBM Corp., Armonk, NY, USA) was used for statistical analyses with and P<0.05 was considered statistically significant. The Kaplan-Meier method and log rank test were used to analyze time-dependent variables. Multivariate analysis was performed by logistic regression model.
RESULTS
1. Characteristics of patients and tumors
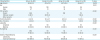
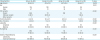
Age and sex distributions were comparable among study groups. Group III and IV (tumors with mETE) tended to show multiplicity/bilaterality and were more frequently treated by total thyroidectomy (
Table 1). Follicular variant of PTC was more common in group II (21.3%) and IV (5.8%) compared to group I (3.7%) (P<0.001).
Table 1
Characteristics of patients and tumors
|
Characteristics |
Group I (n=381) |
Group II (n=150) |
Group III (n=186) |
Group IV (n=121) |
P value |
|
Age (mean) |
48.9±11.6 |
47.4±13.0 |
48.7±10.6 |
49.6±11.7 |
0.429 |
|
Sex |
|
|
|
|
0.513 |
|
Female |
314 |
129 |
151 |
96 |
|
Male |
67 |
21 |
35 |
25 |
|
PTC variants |
|
|
|
|
<0.001 |
|
Classic |
366 |
111 |
186 |
113 |
|
Follicular variant |
14 (3.7) |
32 (21.3) |
- |
7 (5.8) |
|
Other variants |
1 |
7 |
- |
1 |
|
Tumor size (mm) |
4.9±1.9 |
14.5±5.7 |
6.2±1.6 |
14.3±5.3 |
<0.001 |
|
No. of tumors |
1.4±0.9 |
1.5±1.3 |
1.7±1.1 |
1.8±0.1 |
0.005 |
|
Laterality |
|
|
|
|
<0.001 |
|
Unilateral |
343 |
132 |
143 |
93 |
|
Bilateral |
38 (10.0) |
18 (12.0) |
43 (23.1) |
28 (23.1) |
|
Multiplicity |
|
|
|
|
<0.001 |
|
− |
284 |
110 |
114 |
71 |
|
+ |
97 (25.5) |
40 (26.7) |
72 (38.7) |
50 (41.3) |
|
Extent of thyroidectomy |
|
|
|
|
<0.001 |
|
Lobectomy |
116 |
10 |
28 |
7 |
|
Total thyroidectomy |
265 (69.9) |
140 (93.3) |
158 (84.9) |
114 (94.2) |

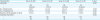
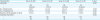
No patients showed evidences of cLNM preoperatively and intraoperatively. However, pathologically proven lymph node (LN) micrometastases were relatively common (11.3%–24.0%) and more frequent in group III and IV, compared to group I and II. The number of extracted LNs and metastatic LNs, and the maximum size of metastatic LNs were also higher in group III and IV, compared to the other groups (
Table 2).
Table 2
Status of LNs and underlying thyroids
|
Characteristics |
Group I (n=381) |
Group II (n=150) |
Group III (n=186) |
Group IV (n=121) |
P value |
|
LNM (pN1) |
|
|
|
|
0.001 |
|
− |
333 |
133 |
146 |
92 |
|
+ |
48 (12.6) |
17 (11.3) |
40 (21.5) |
29 (24.0) |
|
No. of Extracted LNs |
3.8±3.7 |
3.4±5.0 |
4.2±4.5 |
4.0±4.6 |
0.005 |
|
No. of metastatic LNs |
0.2±0.8 |
0.2±0.8 |
0.5±1.5 |
0.7±2.1 |
0.001 |
|
Maximum size of metastatic LN (mm) |
0.1±0.4 |
0.1±0.5 |
0.2±0.6 |
0.3±0.7 |
<0.001 |
|
Hashimoto thyroiditis |
|
|
|
|
0.729 |
|
− |
297 |
120 |
148 |
100 |
|
+ |
84 |
30 |
38 |
21 |

2. Recurrence and mortality
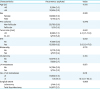
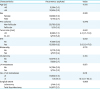
Short-term locoregional recurrences occurred relatively infrequently as follows: group I, none; group II, four; group III, seven; and group IV, six (P=0.001). Recurrences developed as a LNM in the ipsilateral lateral neck or as soft tissue masses in the ipsilateral operative bed (
Table 3). Although tumor size, ETE, and number of metastatic LNs appeared to associated with recurrence by univariate analysis, none were categorized as significant independent prognostic factors by multivariate analysis (
Table 4).
Table 3
Patterns of disease recurrences

|
Pattern of recurrences |
Group I (n=381) |
Group II (n=150) |
Group III (n=186) |
Group IV (n=121) |
P value |
|
Op bed |
|
1 |
1 |
2 |
|
|
Lateral neck LNs |
|
3 |
6 |
4 |
|
|
Total |
0 |
4 (2.7) |
7 (3.8) |
6 (5.0) |
0.001 |

Table 4
Risk factors for recurrence
|
Characteristics |
Recurrence: yes/total |
Value |
|
Age (yr) |
|
0.552 |
|
<45 |
5/304 (1.6) |
|
≥45 |
12/534 (2.2) |
|
Sex |
|
0.522 |
|
Female |
13/690 (1.9) |
|
Male |
4/148 (2.7) |
|
PTC variants |
|
0.940 |
|
Non-follicular |
52/785 (6.6) |
|
Follicular |
1/53 (1.9) |
|
Tumor size (mm) |
|
0.001 |
|
≤10 |
8/666 (1.2) |
4.5 (1.7–12.0) |
|
10–40 |
9/172 (5.2) |
|
|
ETE |
|
0.001 |
|
No |
4/529 (0.8) |
|
|
Yes |
13/309 (4.2) |
5.8 (1.9–17.8) |
|
Bilaterality |
|
0.772 |
|
No |
14/711 (2.0) |
|
Yes |
3/127 (2.4) |
|
Multiplicity |
|
0.355 |
|
No |
10/579 (1.7) |
|
Yes |
7/259 (2.7) |
|
LN metastases |
|
0.851 |
|
No |
14/704 (2.0) |
|
Yes |
3/134 (2.2) |
|
No. of LN metastases |
|
0.011 |
|
≤5 |
16/832 (1.9) |
|
|
>5 |
1/6 (16.7) |
10.2 (1.1–92.4) |
|
Surgical extent |
|
0.869 |
|
Lobectomy |
3/161 (1.9) |
|
Total thyroidectomy |
14/677 (2.1) |

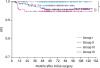
Respective five- and ten-year disease-free survival (DFS) was as follows: group I, 100% and 100%; group II, 97.9% and 96.2%; group III, 94.9%, and 95.9%; and group IV, 94.9% and 94.9% (P<0.001) (
Fig. 1). DFS rates were significantly higher in group I compared to the other groups (P<0.01) , but there were no significant differences among groups II, III, and IV.
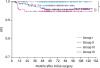 | Fig. 1
Comparison of DFS of patients in control, group I, II, and III. Group I, PTC ≤1 cm without ETE; group II, 1–4 cm without ETE; group III, ≤1 cm with mETE; group IV, 1–4 cm with mETE.
DFS = disease free survival; PTC = papillary thyroid carcinoma; ETE = extrathyroidal extension; mETE = minimal extrathyroidal extension.
*P<0.05; †Statistically not significant.

|
Nine patients died within 29.2±23.0 months of thyroid surgery: Group I, one death; group II, three deaths; group III, two deaths; and group IV, three deaths. The causes of death were pneumonia, cerebrovascular accident, and comorbid advanced cancers such as breast cancer, leukemia, and lymphoma. No patients died of thyroid carcinoma.
DISCUSSION
The 2015 ATA's guidelines extend the indication of thyroid lobectomy for patients who have PTC measuring 4 cm or less without ETE and cLNM. This takes into account the potential decrease in quality of life following total thyroidectomy and the relatively low locoregional recurrence rate (
2). In addition, difficulties in accurate diagnosis and a lack of obvious prognostic significance related with mETE led to the new definition of T3b in 8th edition of TNM staging in 2017. In the present study, we evaluate the impact of mETE on locoregional recurrence in PTCs measuring 4 cm or less without cLNM.
Previously, ATA guidelines recommended total thyroidectomy as the primary initial surgical treatment option for nearly all patients with DTCs greater than 1 cm, regardless of locoregional or distant metastases (
1). Bilimoria et al. (
4) provided strong supporting evidences to demonstrate a slight but significantly higher 10-year relative overall survival for total thyroidectomy compared to lobectomy. However, this report was recently re-evaluated and it was noted that its findings changed when variables related to the complexity and severity of illness were adjusted. Recent studies also failed to demonstrate a significant difference in survival when comparing total thyroidectomy with lobectomy (
567). In addition, the paradigm for DTC management has recently changed. thyroidectomy to facilitate RIA or WBS is becoming outmoded as patients endeavor to avoid potential complications and the burden of life-long hormone medication. Complication rate of total thyroidectomy for cancer is relatively high, at 7.5% on average even by high-volume surgeons (>100 cases/year) as Sosa et al. reported through a nationwide study (
8). Based on these changes, For these reason, the ATA recently revised its recommendations for initial surgical extent for patients who have PTC. In 2015, new guidelines strongly recommended that the initial surgical procedure should be a thyroid lobectomy for PTMC and can be a lobectomy for PTC measuring 4 cm or less unless there are ETE, cLNM, and clear indications to remove the contralateral lobe (
2). New ATA guidelines however did not suggest any recommendations for PTC measuring 4 cm or less with mETE.
In 2017, because of difficulties with accurate diagnosis and a lack of obvious prognostic significance related to mETE, the American Joint Committee on Cancer introduced a new definition for T3b in the 8th edition of TNM staging. Now, T3b is defined as a tumor of any size with gross ETE invading only strap muscles, excluding mETE involving peri-thyroidal adipose tissue, strap muscles, or small vascular structures (
3). In the For this same reason, patients who have PTC measuring 4 cm or less with mETE need to be evaluated.
No patients enrolled in the present study showed any evidences of cLNM preoperatively and intraoperatively. Prophylactic central neck dissections were performed routinely, unilaterally for lobectomy and bilaterally for total thyroidectomy. Pathologically proven LN micrometastases were relatively common (11.3%–24.0%). Recently the ATA redefined the risk of recurrence regarding LNMs in PTC (
9). Nodal metastases were newly stratified into small-volume microscopic disease and clinically apparent macroscopic disease. Not more than 5 pN1 micrometastases (<0.2 cm in largest dimension) are newly classified as lower risk N1 disease (<5% risk of recurrence). In the present study, presence or absence of LNM did not associate with recurrence. However, large number (>5) of LNMs seemed to associate with recurrence but statistical significance is unclear because of small sample size.
The prognosis of low-risk PTC patients in relation to primary tumor size was has been reported by Ito et al. (
10). They classified patients who had PTC without significant ETE and cLNM into 3 groups: tumor ≤2 cm; 2–4 cm; >4 cm. For each group, 10-year recurrence rates were 0.3%, 1.3%, and 1.9% for the thyroid; 1.9%, 4.6%, and 8.1% for LNs; 0.4%, 1.6%, and 3.4% for distant organs, respectively. Based on these results, they suggest that PTC larger than 2 cm have more aggressive biological characteristics than smaller ones but they questioned whether extensive surgery is mandatory for these relatively low-risk PTC patients because of very low incidence of distant recurrence and cancer-specific death. In the present study, we observed similar findings. During the study period, there were was no cancer-specific mortality and a very low rate of recurrence (17/838, 0.2%, respectively). The respective five- and ten-year DFS rates wasere 100% and 100% for group I, 97.9% and 96.2% for group II, 94.9% and 95.9% for group III, and 94.9% and 94.9% for group IV. Although DFS rates were significantly lower in group II, III, and IV compared to group I (PTMC without ETE and cLNM), the differences between groups are relatively small, 5% at most. There were no significant differences among group II, III, and IV.
The present study has several limitations including the limited sample size and a follow-up period. The rates of recurrence in this study may be associated with total thyroidectomy in groups II, III, and IV. The clinical implication of follicular variant of PTC could not be properly evaluated because of its relatively low rate of diagnosis. Further studies are needed to address these issues.
In conclusion, compared to PTMC without ETE, mETE in PTC ≤4 cm measuring 4 cm or less without cLNM may be associated with more aggressive biological behavior and increased risk of recurrence. However, the increments of increase may be relatively small.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download